Impact of Homelessness on Access to Primary Care
Chapter 1: Introduction
Homelessness is an issue that affects most of the developing nations due to increased urbanization and economic hardships because of lack of employment and increased cost of living. Ideally, there are two types of homelessness; absolute and relative homelessness. According to the United Nations, as cited by Hwang (2001), absolute homelessness is a condition in which people without shelter sleep outdoors in abandoned buildings, vehicles, and other places not fit for human habitation. On the other hand, relative homelessness is a condition in which people have a physical shelter that does not meet the basic criteria of safety and health; this entails personal safety and affordability, protection from elements of safe water and sanitation, and safe tenure (Hwang, 2001). Nevertheless, homeless people experience high mortality rates and poor health compared to the general population (Hulchanski, Campsie, Paradis, Hwang, & Chau, 2009). Moreover, homeless people often face difficulties in obtaining health care and other social services. This can be attributed to the fact they are often excluded from broad-based government health initiatives. Moreover, Hulchanski et al. (2009) attributed to the lack of recognition of homeless people to the address and telephone-based census surveys. Similarly, Hulchanski et al. (2009) noted that even if the census reaches the homeless population, it fails to capture or address their unique circumstance. In this regard, this paper investigates the barriers to health care within the homeless population in UK with a focus on the London region and outlines the past and present initiatives to address the barriers. Additionally, for those who are working on healthcare dissertations, seek out healthcare dissertation help to get the most valuable insights and support in navigating this complex topic.
Background Information

Homeless people have got challenges associated with accessing healthcare with their conditions. Most of the time, they will seek medical attention when they are entirely sick or when well-wishers have assisted them. They are a threat to the healthcare sector as they can be the source of the challenges due to lack of proper attention (Hwang, 2001). Most governments have not set up a mechanism through which homeless people can access healthcare services with ease. With the increased cost required to access primary healthcare services, homeless people find it difficult, and they do not seek medical attention unless they are assisted.
Homelessness has directly impacted society's general well-being because it contributes to the overall access to adequate healthcare services. Homeless people do not maintain good health; they do not have medical insurance to care for them. These factors may be carriers of disease that may affect the general community in which they are found. Due to lack of proper care, they are susceptible to disease and can be getting admitted to hospitals overwhelming the existing healthcare resources (Hulchanski et al. 2009). Due to the terrible conditions they stay in, they are most likely frequently exposed to diseases, resulting in the need for primary healthcare services, requiring many resources. Despite the risk that homeless people face of contracting diseases, they cannot access quality primary healthcare and medical insurance covers.
Primary healthcare provides integrated, accessible health care services by medical professionals responsible for taking care of individuals' health care needs, developing a good relationship with patients, and undertaking health care practices based on communal and family needs. Access to primary healthcare can positively be associated with the increased healthcare resources to lower mortality rates and improve quality of living amongst individuals and the community (Kandor et al. 2011). There is a significant limitation on the access to primary healthcare services due to the rise of chronic conditions and other diseases in communities. Evidence indicates that homeless people seek primary healthcare services frequently compared to the rest of the population. Due to the inequalities that they face and the poor living standards, they are susceptible to diseases.
The significant inequalities amongst homeless people in accessing primary healthcare services have impacted the way countries are approaching their planning and accommodating them to ensure they do not act as carriers of dangerous diseases. Countries are taking seriously homeless people as they are trying to standardize the mortality rates. Homeless people tend to have higher rates of mortality when compared to the rest of the population (Hulchanski et al. 2009). Due to the barriers that homeless people face to access healthcare services, the Inverse Care Law applies in their case as they need increased primary care demand. Dig deeper into Adolescent Eating Disorders: A Critical Review with our selection of articles.
There is a higher likelihood that homeless people would fall sick at any specific time than the rest of the population. When they have limitations that pars them from accessing quality healthcare, they are likely to face an increased number of diseases. To address the disparities that exist, healthcare professionals and institutions develop a special approach that ensures homeless people access primary healthcare (Kandor et al. 2011). Medical institutions and centres put up special services directly aimed at providing access to readily available healthcare services, and they can get them at a specific point. Homeless people receive support in the institutions and centres, till when they get well. Some institutions have come up with programs where homeless people are permanently housed.
The delayed access to healthcare services that result in late diagnosis and treatment of homeless people due to barriers has worsened the homeless people's healthcare conditions. The fact that homeless people are likely to experience increased accidents and emergency cases higher by 60% compared to the rest of the population requires special attention. Abuse of drugs and alcohol that may arise due to economic stress may require that the people require primary health care and further specialized treatment (Zlotnick et al. 2013). The condition and needs that arise due to homelessness indicate how the primary healthcare system has been exposed due to homelessness.
Different reasons have led to homeless people not having access to primary healthcare. However, there is an impact that homelessness has had on accessing primary healthcare. Because they live under poor living conditions, they are constantly exposed to diseases, accidents, and other emergencies (Kandor et al. 2011). Their frequent need for primary healthcare facilities has led governments, healthcare professionals, institutions, and centres to come up with different ways to address the rising problems. The resources used to ensure the homeless people access primary healthcare could have helped improve the state of healthcare systems in a country.
Chapter 2: Literature Review
Homelessness is a critical social issue affecting a larger percentage of urban inhabitants around the world (Kandor et al. 2011). Ideally, homeless people experience poor health and disproportionate rates of chronic and acute health issues, including concurrent substance use and mental health disorders (Kandor et al. 2011). Nevertheless, despite their increased need and urgency for health care, the homeless people face many barriers to primary health (Hwang et al. 2010). Moreover, the homeless population has a lot of unmet health care needs compared to the general population.
According to Zlotnick, Zerger, and Wolfe (2013), the number of homeless people increased during the 1980s due to the cuts experienced in housing and other social services, deteriorating economy, and the deinstitutionalization experienced in the country. Moreover, Zlotnick et al. (2013) pointed out that gentrification contributed to the loss of low-cost dwellings resulting in a reduction of cheap housing for individuals faced with homelessness, and displacing many poor people thereby increasing the number of homeless people. Homelessness has some effects on the physical health of an individual. Zlotnick et al. (2013) noted that there were higher rates of respiratory illness, hypertension, HIV, infestation, and tuberculosis among other diseases in homeless people compared to the general population. Similarly, the Durham County Community Health Assessment report (2011) pointed out that exposure to stress for a long time can have negative effects on the health of an individual. The further report outlines that depression, asthma, obesity, and heart diseases are among the common problems facing individuals with prolonged exposure to stress. Ideally, homeless people are faced with high levels of poverty and economic difficulties, which are the major causes of stress in the life of an individual; as such, they are more susceptible to stress-related health conditions. Moreover, reports continue to show similar trends of disparities in physical health between homeless and housed people in samples collected from jailed inmates, homeless adults living in shelters, patients using the clinic, and HIV positive individuals.
According to World Health Organization as cited by Campbell, O’Neill, Gibson and Thurston (2015), primary health care can be defined as “essential healthcare, based on practical, scientifically sound and socially acceptable methods and technology, made universally available to individuals and families in the community through their full participation and at a cost that the community and country can afford to maintain at every stage of their development in the spirit of self-reliance and self-determination” (p.2). Similarly, primary healthcare refers to the first point of contact to the healthcare system. In this regard, this paper will discuss barriers to primary health care among homeless people based on the above two definitions.
Most of the studies on access to primary health care among the homeless population point out to lack of a health insurance as the main barrier to primary health (Kandor et al. 2011). Moreover, lack of knowledge on where to obtain primary health care, chronic homelessness, lack of transport, long waiting times, lack of childcare, and feeling of discrimination are among the barriers to primary health care among the homeless population in Durham (Durham County Community Health Assessment, 2011). Moreover, Durham county report further points out that affordability, language barriers, and individual negative perception are among the challenges facing homeless people.
In addition, homelessness coupled with poverty contributes to ill health through presenting unique constraints to access to health services and self-care. Similarly, poverty and homelessness increase the exposure to parasites and communicable diseases since most of this population live in open and crowded places. For instance, in case of an outbreak of a condition that is communicable, this population can easily infect each other due to poor structures and unhealthy living conditions. Zlotnick et al. (2013) noted that lack of permanent homes complicates treatment adherence and self-care of homeless people. They cited the inability to store medicine or meet refrigeration requirements make it hard to adhere to mediation or meet self-care requirements. Similarly, competing needs such as employment and food coupled with limits on shelter stay interfere with the consistent administration of medication and follow up visits to healthcare facilities. Similarly, Campbell, O’Neill, Gibson, and Thurston (2015) pointed out that lack of access to reliable and regular primary health, poor health status, and lack of specialized health services serves as significant barriers to primary health care to homeless people in Calgary.
Mental health problems are another factor that contributes to the lack of access to primary care. According to Fazel, Khosla, Doll, and Geddes (2008), the prevalence of mental health problems is high in homeless people compared to the general population and the more severe the homelessness, the more severe the mental health problem. However, despite the high rates of mental health problems in the homeless population, less than one-third of the population receive medication (Canavan et al., 2012). As pointed out above, lack of medical insurance serves as one of the major barriers to primary care. The lack of medical insurance can be attributed to various factor one of them being lack of permanent address, which is one of the vital requirement during the registration with a health care system in many countries including Canada (Anderson, Baptista, Wolf, Edgar, Benjaminsen, et al. 2006). Consequently, this forces homeless people to attempt accessing primary care through emergency services, which limits the opportunity of receiving quality health care services through inappropriate treatment and care (Hwang, Tolomiczenko, Kouyoumdjian & Garner, 2005). Moreover, Anderson et al. (2006) noted that entitlement to health care does not always to access to primary care for homeless people. This implies that there are systematic of structural factors that limit the access of homeless people to primary care. For instance, The Feansta Annual Report (2006) outlined that limited accessibility of primary care to homeless people is due to factors such inflexible appointment procedures, opening hours, and location of the healthcare facilities. In addition, Busch-Geertsema, Edgar, Sullivan, and Pleace (2010) pointed out that homeless people experience barriers and difficulties or unwillingness in health services to accommodate their complex and various health needs. The attitudes and unwillingness in health services to accommodate the health need of homeless people scare them aware from seeking primary healthcare services. Moreover, financial constraint serves as another major factor in preventing homeless people from accessing primary care. Nevertheless, it is important to point out the lack of recognition in national affairs such as policies that highlight the plight of homeless people with regards to health care. Ideally, the majority of the policies focus on patients with mental health problems and minority communities.
As a result, there is a need to formulate policies that focus on the homeless people specifically and their diverse healthcare needs. In particular, it is important to formulate policies that address the homeless population separately other than generalizing the population with other minorities like the poor in the society. Despite the homeless being poor, their level of poverty cannot be compared to that of other minority groups in the society. This is because the absolute homeless people live in a unique environment made of complex challenges and factors that make their hardship unique. Therefore, it is important to understand their environment first and other factors that influence their lives before formulating policies that aim to address their complex healthcare needs. This can help formulate effective policies that are successful in addressing the healthcare needs of the homeless people. The research will address the impact of homelessness on access to primary care.

Chapter 3: Methodology
The following are the research methodology process that was used in the study.
Research Approach
The study's research approach falls under the deductive analysis as various pre-set questions explain the targeted audience. Appendix A will illustrate the questionnaire targeted for the specific audience.
Research Strategy
In the research, the strategy used falls under the analysis study category. Goal: To investigate the benefits of digitalization in attaining strategic organizational goals.
Method:
1. hypothesis formulation
2. use of the Stratified Sampling Method to choose the targeted group.
3. Make the questions
4. Data gathering, examine and explain respondent questionnaires
5. test the hypotheses on gathered information
Examples of analysis: Positivism, Deductive, Explanatory, and Qualitative
Research Choice
The research is a quantitative study, and in regards to its objective, it is a descriptive study.
The quantitative analysis centres on authenticating hypotheses (deductive) or noticing a routine (inductive) using massive data. This analysis investigates the impact of homelessness on access to primary care through a large questionnaire distribution.
Time Series
The research uses a cross-sectional analysis that takes a few weeks or months to gather the information needed. The study also uses the self-administered questionnaire where the targeted respondents solely answer the questions and return the questionnaire within the scheduled time.
Data (Primary/Secondary)
For the essential data gathering, the method used is by issuing questionnaires to the respondents. The exercise will be conducted online by giving questionnaires to the respondents an activity called a self-administered questionnaire. A Stratified Sampling method will be used as a way of distributing the questionnaires online. The respondents for the questionnaires were randomly picked from a poll list from organizations worldwide. The cantered reason for this poll is how homelessness impacts access to primary care. I finally used thirty respondents for the analysis who represented both homeless people, government agencies and healthcare organizations.
For secondary statistics gathering, I will gather information by use of past literature review researchers. I will obtain the information from various books and academic sources like Emerald Insights, Directory of Open Access Journals (DOAJ), Science Direct, and ProQuest. The range from the literature overview mainly focuses on the impact of homelessness on access to primary care. The information gathered from the literature review will be put in further analysis through critical research to guarantee the data's viability and credibility.
Instrumentation/Questionnaire
I measured the questionnaire that extended to analyse each information towards establishing the impact of homelessness on access to primary care. When calculating the determinants, I used a five-point Likert scale method. Every statement I interpreted in five points. In which 5 points meant "strongly agree," 4 points as "agree," 3 points denoted," neither," 2 points were given as "disagree," and 1 point was given as "Strongly disagree."
Perceived Impacts
The method was embraced to see the perceived impact of homelessness on access to primary care. The respondents read out the technique, which contained 8 statements, to know whether they agree or disagree with the statements. All the eight opinions are positive.
Homelessness Factors
I used the method to see the homelessness factors that affect access to primary health care. The technique consists of three categories with seven statements. The respondents read the statements to know whether they agree or disagree with the ideas. All the thirteen statements from the scale turned out positive.
Homelessness impacts
I used this method to see the general impact of homelessness on access to primary care. The technique has three categories with 15 statements that the respondents read to know whether they agree or disagree with the ideas. All five views turned out to be positive.
The role of health care facilities on homelessness
I used the method to look at the role healthcare facilities in addressing homelessness. The instrument had six statements. The respondents read the statements to know whether they disagree or agree with them. All six statements turned out positive.
Source of Data Collection
For first-hand information, I will gather the data by issuing online questionnaires to the respondents. I gathered secondary information from past researches and literature reviews. I will obtain information from various academic sources like ProQuest, EBSCO, Science Direct, Emerald Insights, and Directory of Open Access Journals (DOAJ). The literature scope overview mainly focused on the following determinants: perceived impacts, homelessness factors, and homelessness impacts, and the role of health care facilities on homelessness. To ensure the information is accessible and valid, I will subject data from the literature review to further primary research.
Sampling
The sampling method that will be used is approach employees in different healthcare facilities, homelessness people and workers of social services government agencies. The sampling will be based on different industries. The study used a stratified sampling methodology. The number of participants that will be approached is 30 who will be approached. The Margin of error = 10% where the Confident Level= 95%.
Ethical Consideration
The research took into consideration of the ethical issues that could rise and addressed them even before the beginning of the study. However, the ethical standards were maintained all through the study and even after the completion of the study. In the cause of the study, the information collected was treated with privacy and confidentiality with all respondents respected equally with the information that was obtained. Before conducting a survey, it was agreed that the consent for all the participants is first obtained before any form of engagement. The reason for the study was explained to ensure proper understanding. Therefore, because of the ethical observations, there was not ethical breach that was observed on the part of the researcher and the respondents either directly or indirectly. To ensure that the results reflected the true findings of the study, there was no distortion or misrepresentation of data. Respondents were required to be truthful and honest with the responses they were giving. They also cooperated without any form of conditions.
Data Processing
Processing of data took place using excel and they were analysed based on the group. The results generated were recorded and they were processed without any alteration. It is from these that the data was obtained for further analysis and determining of the findings.
Data Analysis
The analysis of data was undertaken using excel and the results presented using tables and charts to ensure that interpretation of the results has been made easy. To ensure validity and relevancy the sampling that took place was big enough and from those employees of different organizations that understood the importance of the study. Both inferential and descriptive statistics was used.
Conclusion
This research study aims to understand the impact of homelessness on access to primary care. Few studies had been conducted in Chapter Two: Literature Review had found the significant impact of homelessness on access to primary care. Furthermore, this research study also investigated how these determinants (perceived impacts, homelessness factors, and homelessness impacts, and the role of health care facilities on homelessness) effects on the primary healthcare. In addition, despite of looking into the determinants of the variable, demographic is also part of the research contents. Although, initially the respondents were included in the research framework and being removed in the later research on going. Due to the sampling methodology used, specific demographic profile such as working industry, employment status and working experience need to be included as part of the research design.
Chapter 4: Findings and Analysis
While 97% of the English general population registered are general practitioners, from our study of 83.3% of sole homeless accommodation, unrevealed homeless people of 89%, and rough sleepers recorded at 65.5%. With all other factors controlled, less than half of the odds reported as rough sleepers. The analysis was put in consideration with a general practitioner of single homeless people with shelter. Several factors influence secondary care utilization. In this analysis, the best foreteller of secondary care usage was a previous denial of general practitioner and a dentist registration. We anticipated finding poor access to essential services and care could relate to higher secondary care usage rates. The rejection of dentist and general practitioner registration had a relationship with the elevated turnout from A&E medical corporation. The collaboration was lessened by accommodating the health status, although this analysis might seem insufficient to detect any variation.
From hospital admissions, we gathered apparent collaboration but not according to our expectations. Previous assessments have discovered that the homeless areas' admission rates are high compared to the general population. My analysis reached the homeless population with the admission rates and found that those recently refused in the general practitioners and dentist registration had low chances of being accepted to the hospital (OR 0.67, 95% CI 0.49–0.91). It was the opposite of our expectations, and gatekeeping had to explain the general practitioners' responsibility in England. I did not expect to find that the high ambulance usage rates were associated with homeless health service utilization (OR 1.62, 95% CI 1.14–2.31). The results gathered need further assessment, but it might conclude that the neediest homeless people are likely to sort out for homeless health services and emergency care.
I tested the general practitioner's responsibility as a gatekeeper by using the mediation model to know if denial of GP/dental registration and general practitioner registration mediated a relationship on secondary care utilization and sleeping status. I did not find any crucial mediating impacts. The findings might have insufficient power to note such defects of unequal confounding. The results might also be that there were no such effects and need for further confirmation by several detailed street people's analyses.
Facts on this topic
Home care usage for homeless people in western nations is mainly related to high unplanned care and emergency usage, resulting in poor primary care access. For example, with an estimation, the street people in the United Kingdom utilize A&E an average of six times higher than the general public. Homeless people in the United Kingdom have been experiencing challenges accessing primary health care. Their challenges include having a hard time registering with a general practitioner because they often move between areas and lack fixed addresses. Other challenges include transport inaccessibility, making it hard to find healthcare services that are far, and having a chaotic lifestyle, making it challenging to keep an appointment. However, there is no much information on how various types of homeless can affect usage of healthcare methods or what other elements affect the healthcare usage among the homeless population.
Just like England has universal health coverage, an analysis from Canada mentioned people with low physical scores and low mental health, and young people who have been previous victims of abuse and any physical assault for the last year have more unmet needs of healthcare services. However, researchers have not yet done similar studies in Europe to confirm the same.
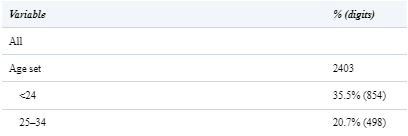
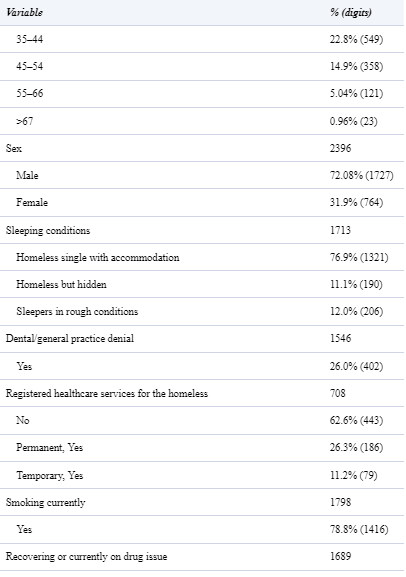
In the survey, volunteers who participated were 2505. The features of these members are below (Table 1). Most participants were youthful members (54.3% were below 35years), with the men taking the largest percentage of 69.2%. From the total participants, 76.9% were single homeless people. A common health problem detected among the homeless population was mental illness, with 85.5% of the participants currently suffering from the disease and 42.1% reported having formally been diagnosed with the disease. Over the last six months, 26% of people who participated in the survey were denied enrollment with both dental and general practitioner services.
Table 1
Population features of 2403 homeless members
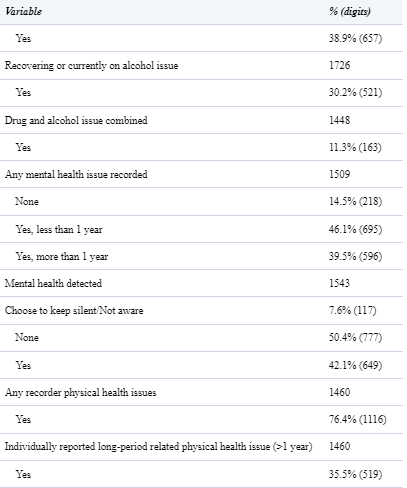
From table 2, we can see a 66.5% of the rough sleepers showed a low rate of general practitioner registration when put in comparison, with hidden homeless and homeless single with accommodation with 87.3% and 82.0%, respectively. On the contrary, the general public's voluntary sample taken from the Health Survey institution for England showed that 98% of adults registered with a general practitioner. The table also shows that high alcohol and drug misuse rates with impaired physical health were associated with rough sleepers.
Table 2
Features of 1710 homeless people with their sleeping conditions

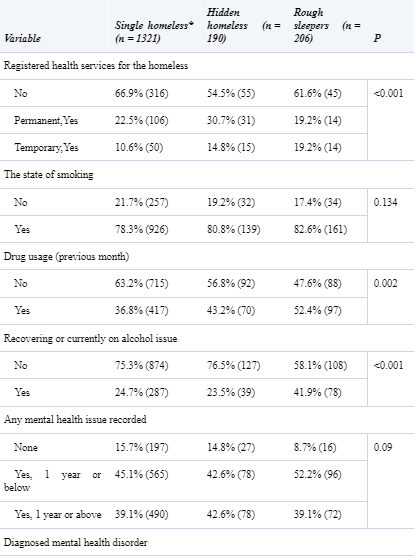

The findings from this analysis of the collaboration between the measure of primary care accessibility and sleeping status are below in Table 3. After adjusting health status measures, there existed a partnership between GP registration and rough sleeping (OR 0.45, 95% CI 0.30–0.66); however, there was no relationship connecting general practitioner utilization and rough sleeping (OR 0.71, 95% CI 0.49–1.02).
Table 3
Multivariable regression logistics assessment of linking general practitioner utilization and registration


The digits in bold show result significantly statistically at level 95%.
OR, 95% CI of odds ratio; confidence interval at 95%.
aModel 1—modified for age plus gender
bModel 2—modified for alcohol addiction, smoking condition, sex, current using or recovering drug addiction, age, recorded mental health issue, and recorded physical status.
From Table 4, it shows an assessment of elements connecting to the utilization of secondary care. No relationship between the sleeping status and secondary care findings actions. In the models fully modified, denial of registration at the general practitioner or dental is negatively related to ambulance utilization (OR 0.73, 95% CI 0.54–0.99) and admissions in hospitals (OR 0.67, 95% CI 0.49–0.91). On the other hand, usage of homeless healthcare services had a positive relationship with ambulance use (OR 1.62, 95% CI 1.14–2.31). Definitive 1.14–2.31). Definitive diagnosis showed significant results from all models that had good specifications and adequacy of fit.
Table 4
Study for multivariable logistic regression of factors related to hospital usage with homeless people
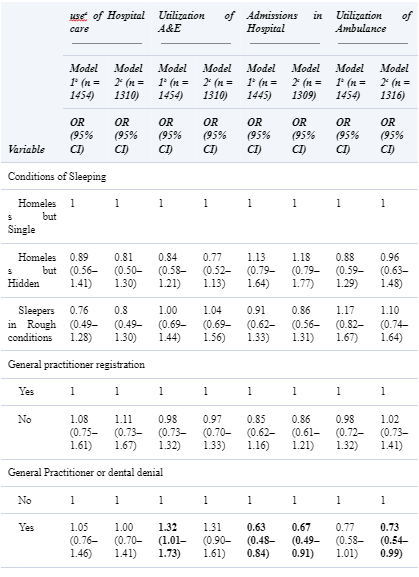

Utilization of healthcare services for the Homeless

The digits in bold show results that are significant statistically at 95%level.
OR, confidence interval at 95%, 95% CI of the odds ratio.
aHospital care utilization is associated with the study of hospital accessibility for the last six months and A&E.
bModel modified for gender and age.
cModel modified for gender, age, smoking conditions, recorded mental status, recorded physical conditions, recovering or under drug and alcohol addiction.
Table 5 indicates the findings from the negotiation assessment. We did not find any essential mediating impacts from this study. The whole findings from data accessible did not show a direct link between secondary care use and sleeping status.
Table 5
The percentage of relationship between secondary care use and sleeping status mediated by general practitioner or dentist registration in mediation assessment
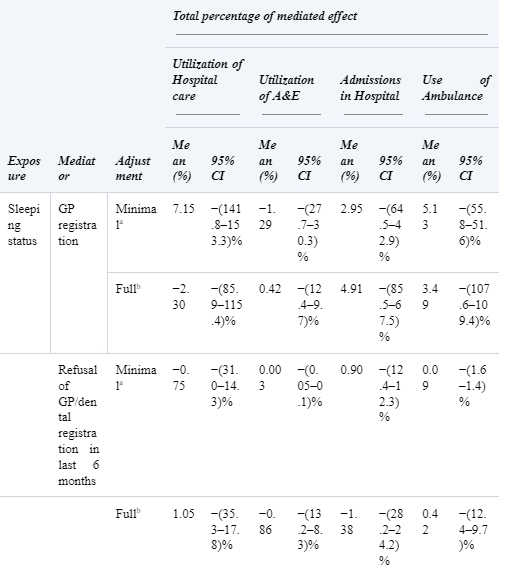
aModified for sex, age.
bModified for smoking status, sex, age, drug use, alcohol issues, physical health problems, and mental health problems.
Chapter 5: Discussion and conclusion
Factoring the crucial needs for the homeless and ignorance, health care professionals, including adult nurses, receive almost the exact healthcare needs; without any doubt, they never implement care and support for the homeless. However, we cannot discuss every issue affecting the homeless from our findings. Without a doubt, healthcare professionals and adult nurses can change by developing a positive relationship, stop being judgmental, reduce stigmatization and maintain respect for homeless patients. These will help the homeless patients to improve their communication while talking to the practitioners. With positive engagement, the nurses and healthcare professionals will deliver the best results by ensuring they meet their needs.
The Nursing and Midwifery Council (2015) mentions how nurses must always show respect, kindness, and compassion to their patients. They should always avoid misjudgment and respect personal choice, and recognize diversity. Rae and Rees (2015) participants mentioned unfair treatment against them, and how they could find it difficult to talk with the nurses as most of the time, the nurses never paid attention. Communication between the nurses and patients was poor, thereby limiting good engagement. Supposing when nurses treat homeless patients with respect, they are likely to willingly open up their healthcare issues and services to help in the treatment process. On the other hand, if nurses had exposure to the homeless lifestyle, it could bring more awareness of various health issues they face. They could gather more information that could lead to an in-depth analysis of homeless patients' needs on the first contact (Chung-Park et al., 2006). With increased awareness and knowledge, healthcare professionals will find available services plus resources to help homeless patients. Therefore, social and health care professionals need to collaborate for the sole purpose of providing health care. The NMC (2015) states that reliable and timely referral should be done to a different health professional for the patient's best interest who needs urgent care and attention (Wen et al., 2007).
With increased knowledge of the homeless people's lifestyle, adult nurses should engage with patients without judgment and combine nursing values such as 6Cs; compassion, care, communication, competence, commitments, and courage (NHS England, 2016). When healthcare professionals use these nursing values, patients feel cared for and supported; the homeless people will feel confident and indiscriminate. They will get assured that the adult nurses want to treat them equally despite the living conditions. With good communication, the quality of care given to a patient is improved, thereby building a solid therapeutic relationship between healthcare professionals and homeless patients. When healthcare professionals improve their communication, it helps homeless people feel less judged or unequally treated. Therefore, patients and adult nurses can build their relationships to allow physical and mental care to properly manage homeless patients (Kourkouta and Papathanasiou, 2014).
There has been a continuous rise of the number of people who are homeless for a while. This had been experienced because of the cuts experienced in housing and other social services, deteriorating economy, and the deinstitutionalization experienced in the country. Gentrification has been the main contributor to the loss of low-cost dwellings resulting in a reduction of cheap housing for individuals faced with homelessness, and displacing many poor people thereby increasing the number of homeless people. Therefore, people find themselves to be helpless without any form of quality life that could have protected them from diseases. They end up overwhelming the primary care facilities. Homelessness has some effects on the physical health of an individual. They may easily be injured and even be exposed to disease making them the majority that are seeking primary care services. Due to these, there are higher rates of respiratory illness, hypertension, HIV, infestation, and tuberculosis among other diseases in homeless people compared to the general population. All of which can be attributed to the lack of quality life. Lack of sufficient nutrition also contributes to homeless people not having the sufficient immunity that could help them fight diseases. Others are exposed to difficulties that leads them into depression. Exposure to stress for a long time can have negative effects on the health of an individual. From the findings also it can be detected that depression, asthma, obesity, and heart diseases are among the common problems facing individuals with prolonged exposure to stress. Ideally, homeless people are faced with high levels of poverty and economic difficulties, which are the major causes of stress in the life of an individual; as such, they are more susceptible to stress-related health conditions. Moreover, reports continue to show similar trends of disparities in physical health between homeless and housed people in samples collected from jailed inmates, homeless adults living in shelters, patients using the clinic, and HIV positive individuals.
All the above indicated disease require primary care services. The frequency of homeless people visiting the primary care facilities will rise leading to pressure on the institutions. They will also spend resources on ensuring that they improve the quality of life for these people. Therefore, even those workers who are in the primary care sector are always under pressure to serve the population. Increased cases of diseases that come as a result of homelessness is an indication that the vice comes with a burden on those who are willing to spend and ensure they have good health for productivity.
Going by the World Health Organization primary health care can be defined as an essential healthcare, based on practical, scientifically sound and socially acceptable methods and technology, made universally available to individuals and families in the community through their full participation and at a cost that the community and country can afford to maintain at every stage of their development in the spirit of self-reliance and self-determination. Similarly, primary healthcare refers to the first point of contact to the healthcare system. In this regard, this paper will discuss barriers to primary health care among homeless people based on the above two definitions. Therefore, in the case where homeless people overwhelm the healthcare sector, then it means resources would be spend to ensure that things are got right. We understand the resources are currently scarce meaning constraints will be experienced.
Most of the studies on access to primary health care among the homeless population point out to lack of a health insurance as the main barrier to primary health (Kandor et al. 2011). The homeless will lack health care access because they are not able to afford the cost of healthcare in different institutions. Moreover, lack of knowledge on where to obtain primary health care, chronic homelessness, lack of transport, long waiting times, lack of childcare, and feeling of discrimination are among the barriers to primary health care among the homeless population in the UK. Moreover, UK reports further points out that affordability, language barriers, and individual negative perception are among the challenges facing homeless people. Due to this it makes it difficult for those who want to access primary care to find it difficult.
In addition, homelessness coupled with poverty contributes to ill health through presenting unique constraints to access to health services and self-care. Similarly, poverty and homelessness increase the exposure to parasites and communicable diseases since most of this population live in open and crowded places. For instance, in case of an outbreak of a condition that is communicable, this population can easily infect each other due to poor structures and unhealthy living conditions. From the research it can detected that lack of permanent homes complicates treatment adherence and self-care of homeless people. They cited the inability to store medicine or meet refrigeration requirements make it hard to adhere to mediation or meet self-care requirements. Similarly, competing needs such as employment and food coupled with limits on shelter stay interfere with the consistent administration of medication and follow up visits to healthcare facilities. Similarly, the reports points out that lack of access to reliable and regular primary health, poor health status, and lack of specialized health services serves as significant barriers to primary health care to homeless people in the UK. It an evidence homelessness has its own challenges on the UK’s primary care sector.
Mental health problems are another factor that contributes to the lack of access to primary care. There are a number of mental healthcare cases that has been attributed to lack of proper care amongst people. The prevalence of mental health problems is high in homeless people compared to the general population and the more severe the homelessness, the more severe the mental health problem. However, despite the high rates of mental health problems in the homeless population, less than one-third of the population receive medication (Canavan et al., 2012). As pointed out above, lack of medical insurance serves as one of the major barriers to primary care. The lack of medical insurance can be attributed to various factor one of them being lack of permanent address, which is one of the vital requirement during the registration with a health care system in many countries including Canada (Anderson, Baptista, Wolf, Edgar, Benjaminsen, et al. 2006). Consequently, this forces homeless people to attempt accessing primary care through emergency services, which limits the opportunity of receiving quality health care services through inappropriate treatment and care (Hwang, Tolomiczenko, Kouyoumdjian & Garner, 2005). Moreover, the research indicates that entitlement to health care does not always to access to primary care for homeless people. This implies that there are systematic of structural factors that limit the access of homeless people to primary care. For instance, The research also outlines that limited accessibility of primary care to homeless people is due to factors such inflexible appointment procedures, opening hours, and location of the healthcare facilities. In addition, Busch-Geertsema, Edgar, Sullivan, and Pleace (2010) pointed out that homeless people experience barriers and difficulties or unwillingness in health services to accommodate their complex and various health needs. The attitudes and unwillingness in health services to accommodate the health need of homeless people scare them aware from seeking primary healthcare services. Moreover, financial constraint serves as another major factor in preventing homeless people from accessing primary care. Nevertheless, it is important to point out the lack of recognition in national affairs such as policies that highlight the plight of homeless people with regards to health care. Ideally, the majority of the policies focus on patients with mental health problems and minority communities.
As a result, there is a need to formulate policies that focus on the homeless people specifically and their diverse healthcare needs. In particular, it is important to formulate policies that address the homeless population separately other than generalizing the population with other minorities like the poor in the society. Despite the homeless being poor, their level of poverty cannot be compared to that of other minority groups in the society. This is because the absolute homeless people live in a unique environment made of complex challenges and factors that make their hardship unique. Therefore, it is important to understand their environment first and other factors that influence their lives before formulating policies that aim to address their complex healthcare needs. This can help formulate effective policies that are successful in addressing the healthcare needs of the homeless people.
Limitations of this study
The homeless population is the most challenging group for health researchers to access. A Homeless Link has collected an exceptional significance that uses a standardized sample and pre-test poll by collaborating with a group that provides services to the homeless. However, there are substantial limitations to the analysis. Precisely, the sampling was done as planned. The poll was done among those who are in touch with service providers for the homeless, and significantly, and this data does not have details of people who did not want to get involved. Nonetheless, a significant percentage of the single homeless is probably to get in touch with healthcare service providers. The demographics from the people selected reflected various studies done on single homelessness. According to the survey, high rates of participants reported.
It is hard for the government to include the homeless population in scheduled statistics like census because they frequently move and lack a permanent address. An official analysis of the sample participants was impossible. Still, research from the United States discovered samples gotten from homeless shelters could issue the best estimation of homeless people. Regrettably, in the United Kingdom, there is no similar evidence. Presumed statistical procedures applied in assessing this data uses an odd sample. While it might seem challenging to confirm this assumption, there is a possibility that the results were biased as there was no actual representative sample.
This study focused more on individually reported data on the variables used, such as healthcare utilization measures. It could have made it at risk to recall bias. The research for the validity of the individual reports for the homeless population from the United States reported ambulance visits very accurate, but the number of such visit records was never correct.
Another limitation of the survey is that it never allowed a difference between denial of general practice and dentist registration. Nonetheless, this variable was an indicator representing access to primary health care, and registration denial in any way does not invalidate this research. Lastly, the cross-sectional study involves risky informal inference, although not permanent relations making it unexpected that seen associations resulted from reverse causality.
Recommendation
Ultimate homeless people's health care needs and challenges in getting health care services are examples of inverse care law work. Besides, they do not have more significant challenges in getting healthcare services when compared to the general public. Still, there is a disadvantage for the most vulnerable when accessing primary health care services. Most of the time, people assume that it would reduce their need for secondary health care when the homeless have access to better primary health care services. It might as well be a fact for A&E services, but at a point, they did not provide a conclusive report. However, from this study, the relationship between secondary and primary health care services is complex. Better accessibility of primary health care services for the homeless population might probably provide good accessibility for essential services for inpatient for the homeless who might miss.
References
- Anderson I, Baptista I, Wolf J, Edgar B, Benjaminsen L, Sapounakis A, Schoibl H. (2006). The changing role of service provision: barriers to access to health services for homeless people. European Observatory on Homelessness, Feansta
- Busch-Geertsema V, Edgar W, O’Sullivan E, Pleace N. (2010). Homelessness and Homeless policies in Europe: lessons from research. Feansta: A report prepared for the European Consensus Conference on Homelessness.
- Campbell, D., O’Neill, B., Gibson, K., & Thurston, W. (2015). Primary health care needs and barriers to care for Calgary’s homeless populations. BMC Family Practice, 16(1). http://dx.doi.org/10.1186/s12875-015-0361-3
- Campbell DJ, Sargious P, Lewanczuk R, McBrien K, Tonelli M, Hemmelgarn B, et al. (2013). Use of chronic disease management programs for diabetes: in Alberta’s primary care networks. Can Fam Physician. 59: E86–92.
- Canavan, R., Barry, M., Matanov, A., Barros, H., Gabor, E., & Greacen, T. et al. (2012). Service provision and barriers to care for homeless people with mental health problems across 14 European capital cities. BMC Health Services Research, 12(1). http://dx.doi.org/10.1186/1472-6963-12-222
- Feansta Annual Report. (2006). The right to health is a human right: ensuring access to health for people who are homeless. Feansta Annual European Report
- Hulchanski, J., Campsie, P., Paradis, E., Hwang, S., & Chau, S. (2009). Finding home: Policy Options for Addressing Homelessness in Canada. [Toronto, Ont.]: Cities Centre Press.
- Hwang, S., Ueng, J., Chiu, S., Kiss, A., Tolomiczenko, G., & Cowan, L. et al. (2010). Universal Health Insurance and Health Care Access for Homeless Persons. American Journal Of Public Health, 100(8), 1454-1461. http://dx.doi.org/10.2105/ajph.2009.182022
- Hwang, S., Tolomiczenko, G., Kouyoumdjian, F., & Garner, R. (2005). Interventions to Improve the Health of the homeless Systematic Review. American Journal Of Preventive Medicine, 29(4), 311-311. http://dx.doi.org/10.1016/j.amepre.2005.06.017
- Hwang SW. Homelessness and health. (2001). CMAJ. 164:229–33.
- Fazel S, Khosla V, Doll H, Geddes J. (2008) The prevalence of mental disorders among the homeless in western countries: a systematic review and meta-regression analysis. PLoS Med. 5(12):e225. doi: 10.1371/journal.pmed. 0050225 5 retrieved from:http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.0050225 .
Appendix A
1. What is your age?
2. Are you single or married?
3. What is your gender?
4. What is your sleeping condition? Explain
5. Have you ever sought for healthcare services?
6. Do you smoke?
7. Do you use drugs and have sought help?
8. Do you take alcohol?
9. Do you have any mental health problem?
10. Do you have any physical health issue?
11. Are you registered to nay homeless healthcare program?
Looking for further insights on Impact of Family Presence during Cardiopulmonary Resuscitation? Click here.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



