Value-Based Healthcare and Surgical Performance
TASK ONE
The journal article “Value-based Healthcare: Measuring What Matters-----Engaging Surgeons to Make Measures Meaningful and Improve Clinical Practice” (Winegar et al. 2018) discusses the procedural actions and interest in the transformation of the profit based health services to the value based healthcare and ponders upon the dependence of this process of the healthcare analytics to determine and consequently transform the entire healthcare processes. In context of the prospects of Value based Healthcare, the scope of the journal article is of dual fold. The first could be comprehended as the establishment of the efficacy of the programmes of bundled payments such as Bundled Payments for Care improvement and the Quality Payment Programme in instilling of the psychological impetus of behavioural modification of the orthopaedic surgeons. This modification indicates the drive towards greater improvement of performance in terms of providing surgical services to the patients. The emphasis on the supposition of the Hawthorne effect on the surgeons is the literary academic credibility of this article since this amply provides the perceptual avenue to the readership through which the actual credibility and effect of the underlying thematic construct of the reliability of robust healthcare service quality and extent measurement could be realised. The article had been published in 2018 and has not been modified or updated since and this could be understood to be the currency of the article.
The intended audience has been the readership with the acute interest in the influence of the effect of data based healthcare analytics on the value based healthcare systems and the emphasis has been on the perspective of the transcendental qualities which such process of linking value reimbursement with the quality of services provided could provide against the previous researches which stressed on the awareness enhancement of the surgeons to better the clinical performance of the same.
Furthermore, the journal article of Value-based Healthcare: A Surgeon Value Scorecard to Improve value in Total Joint Replacement” (Leyton-Mange, Andrawis and Bozic, 2018), could be summarised to have emphasised on the prospective of incentivisation of care co-ordination as the scope of the clinical literature. The scope of the article has involved the process of Total Joint Replacement and the utilisation of the value based models of payment. The credibility of the article has been the outlining of the necessities of value based models of care into regular orthopaedic clinical practices and, the necessity of the medical institutions to translate the value based models of care into actual orthopaedic practice through providing the orthopaedic surgeons the information at patient and system levels, have been also discussed. The currency of the article could be outlined as it had been published during 2018 and there has not been any modification or update added to the published article. In this context, the intended audience have been different medical institutions and the currency of credence has been the value based healthcare models in enhancing the awareness of the orthopaedic surgeons concerning the performance scenario.
Furthermore, the book “Value Based Health Care: Linking Finance and Quality” (Dlugacz, 2017) could be summarised to have highlighted the interconnectivity of models of reimbursement, under the measures of value based healthcare and the previously supposed independent entities such as clinical operations, cost architecture formulation and management of quality which belonged to the prerogative of the health service providers. The book provides the scope of the rationale of linking the administrative responsibilities and clinical procedures and practices. Thus, the credence of this literary source has been to point out the detrimental effects of such divergence of operations and finances and also attempts to link these with the primary principles of quality management. The currency of the book could be outlined as it had been published during 2017 and no further modification or revision has been available. The intended audience has been the health management and care services provisioning community.

To this effect, the book “Value Management in Healthcare: How to Establish a Value Management Office to Support Value-Based Outcomes in Healthcare” (Tierney, 2017) has embarked upon the specifications concerning the emerging concepts of delivering quality through value in return for the invested costs. The scope of the book is that it could be considered as a valuable guidance material with the intended audience of the entire medical industry. The credibility of the book lies in the fact that this book provides the format through which any organisation could access the fundamentals methods of value management and could improve the healthcare delivery mechanisms. The currency of the book lies in the fact that it had been published for the first time during 2017 and has not been revised since. The intended audience have been the healthcare delivery institutions which require the learning of the specifics.
The two web resources healthinformatics.uic.edu (2018) and cms.gov (2018) have concisely drawn upon statistical and argumentative data regarding the academic exploration of the global shift from volume to value based healthcare provisioning and concerning the establishment of pioneering institutions of value based care provision such as the Centre for Medicare & Medicaid Services (CMS). The scope of these web resources has been the statistical procedures through which this transformation has been specified. The credence of these web resources have been related to the exploration of the reasons of such shifts through evaluation of the statistical data enshrined in these two web resources. The currency of the web resource healthinformatics.uic.edu (2018) has been the updated versions in the year 2018, this has also been the case with the cms.gov (2018) web resource. The intended audience have been the global patient and medical communities in this regard.
TASK TWO
Impact of Value based Healthcare on Service Users
The model of value based healthcare firmly focuses on the provisioning of maximised value to the care recipients in the form of actual qualitative services. This is primarily a coordination effort through which a set of triple objectives are pursued. These are the objective of better care provision to the patients, administering of accurate care to the patients at the opportune time and the objective of making available such care at a manageable cost structure.This could be considered to be one of the most significant concepts of healthcare reformation which had emerged during the previous 100 years of the modern clinical practices and medicinal procedures. According to Colldénet al (2017), the concept had been developed Michael Porter, the Professor at the Harvard Business School. The core theoretical emphasis of this has been on the inquest of the processes through which the global medical industry could reshape the organisational procedures as well as the methods through which the measuring of the outcomes and the cost structure could be performed. Controlling the costs has been always one of the key issues on which the concept of value based healthcare has focused. This concept recognises the stakeholders of any healthcare cost structure as the clinicians, administrators, patients and the payment remitting personnel on behalf of the patients, if the patients could not be so themselves. As per the research of Donettoet al (2015), the concept under consideration also concerns itself with the transition from the conventional service-in –return-of-fee to the more patient centric operational process of value based reimbursement models of healthcare provisioning. Fredriksson, Ebbevi and Savage (2015),has highlighted this process to be the redefining the paradigm of service delivery based on the achieved value of success. The framework of value realisation is critical from a patient centric and value provision based standpoint since this could outline the principles of progress through which the healthcare services could re-engineer the entire approach of patient centric care.
Looking for further insights on Security, Privacy, and Ethical Considerations in E-Healthcare? Click here.
As per the opinion of Greenhalgh (2017), value based model of healthcare delivery encompasses the entire range of service providers, including those of the hospitals and individual physicians, to reimburse the services in the context of provided value and achieved success on the health outcomes of the patients. The two components of the value based outcomes could be understood to be monetary factors and the qualitative worth of the lives of the patients after they avail the healthcare services. In case of the impact on the patients, the worth could be comprehended to entail the relevance and practical utilitarian applicability as well as meaningfulness of the developed and administered health solutions of the patients. The combination and establishment of linkages in between the valuation and imbursement of payments within the overall working architecture of the healthcare process could be critical and timely consideration which could yield extensive dividends for the health service recipients. According to the research of Hardyman, Daunt and Kitchener (2015), the element of impact of value could be measured through the analysis of the cost and consequences regarding the deliverables and the outcomes of the health service provision to the conditions of the patients. In this context, Hillary et al (2016) has observed that the value based healthcare systems are integral to the holistic approach which intertwines the greater outcomes of the health conditions as well as the societal conditions of the patient with that of medical expenditure. Marsh et al (2017) has outlined that this concept has been gaining significant traction in a considerably rapid manner since, for a host of reasons, the impact of such a process on the healthcare service users has been mostly positive and thus, it could be often considered as a desired avenue towards instituting greater improvement of the existing healthcare administration services. According to Meehan, Menziesand Michaelides (2017), the evidence indicated host of reasons could be identified from multiplicity of perspectives. The initial one of such evidence of the impact of the value based healthcare services on the patients has been the opportunity for the patients to expend lesser volume of money for the achievement of greater qualitative health. According to the opinion of Mkanta et al (2016), this could be considered to be one of the evidences pertaining to the positive experiences of the patient concerning the cost saving factor. The second one of such impacts is the achievement of greater efficiency in patient care by the health service providers. This could be achieved through the identification of more focused care administration systems and this leads to the business process re-engineering effects where the redundant and unnecessary segments of the health services delivery mechanisms. This could save valuable effort and time of services and could essentially provide greater satisfaction for the patients. The third of such evidences is discernable in the form of better alignment of the healthcare components by the suppliers and service providers in terms of the patient necessities and this could entail greater economical pricing as well as lesser expenditure incurrence for the health benefit outcomes of the patients. According to Mofidi et al (2016), the benefits derived from this effect could involve the particularity of health concerns such as chronic diseases and the positive outcome could influence the processes such as hospitalisation cost incurrence and medical emergencies.
As has been stated by Moriates, Shah and Arora (2016), the core aspect of any value based healthcare mechanism is the effort to provide the maximised measure of value for the involved patients. This could be more simplified in the manner of providing the best and most qualitative health solution outcomes at the lowest of the costs. As per the observation of Nilsson et al (2018) it is paramount that the healthcare systems, at the global scale, should transcend the boundaries of the conventional framework of operations which involves the supply directed and controlled healthcare service administration. Such a traditional system has been so far completely oriented towards and organised around the activities of the physicians. The value based healthcare emphasises on the person centric approach with particular significance on the necessities of patients. The resultant impact is general shift in the culture of the entire healthcare industry. This shift involves divergence from the previously prevailing focus on the volume based service specifications including profitability to the prioritisation of whatever is necessitated by the patients. Thus, the impact on the patients is consistent with the principles of the patient centric formulation of care planning as well as management of associated costs to the extent where the same could cease from becoming the source of persisting consternation for the healthcare service subscribers. This is a definite impact of the shift of conventional healthcare services to value based healthcare which could be recognised involving the patients, In this context, the research of Ocloo and Matthews (2016),has highlighted a particular evidence. This could be demonstrated as the requirement of greater involvement of the patients as well as their representations, including the payers, within the entire management of the agenda of quality. This process has to be meaningful for the process to be successful. In the previous profit based and cost oriented model of healthcare services, it could be identified, according to Serena et al (2017), that very little to no attention was ever paid to the addressing of the questions of how to define and identify the actual necessities of the patients in terms of the agenda of quality management. This had been the case with the identification of which services could be valued the most by the patients during the care experiences. This formulates the next impact probability on the patients regarding the value based healthcare. The prospect could be better realised to be the necessity to utilise the value based healthcare frameworks to translate the rhetoric of what actually matters for the patients into reality. Value based healthcare impact has also been evident from the fact that the renewed emphasis has been focused on the patients and not on the numbers of mere cases which have been performed on by the surgeons of various different streams of medicinal disciplines, including that of the Orthopaedic ones. According to Rantala and Karjaluoto (2017), during the Mid-Staff public review and inquiry at the United Kingdom, Sir Robert Francis had unequivocally outlined the necessity to progress towards greater institution of value based healthcare management and administration performance. This is a definite evidence of the impact of the value based healthcare pertaining the shift from profit based to value based health services provision.
TASK THREE
Introduction
The Personal Development Plan has been constituted on dual perspectives. The first has been that of an instrument of self-appraisal and the second one has been the basis on which the self-development objectives could be performed. As a clinical healthcare assistant, my personal development plan would be formulated with the objective to enable my professional development through performing a range of different requirements.
Personal Vision
The vision is to progress towards improvement of self-career through the upgrading of skills and abilities related with the responsibilities of the clinical healthcare assistant.


Ideal future job role


SWOT


SMART objectives




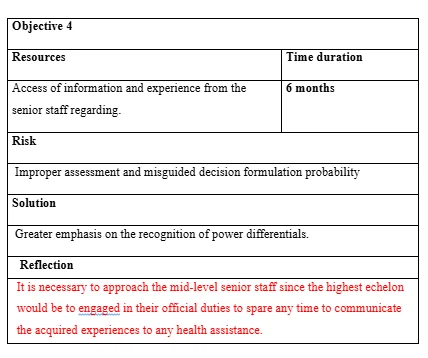
Action plan of objective fulfilment



Conclusion
The highlighted points have been development of greater effective and independent learning skills through self-directed learning, relating the skill development scenario to the wider healthcare context, performing a strength and weakness as well as opportunity and threats evaluation so as to improve the general skill sets for management of career and finally to maintain effective progression towards the skill development goals holistically. The involved components have been articulation of personal vision and task profile, resource requirement analysis in terms of objectives fulfilment and finally, an action plan formulation for personal development project.
Reference List
Colldén, C., Gremyr, I., Hellström, A. and Sporraeus, D., 2017. A value-based taxonomy of improvement approaches in healthcare. Journal of health organization and management, 31(4), pp.445-458.
Dlugacz, Y.D., 2017. Introduction to Health Care Quality: Theory, Methods, and Tools. John Wiley & Sons.
Donetto, S., Pierri, P., Tsianakas, V. and Robert, G., 2015. Experience-based co-design and healthcare improvement: realizing participatory design in the public sector. The Design Journal, 18(2), pp.227-248.
Greenhalgh, T., 2017. How to implement evidence-based healthcare. John Wiley & Sons.
Hardyman, W., Daunt, K.L. and Kitchener, M., 2015. Value co-creation through patient engagement in health care: a micro-level approach and research agenda. Public Management Review, 17(1), pp.90-107.
Leyton-Mange, A., Andrawis, J. and Bozic, K.J., 2018. Value-based healthcare: A surgeon value scorecard to improve value in total joint replacement. Clinical Orthopaedics and Related Research®, 476(5), pp.934-936.
Meehan, J., Menzies, L. and Michaelides, R., 2017. The long shadow of public policy; Barriers to a value-based approach in healthcare procurement. Journal of Purchasing and Supply Management, 23(4), pp.229-241.
Moriates, C., Shah, N.T. and Arora, V.M., 2016. A framework for the frontline: how hospitalists can improve healthcare value. Journal of hospital medicine, 11(4), pp.297-302.
Nilsson, K., Bååthe, F., Erichsen Andersson, A. and Sandoff, M., 2018. The need to succeed–learning experiences resulting from the implementation of value-based healthcare. Leadership in Health Services, 31(1), pp.2-16.
Serena, T.E., Fife, C.E., Eckert, K.A., Yaakov, R.A. and Carter, M.J., 2017. A new approach to clinical research: Integrating clinical care, quality reporting, and research using a wound care network‐based learning healthcare system. Wound Repair and Regeneration, 25(3), pp.354-365.
Van Hoof, J., Rutten, P.G., Struck, C., Huisman, E.R. and Kort, H.S., 2015. The integrated and evidence-based design of healthcare environments. Architectural Engineering and Design Management, 11(4), pp.243-263.
Winegar, A.L., Moxham, J., Erlinger, T.P. and Bozic, K.J., 2018. Value-based Healthcare: Measuring What Matters—Engaging Surgeons to Make Measures Meaningful and Improve Clinical Practice. Clinical Orthopaedics and Related Research®, 476(9), pp.1704-1706.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



