Delivering a physiotherapy program
Personalized Physiotherapy Plan
Distress Notification
While performing the Romberg’s stance, Jackie slipped and almost fell due to loss of strength and balance. During her last fall, Jackie injured her right leg and has now become less stable and confident as she walks with the crutches. Since then, Jackie has been experiencing problems with navigating uneven surfaces, clutter on the floor or climbing the ramp – increasing her risk of fall accidents. For a comprehensive approach to understanding and addressing such issues, consulting healthcare dissertation help resources can provide valuable insights. Appendix 2 illustrates a distress notification form delivered to the physiotherapist.
The Role Play
As an assistant physiotherapist, I am assigned the role of helping Jackie perform the above-mentioned physiotherapy intervention. The following chat transcript represents my conversation with Jackie as we perform the action:
Me: Hi Jackie, so today I am going to show you a few exercises to help with your balance and strength
Patient: Oh, glad to hear that, lately it has been so difficult for me going through the ramp, I cannot even pass over to the living room
Me: that’s quite unfortunate, but don’t worry, after a few days of preforming these exercises, you will be able to regain your strength and balance, and then you can move around again
Patient: Okay, so I guess you will be showing me each move as we progress?
Me: Yes, I will first demonstrate how each move goes, then I will perform each of them together just to ensure you are doing it right
Patients: Okey, I am ready when you are ready
Me: These exercise activities are mean to enhance your balance, strength and flexibility. For the next8 weeks, we will have 2-3 sessions per week. I will gradually introduce you to the exercises to allow you make proper adjustments while ensuring your safety.
Patient: well, that sounds so organized. I already have a feeling I will enjoy each session (laughs)
Me: Yes.so the basic exercises that we are going to perform will involve holding something and will last for 10-13 seconds each, but eventually we will work out way up to about one minute each
Patient: Right, that’s manageable for me
Me: so, the first one is the Romberg stance. Here, we will use a chair for balance. Bring your feet as close as you can, and then just balance
Patient: without holding the chair?
Me: yes, just balance, you will only need to hold the chair when you feel like you are totally off balance
Patient: like this?
Me: Yes. Then hold on there for 13-15 seconds
Patient: OK. (patient performs the Romberg’s stance but slips, almost to fall)
Me: Oh Sorry. Did you hurt yourself? (supporting the patient from falling)
Patient: Not Much, I just feel some sharp pain on my right leg, but I am good, we can continue

Me: I am so sorry; I will notify the physiotherapist about that and we will develop a better plan to treat the pain. You will be fine.
Me: The second exercise will still involve the Romberg’s stance, but with your eyes closed
Patient: Ahaa!
Me: yes, it is the same thing, but only that this time, you will close your eyes and make sure you hold on to the chair if you need to
Patient: Like this?
Me: Yes, ensure you keep your eyes closed until you are done.
Patient: Got it!
Me: So, the third activity will be Romberg’s again, but you will throw your head side to side to through your visual a little bit off balance.
Patient: Sounds like we are beginning to ramp up. Hehe
Me: Yes, again, make sure you hold on to the chair to start off with
Patient: Like this?
Me: Yes. Exactly.
Patient: Wow! That almost threw me off balance
Me: Ok. Now we move to the next activity, which is standing with more weight on one leg while remaining the other leg on the side.
Patient: So, basically, I stand with one leg?
Me: Yes. You can hold the chair if you feel off balance
Patient: like this?
Me: Yes, hold on for 15 seconds. I will count
Patient: Ok
Me: In the next exercise, you will use the chair to sit and stand without any support
Patient: Really?
Me: Yes, I will be close to offer support when you really need it
Patient: Ok, let me try
Me: so that marks the end of our session, and as I mention, we have one more session for this week, where we will perform more advanced exercises.
Patient: Ok. Thank you.
Q. 1 the client’s physiotherapy needs
Jackie was suffering from age-related decline in various physiological system that led to decreased muscle strength and flexibility, slowed motor process, and reduced central processing of sensory information. Apart from increased risk of falls, Jackie’s diminished mobility and balance may limit her participation in leisure or community activities, and activities of daily living. Due to these needs, she cannot get out of her home to access the community, lacks confidence when walking around the home, and cannot spend much time with her daughters. Therefore, it is important that she engages in balance exercises as part of her physical activity program.
Q2. How her needs were met
A balance and strength exercise were prescribed by a physiotherapist to meet Jackie’s needs. According to Hall et al (2018), the balance and strength exercises are usually undertaken to improve strength, posture, locomotor performance in older adults, standing balance and reduce risks of falls. Through balance and strength exercise, Jackie would have strengthened balance control – improving her fall-related efficiency and better walking speed (Dunsky, 2019). furthermore, through balancing and strength exercises, Jackie would have improved physical function, and eventually improved quality of life (Hamed et al, 2018).
Q3. How I assisted the client in undertaking this physiotherapy program
My main role was to assist Jackie to conduct basic balance and strength exercises at home using simple and available equipment- a chair. In doing so, I first explained to Jackie the meaning of the exercises, and how they would assist in increasing her strength and balance to achieve the said objectives. Afterwards, I demonstrated each physical activity before allowing Jackie to carry them out. As she carried out the exercises, I observed to see whether she was doing them in the right way. This enabled me to apply the necessary physiotherapy skills needed in light with the biopsychosocial model to ensure patient-centred and holistic approach (Rose et al, 2017).
Q4. How I identified if the client was experiencing pain and what action I took to address this issue
I noticed that the client experiencing pain when she kept complaining of her right leg. Furthermore, her mobility became more impaired and could not perform activities such as going to the toilet – which she could do a while ago. Moreover, I sought more information from her daughters, who mentioned he increased pain complaints especially at night.
Upon hearing this, I initiate da pain assessment process by asking Jackie some questions that would help me determine the interval at which the pain occurs. I relied on self-report, regarded as the single most reliable method to determine client’s experience of pain in healthcare research and practice (Bullock et al, 2019). eventually, I was able to determine Jackie’s experience of pain in terms of pain presence, intensity and interference with activities of her daily life.
Q5 Client distress and how I responded to this distress
After falling down the ramp, I noticed that Jackie was distressed and needed emotional support. According to Zebrack et al (2019), responding to patient requires effective communication skills that gives them the emotional support they require. As I supported Jackie to stand up after falling on the ramp, I used supportive expressions to relieve her distress, allowed her to express her emotions and reassured them that she will be fine in a couple of days. In the process, as recommended by Calfee et al (2018), I spoke to her gently, and talked in a way that inspired hope without hugging or touching hugging her. More importantly, I asked Jackie to tell me what scares her most about her condition and reassured her that I will be there to support her through it.
Q6. How to respond to client’s adverse reaction during the intervention
In case Jackie reacted adversely to the interventions I would initiate a crisis intervention that seeks to reduce the intensity of her physical, emotional, behavioural, and mental reaction to the adverse event. In doing so, as recommended by Zebrack et al (2019), I would advise Jackie of the normal reactions to abnormal reactions and inform her that the reaction is temporary, giving her hope that she will recover upon receiving an intervention from the physiotherapist.
Q7. A description of the document management system that I am required to use within my workplace
My workplace subscribes to eClinicalWorks client management software to keep and manage patient records. It entails various automated systems useful in tracking patient information, prescriptions, diagnoses encounter and interactions within the organization. The software focuses on general patient management and perform several other specific processes such as blood testing and inpatient tracking, all of which are meant to make my job as a provider more manageable and smoother.
The eClinicalWorks provides a range of benefits to me as a practitioner. For instance, it facilitates effective practice management. Through the eClinicalWorks mobile app, I can streamline every element of my practice including clients’ medical record keeping, patient scheduling, charting, billing and claims settling functions. This software also facilitates my efficient and timely patient care, especially when there is a heavy patient flow. The scheduling functionalities in the eClinicalWorks enable immediate patient record transfers and enhances patient workflows by eliminating treatment errors that emanate from incomplete data.
Q8. If I notice that the client is confused or misunderstands the information, I provide to them, what steps do I need to take?
Older patients like Jackie may be cognitively impaired and present continuous communication problems. As such, according to Werner et al (2017), they may have challenges following any instructions about their care, including when and how to adhere to the prescriptions. Therefore, it is crucial to keep a close monitoring of their care management. There are several techniques that I can use to manage a situation. First, I would try to address the patient more directly regardless of her cognitive impairment. Also, as recommended by Scholzet al (2020), I would try to gain the patient’s attention by sitting in front of her – at the same level as her to maintain eye contact.

The other effective communication technique I would use is to speak at a natural pace and distinctively – resisting the temptation of speaking loudly. More importantly, I would orient the patient by explaining and re-explaining the instructions, who I am and how I would help her improve hear health status. Moreover, as I did throughout the role play, I would reassure and support the patient, acknowledging whenever their response is right. If she gropes for a work, I would offer her a gentle assistance. Lastly, whereas open-ended questions are desirable in most patient-practitioner situations, patients with cognitive problems may find it difficult to cope with them. Therefore, I would consider multiple-choice questions or yes/no questions.
Dig deeper into Decision Making in Healthcare with our selection of articles.
References
Bullock, L., Bedson, J., Jordan, J.L., Bartlam, B., Chew‐Graham, C.A. and Campbell, P., 2019. Pain assessment and pain treatment for community‐dwelling people with dementia: A systematic review and narrative synthesis. International journal of geriatric psychiatry, 34(6), pp.807-821.
Calfee, C.S., Delucchi, K.L., Sinha, P., Matthay, M.A., Hackett, J., Shankar-Hari, M., McDowell, C., Laffey, J.G., O'Kane, C.M., McAuley, D.F. and Johnston, A.J., 2018. Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: secondary analysis of a randomised controlled trial. The Lancet Respiratory medicine, 6(9), pp.691-698.
Dunsky, A., 2019. The effect of balance and coordination exercises on quality of life in older adults: a mini-review. Frontiers in aging neuroscience, 11, p.318.
Hall, E.A., Chomistek, A.K., Kingma, J.J. and Docherty, C.L., 2018. Balance-and strength-training protocols to improve chronic ankle instability deficits, part I: assessing clinical outcome measures. Journal of athletic training, 53(6), pp.568-577.
Hamed, A., Bohm, S., Mersmann, F. and Arampatzis, A., 2018. Exercises of dynamic stability under unstable conditions increase muscle strength and balance ability in the elderly. Scandinavian journal of medicine & science in sports, 28(3), pp.961-971.
Rose, D.K., Nadeau, S.E., Wu, S.S., Tilson, J.K., Dobkin, B.H., Pei, Q. and Duncan, P.W., 2017. Locomotor training and strength and balance exercises for walking recovery after stroke: response to number of training sessions. Physical therapy, 97(11), pp.1066-1074.
Scholz, B., Goncharov, L., Emmerich, N., Lu, V.N., Chapman, M., Clark, S., Wilson, T., Slade, D. and Mitchell, I., 2020. Clinicians’ accounts of communication with patients in end-of-life care contexts: a systematic review. Patient Education and Counseling.
Werner, S., Yalon-Chamovitz, S., Rinde, M.T. and Heymann, A.D., 2017. Principles of effective communication with patients who have intellectual disability among primary care physicians. Patient education and counseling, 100(7), pp.1314-1321.
Zebrack, B., Kayser, K., Bybee, D., Padgett, L., Sundstrom, L., Jobin, C. and Oktay, J., 2017. A practice-based evaluation of distress screening protocol adherence and medical service utilization. Journal of the National Comprehensive Cancer Network, 15(7), pp.903-912.
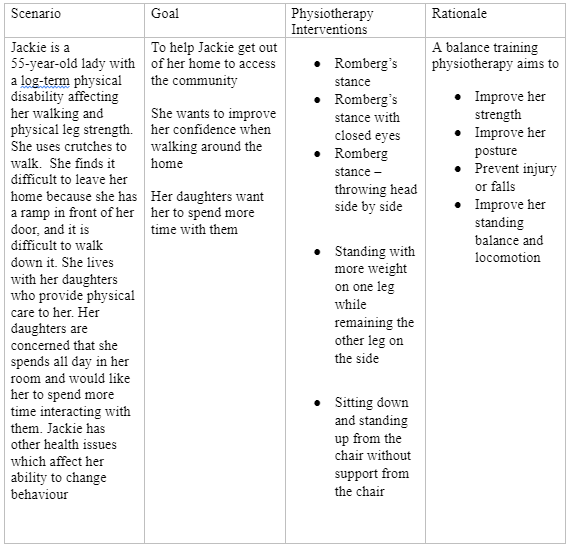
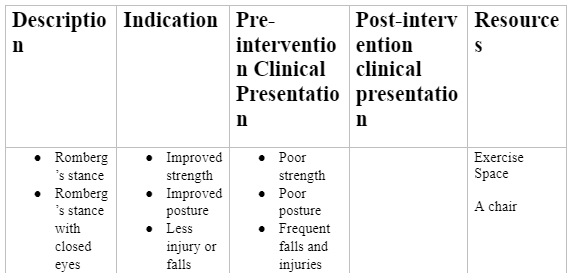
Appendix 1: Physiotherapy intervention delivery template

Appendix 2: Distress notification note
Physical Therapist Assistant
Distress Notification Note
XXX Care Unit
Patient Name:
Patient ID:
Case Number:
Name of Assistant Physiotherapist
Contact:
This is to notify you that while performing the Romberg’s stance, Jackie slipped and almost fell due to loss of strength and balance. She mentioned a sharp pain on her right leg. During her last fall, Jackie injured her right leg and has now become less stable and confident as she walks with the crutches. Since then, Jackie has been experiencing problems with navigating uneven surfaces, clutter on the floor or climbing the ramp – increasing her risk of fall accidents. Appendix 2 illustrates a distress notification form delivered to the physiotherapist.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



