Health in Diversity: Unveiling Perspectives on COPD and Well-being
Introduction
The World Health Organisation (WHO) defines health as a state of complete social, mental and physical well being and not merely characterized by the absence of infirmity. This is consistent with the biophysical model of health considering the psychological and physiological factors of well being and interaction with a series of social factors. It differs from the traditional medical model that defines health through the absence of specific illness and stresses the importance of clinical diagnosis. However, Chatterjee and Noble (2016) defined health as an ability to self manage and adapt, which is inclusive of the ability of people to adjust to the changes as key to health and the meaning of health will differ from person to person depending on their needs. The assignment in the mentioned context works on understanding the concept of health and COPD. The assignment, therefore, provides a brief explanation of COPD, the factors that cause the disease, coupled with the possible symptoms. However, it is important to note the fact that COPD is a chronic ailment and demands holistic treatment. The role of nurses is of prime importance to ensure that the patient's needs are answered just in time. The research literature, therefore, works on comparing the statistics of COPD in Kensington and Chelsea to that of Westminster and the World Health Organisation (WHO). In a similar vein, the research report discusses the possible barriers to treatment and, with healthcare dissertation help, provides better health alternatives for disease management.
A brief explanation of COPD
COPD or Chronic obstructive pulmonary disease is a common lung disorder causing difficulty in breathing. The most common is chronic bronchitis and emphysema. As pointed out by Hillebregt et al. (2017, p. 123), several people with COPD have both chronic bronchitis and emphysema. Emphysema slowly destroys the alveoli disrupting the outward air flow. Bronchitis, on the other hand, leads to inflammation of the bronchial tubes, allowing the accumulation of mucus. As opined by Zakrisson et al. (2019, p. 179), the top cause of COPD is smoking tobacco; however, long term exposure to chemical irritants can result in COPD. There remains no cure for COPD, but the use of the right treatment can ease the symptoms while lowering the chances of complications. The use of the right medical intervention such as oxygen therapy, medications and other forms of treatment can help in improving the quality of life. If kept untreated, COPD can lead to additional health issues such as worsening of respiratory problems and heart problems.

Symptoms:
COPD makes it difficult to breathe and the symptoms are varied through the stages and gradually progress with later stages.
Early symptoms:
Occasional shortness of breath after heavy activity such as exercise
Recurrent but mild cough
The urge to clear the throat, especially first thing in the morning
The early symptoms may often manifest subtle changes in lifestyle, such as skipping exercises and avoiding the stairs. Symptoms may progressively worsen over time. As the lungs become more damaged patient may experience:
Shortness of breath, even after mild physical exercise
Wheezing during exhalations
Tightness in the chest and chronic cough without or with mucus
Lack of energy and frequent respiratory infections
In later stages, the COPD degrades the condition of the patient and the following symptoms are as follows:
Fatigue
Swelling of lower limbs
Weight loss
Epidemiology in the UK
A rough estimation suggests that 1.2 million people live with diagnosed COPD (Rothnie et al. 2017, p. 1663). In terms of diagnosed cases, COPD can be termed as the second most cause of common lung ailment in the UK after asthma 4.5% of the total population lives with COPD (Landis et al. 2017, p. 84). Research suggests prevalence is on the rise, the number of people is increasing hinting towards the fact that there may be a possibility of more undiagnosed cases of the disease is becoming more common. However, Chalmers et al. (2017, p. 5) suggested prevalence increased by 9% in successive years while the practice related to record-keeping is the same. The distribution of COPD was higher in the north of the UK, North East and North West of England (Statistics.blf.org.uk, 2020). In 2012, the proportion of males suffering from COPD was always higher than the females of the same age group. The death from COPD was higher in the UK compared to the rest of the countries within the European continent (Statistics.blf.org.uk, 2020). The statistics provide a clear understanding that the UK is at high risk of COPD and there certainly exist in health determinants that make the condition worse in the country.
Determinants of COPD through Marmot Indicators
Poor housing: Older homes or houses with poor repair increases the exposure to mould due to water leakage and humid basement. As influenced by Whittaker et al. (2019, p. 1063), people may inhale mould spores causing triggers of COPD. Similarly, crowding increases the risk of spreading the germs causing infections, triggering an asthma attack or COPD
Environment: Warm environment is a breeding ground for pathogens, especially dust mites that can cause respiratory irritation. Dust mites cause continuous irritation of the respiratory tract and lead to the formation of mucus and a constant urge to clean throat (Takundwa et al. 2017, p. 97).
Age: The human lung grows until the age of 12 years and matures until the age of 20 years in the case of females and 25 in the case of males (Brandsma et al., 2017, p. 170073). The function of the lung function declines with an increase in age, a manifestation of physiological and structural change to the lungs. As influenced by Price et al. (2016, p. 5), with the advent of age the natural defense mechanism of lungs gradually decreases causing an increased risk of infection
Gender: Genetic predisposition specific to gender for damage to the lungs in response to tobacco exposure can be termed as a potential explanation for the findings. As pointed out by Fisk et al. (2018, p. 336), women have smaller airways than men, suggesting the fact that smoking the same amount of tobacco as men may lead to greater exposure for women. Bronchial hyperresponsiveness is typically associated with asthma and linked with COPD mortality more in females than in males with mild COPD. The gender-related difference may start during the initial stages of life and could be further influenced by sex hormones. For instance, females exposed to tobacco smoke or air pollution show reduced functionality of lungs than boys exposed to the same amount of tobacco.
Economic status (stress): Poor economic conditions can often make COPD go untreated (McDaniel, 2018, p. 205). In similar regards, Chalmers et al. (2017, p. 6), pointed out the fact that people smoke to relieve stress and smoking tobacco can be termed as one of the greatest factors of COPD.
Social situation: A study conducted by (Oates et al. 2017, p. 612) found the fact that low baseline functional capacity, indicative of health-related problems. Absence of health-related limitations and poor knowledge among the patients related to the disease can be termed as a leading cause of COPD
Compare the statistics of COPD in Kensington and Chelsea to that of Westminster and World Health Organisation (WHO)
Across the region of England, 1.1 million individuals are diagnosed with COPD, inclusive of a series of lung conditions causing problems in breathing (Library, 2020). As per the data and information available, COPD registration is available for Wales, Scotland and Northern Ireland. However, there exists no corresponding data on the location of the patients (Library, 2020). Thus, comparable estimates for small areas can be produced in the case of England. However, the national prevalence level can be provided for the rest of the places in the UK. For Scotland and Wales, it is 2.3% for Northern Ireland it is 2% (Statistics.blf.org.uk, 2020)
Areas with highest COPD prevalence
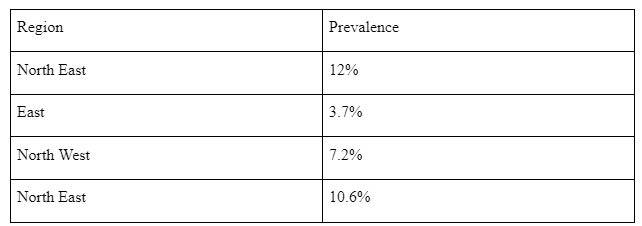
Some of the highest rates of COPD are highest in the northern sides of the country. The rate of increase can be attributed to factors such as the presence of suspended air pollutants in an urban lifestyle. In similar regards, Chelsea has the highest number of smokers and the adult smoking rate is 50% higher in the city than statewide (Pleasants et al. p. 2475). Thus, it can be conclusively stated, smoking can be termed as one of the leading causes of COPD. Westminster has a lower COPD prevalence as compared to the other regions of England. COPD rates tend to be higher among the older population and Westminster has younger than the average population. However, the rate of COPD in some places of Westminster is higher than expected based on the age of the current population. Citing an example from other places Tower Hamlets has prevalence two thirds higher than as per the expected age structure. Areas in and around Islington and Dagenham have 40% more prevalence than the expected ones (Statistics.blf.org.uk, 2020). Keeping this in mind, there are certain areas with lower rates of prevalence than their age profile would predict, especially in areas such as Ealing and Richmond. The increase in smoking habit can be termed as one of the leading causes of COPD.
Role of nurses in managing COPD
The nurses need to embrace a proactive measure for addressing the health issue related to COPD. The goal of effective COPD management plan is to prevent the following:
Prevent the possible progression of the disease
Relieve the symptoms
Improve tolerance towards exercise
Improve health status
Treat and prevent possible health complications and exacerbations
Reduce the rate of mortality
From the point of nursing intervention, it can be clearly stated that effective management of COPD is inclusive of four components as follows:
Assess and monitor the disease: Diagnosis of COPD is dependent on previous medical history coupled with the presence of airflow related limitation that is not fully responsible. As stated by Early et al. (2017, p. 2955), patients with chronic cough and sputum need to be tested for limitation of airflow, even if they do not exhibit symptoms of dyspnoea. Thus, nurses working with COPD patients should have access to spirometry. Measurement of arterial blood gas tension should be taken into consideration with FEV1 less than 40% may act as a suggestive sign of respiratory failure (Coventry et al. 2019, p. 659)
Reducing the associated risk factors: Reduction in total exposure to tobacco smoke and even respiratory irritants is important to reduce the onset of COPD. As influenced by Martins et al. (2016, p. 5), smoking cessation can be termed as the single most effective way of reducing COPD. The nurses should obtain optimum knowledge about tobacco dependence treatment and the nurses or responsible healthcare professionals should offer the patient with this treatment. As stated by Gergianaki et al. (2019, p.3), nurses are often asked to act as a point of communication for the patients. Thus, counseling can be termed as a great way of ensuring practical counseling and social support, as a part of healthcare treatment. Similarly, the progression of occupationally induced respiratory disorders can be controlled through strategies aimed at reducing the amount of inhaled gases
Manage stable COPD: The overall approach for managing COPD is characterized by an increase in treatment based on disease severity. Patients with severity need to be characterized by systematic treatment. As opined by Aasbø et al. (2019, p. 299) health education related to COPD plays an important role in coping with the illness and effective in accomplishing goals such as smoking cessation. Bronchodilator related medication is central to symptomatic management related to COPD. As stated by Dennis et al. (2017, p. 2017), continuous treatment with glucocorticosteroids needs to be administered regularly only for symptomatic patients. The long term administration of oxygen through the use of a nasal cannula, more than 15 hours per day with patients suffering from chronic respiratory problem or failure is shown to have effective results (Yin, Yang, and Ye, 2018, p. 152)
Manage exacerbations: one of the most common causes of exacerbation is an infection within the tracheobronchial tree. Patients experiencing exacerbation with clinical signs related to airway infection experience a change in colour of sputum (Liu, Zhao, and Hao, 2019, p. 2589). Finally, non-invasive positive pressure ventilation in acute exacerbation improve the circulation of blood gases and reducing the rates of mortality
Role of nurses in reducing pain related to COPD
Pulmonary rehabilitation is a specialized program designed to ease the pain. Thus, pulmonary rehabilitation can help in reducing pain among patients. Breathing exercises can work on reducing the problems and a typical program is the inclusion of the following:
Physical exercise tailored as per the ability and need of the patients such as walking and cycling
Education about the condition to the patient
Psychological and emotional support
Chronic disease management at home
With the increasing incidents of COPD, it becomes important to note the increasing prevalence of COPD can lead to additional pressure on healthcare organizations (Rodgers, Stanton and Jackson, 2018, p. 210). The increasing rates of patients create a pressure on the existing resources and medical facilities. Thus, it becomes increasingly important to manage the pressure of disease and treatment is given to patients in the comfort of home. Personalized COPD plan at home prevents flair ups and emergency visits to the hospitals. Healthcare services at home implement a combination of nursing care and therapy to maintain a high quality of life. The healthcare professionals will monitor the symptoms by educating the patient and their family members. Compliance with medication is of absolute importance, the nurses instruct the patient with ways to use inhalers and the importance of sticking with a suitable medication regime for managing COPD. As influenced by Sandelowsky et al. (2018, p. 12), nutrition plays an important role in COPD management, especially intake of fluid. Weight management can play an important role in managing breathing difficulties. Physical therapy can help COPD patients to achieve events of dyspnea and preventing the need for hospitalization continuously. Physical therapists make use of exercise regimes for strengthening the pulmonary system building endurance and muscle strength. Physical therapy helps in performing a series of activities without becoming out of breath. This is accompanied by a teaching series of breathing activities and ways to conserve energy.
Barriers to treatment
The evidence-based study suggested the fact that there exists no treatment for COPD (McDonald, Roberts and Inder, 2018, p. 192). A combination of medication can be suggested to decrease the symptoms. As stated by Barken, Thygesen and Söderhamn (2017, p. 181), the current series of medication can produce limited effects as none have shown to slow or reverse symptoms of possible lung damage. The cost of care can emerge out as a possible prohibitive barrier for several patients. The series of expensive drugs, coupled with therapy is a cumbersome burden on some patients. As observed by Zakrisson et al. (2017, p. 182) when patients cannot pay for the medications they are less likely to have it, which in return can aggravate the symptoms. Mental health disorders such as depression provide low confidence for the patient to trust the physician.
A study conducted by Cox et al. (2017, p. 155), found that patients are likely to follow COPD management therapy if clinicians encourage the participation of caregiver. The matching interval of dosing with the lifestyle of the patient and making the required medical appointment becomes a bit difficult. However, Aasbø et al. (2019, p. 293), pointed out the barrier created due to lack of research. As supported by Baker and Fatoye (2019, p. 26), scientific studies need to address the phenotypes and understand the merger of genes with the environment. Thus, the future lies within the use of personalized medicine as the symptoms of COPD are subjective and personalized medication creates a better response to people. A final barrier is the reluctance of people in not participating in clinical trials. The NHS is funding COPD management strategies but these studies are still in need of participants. The strategies by NHS can be stated as follows (Duenk, 2017, p. 99):
LEEP: Losartan Effects on Emphysema Progression. This Randomised clinical trial evaluates the efficacy of anti-hypersensitive drug losartan that slows down the progression of emphysema related to COPD
RETHINC: REdifining Therapy IN early COPD, determines evaluates the possible effects of bronchodilators in helping the ex-smokers and symptomatic smokers gain normal lung function
INSIGHT COPD: Intervention Study IN overweight patients with COPD works on relating weight with COPD. Researchers planned ways for modest weight loss coupled with an increased activity that improves shortness of breath.
Despite the series of medical interventions, there remains no improvement in the rates of COPD. There remains no doubt that the interventions are not targeted to answer the needs of the population suffering from COPD. The barriers become a major hindrance in treating COPD related problems.

Conclusion
Based on the above study research it can be easily seen that COPD in the UK is the highest. The rate of prevalence can be attributed to a series of factors such as poor adherence to medication and a lack of suitable knowledge. Nurses lack the required training needed to manage patients with COPD. Analyzing the current scenario, it can be easily seen that the condition in the Kengiston and Chelsea is better in regards to better living conditions. However, the other areas in London are severely affected due to the presence of possible irritants in the atmosphere. These irritants are often a manifestation of pollutants. The urban areas are subjected to a greater risk of smoking due to lifestyle stress. In similar regards, it can be easily concluded that COPD is a chronic disease, targeted medicine, and strategic nursing intervention can address the possible issues.
Continue your journey with our comprehensive guide to Health Implications of Climate Change.
Reference list
Aasbø, G., Kristvik, E., Nyheim Solbrække, K. and Werner, A., 2019. Searching for “transformative moments”: A qualitative study of nurses’ work during home visits to COPD patients and their caregivers in Norway. Nursing open, 6(2), pp.293-300.
Baker, E. and Fatoye, F., 2019. Patient perceived impact of nurse-led self-management interventions for COPD: A systematic review of qualitative research. International journal of nursing studies, 91, pp.22-34.
Barken, T.L., Thygesen, E. and Söderhamn, U., 2017. Advancing beyond the system: telemedicine nurses’ clinical reasoning using a computerised decision support system for patients with COPD–an ethnographic study. BMC medical informatics and decision making, 17(1), p.181.
Brandsma, C.A., de Vries, M., Costa, R., Woldhuis, R.R., Königshoff, M. and Timens, W., 2017. Lung ageing and COPD: is there a role for ageing in abnormal tissue repair?. European Respiratory Review, 26(146), p.170073.
Chalmers, J.D., Tebboth, A., Gayle, A., Ternouth, A. and Ramscar, N., 2017. Determinants of initial inhaled corticosteroid use in patients with GOLD A/B COPD: a retrospective study of UK general practice. NPJ primary care respiratory medicine, 27(1), pp.1-8.
Chatterjee, H. and Noble, G., 2016. Museums, health and well-being. Routledge.
Coventry, P.A., Blakemore, A., Baker, E., Sidhu, M., Fitzmaurice, D. and Jolly, K., 2019. The push and pull of self-managing mild COPD: An evaluation of participant experiences of a nurse-led telephone health coaching intervention. Qualitative health research, 29(5), pp.658-671.
Cox, K., Macleod, S.C., Sim, C.J., Jones, A.W. and Trueman, J., 2017. Avoiding hospital admission in COPD: impact of a specialist nursing team. British Journal of Nursing, 26(3), pp.152-158.
Dennis, S., Reddel, H.K., Middleton, S., Hasan, I., Hermiz, O., Phillips, R., Crockett, A.J., Vagholkar, S., Marks, G.B. and Zwar, N., 2017. Barriers and outcomes of an evidence-based approach to diagnosis and management of chronic obstructive pulmonary disease (COPD) in Australia: a qualitative study. Family practice, 34(4), pp.485-490.
Duenk, R.G., Verhagen, C., Dekhuijzen, P.N.R., Vissers, K.C.P., Engels, Y. and Heijdra, Y., 2017. The view of pulmonologists on palliative care for patients with COPD: a survey study. International journal of chronic obstructive pulmonary disease, 12, p.299.
Early, F., Young, J.S., Robinshaw, E., Mi, E.Z., Mi, E.Z. and Fuld, J.P., 2017. A case series of an off-the-shelf online health resource with integrated nurse coaching to support self-management in COPD. International journal of chronic obstructive pulmonary disease, 12, p.2955.
Fisk, S.A., Mulinari, S., Wemrell, M., Leckie, G., Vicente, R.P. and Merlo, J., 2018. Chronic obstructive pulmonary disease in Sweden: an intersectional multilevel analysis of individual heterogeneity and discriminatory accuracy. SSM-population health, 4, pp.334-346.
Gergianaki, I., Kampouraki, M., Williams, S. and Tsiligianni, I., 2019. Assessing spirituality: is there a beneficial role in the management of COPD?. NPJ primary care respiratory medicine, 29(1), pp.1-5.
Hillebregt, C.F., Vlonk, A.J., Bruijnzeels, M.A., van Schayck, O.C. and Chavannes, N.H., 2017. Barriers and facilitators influencing self-management among COPD patients: a mixed methods exploration in primary and affiliated specialist care. International journal of chronic obstructive pulmonary disease, 12, p.123.
Landis, S.H., Wurst, K., Le, H.V., Bonar, K. and Punekar, Y.S., 2017. Can assessment of disease burden prior to changes in initial COPD maintenance treatment provide insight into remaining unmet needs? a retrospective database study in UK primary care. COPD: Journal of Chronic Obstructive Pulmonary Disease, 14(1), pp.80-85.
Lim, J.U., Lee, J.H., Kim, J.S., Hwang, Y.I., Kim, T.H., Lim, S.Y., Yoo, K.H., Jung, K.S., Kim, Y.K. and Rhee, C.K., 2017. Comparison of World Health Organization and Asia-Pacific body mass index classifications in COPD patients. International journal of chronic obstructive pulmonary disease, 12, p.2465.
Liu, M., Zhao, Y. and Hao, H., 2019. Intervention of high-quality nursing care in combination with transitional care in the treatment of COPD patients. Int J Clin Exp Med, 12(3), pp.2583-2590.
Martins, S.M., Salibe-Filho, W., Tonioli, L.P., Pfingesten, L.E., Braz, P.D., McDonnell, J., Williams, S., Do Carmo, D., De Sousa, J.C., Pinnock, H. and Stelmach, R., 2016. Implementation of ‘matrix support’(collaborative care) to reduce asthma and COPD referrals and improve primary care management in Brazil: a pilot observational study. NPJ primary care respiratory medicine, 26(1), pp.1-7.
McDaniel, J.T., 2018. Prevalence of chronic obstructive pulmonary disease: county-level risk factors based on the Social Ecological Model. Perspectives in public health, 138(4), pp.200-208.
McDonald, V.M., Roberts, M. and Inder, K., 2018. The Respiratory Nurse in Pulmonary Rehabilitation. In Textbook of Pulmonary Rehabilitation (pp. 183-194). Springer, Cham.
Oates, G.R., Hamby, B.W., Stepanikova, I., Knight, S.J., Bhatt, S.P., Hitchcock, J., Schumann, C. and Dransfield, M.T., 2017. Social determinants of adherence to pulmonary rehabilitation for chronic obstructive pulmonary disease. COPD: Journal of Chronic Obstructive Pulmonary Disease, 14(6), pp.610-617.
Pleasants, R.A., Riley, I.L. and Mannino, D.M., 2016. Defining and targeting health disparities in chronic obstructive pulmonary disease. International journal of chronic obstructive pulmonary disease, 11, p.2475.
Price, D., Miravitlles, M., Pavord, I., Thomas, M., Wedzicha, J., Haughney, J., Bichel, K. and West, D., 2016. First maintenance therapy for COPD in the UK between 2009 and 2012: a retrospective database analysis. NPJ primary care respiratory medicine, 26(1), pp.1-6.
Rodgers, J., Stanton, M. and Jackson, J., 2018. Providing care to COPD patients using in-home visits by nurse practitioners. Journal of nursing care quality, 33(3), pp.208-212.
Rothnie, K.J., Chandan, J.S., Goss, H.G., Muellerova, H. and Quint, J.K., 2017. Validity and interpretation of spirometric recordings to diagnose COPD in UK primary care. International journal of chronic obstructive pulmonary disease, 12, p.1663.
Sandelowsky, H., Natalishvili, N., Krakau, I., Modin, S., Ställberg, B. and Nager, A., 2018. COPD management by Swedish general practitioners–baseline results of the PRIMAIR study. Scandinavian journal of primary health care, 36(1), pp.5-13.
Takundwa, R., Jowett, S., McLeod, H. and Peñaloza-Ramos, M.C., 2017. The effects of environmental factors on the efficiency of clinical commissioning groups in England: A data envelopment analysis. Journal of medical systems, 41(6), p.97.
Whittaker, H.R., Müllerova, H., Jarvis, D., Barnes, N.C., Jones, P.W., Compton, C.H., Kiddle, S.J. and Quint, J.K., 2019. Inhaled corticosteroids, blood eosinophils, and FEV1 decline in patients with COPD in a large UK primary health care setting. International Journal of Chronic Obstructive Pulmonary Disease, 14, p.1063.
Yin, H., Yang, L. and Ye, Q., 2018. A systematic review of the effectiveness of clinical nurse specialist interventions in patients with chronic obstructive pulmonary disease (COPD). Frontiers of Nursing, 5(2), pp.147-156.
Zakrisson, A.B., Arne, M., Hasselgren, M., Lisspers, K., Ställberg, B. and Theander, K., 2019. A complex intervention of self‐management for patients with COPD or CHF in primary care improved performance and satisfaction with regard to own selected activities; A longitudinal follow‐up. Journal of advanced nursing, 75(1), pp.175-186.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



