Marking Criteria and Feedback Form
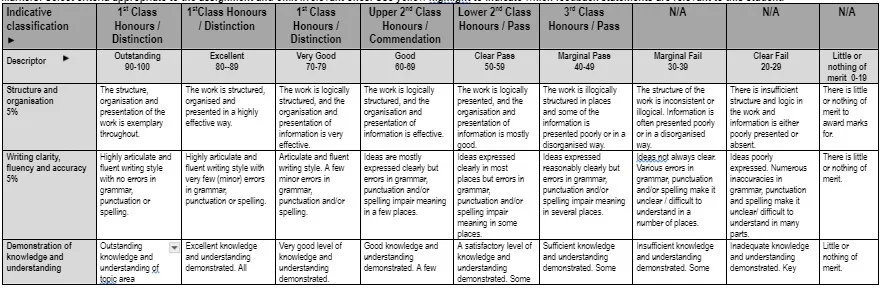
Markers: Select criteria appropriate to the assignment and omit irrelevant ones. Use yellow highlight to indicate which feedback statements are relevant to this student.



First Submission: For each day for up to five days after the published deadline, coursework submitted late will have the numeric grade reduced by 10 grade points until the numeric grade reaches the pass grade, i.e., 40 (UG) or 50 (PG); this includes deferred coursework.

Second Submission (referral): The resubmitted element, if successful, will be capped at a bare pass, i.e., 40 (UG) or 50 (PG). The full mark of any previously passed elements will be retained. Coursework submitted late, i.e., at any point after the published deadline date and time, will be awarded a zero.
Re-enrolment: Grades awarded for modules on re-enrolment will not be capped for classification purposes.
Provisional Marks: All marks are provisional until ratified by the relevant Board of Examiners.
Marking and Moderation: All marking, and moderation procedures are governed and guided by the current University’s Policies and Regulations.
Reflection on Learning
Please consider the learning you have achieved while working on this assignment and how you have applied the feedback you have been given. For example:
What previous feedback have you been given and how have you used it to inform and improve this assessment?
What have you learned in this assessment that you intend to apply to your practice and how will you demonstrate this? Keep your feedback and reflection in a file/portfolio as evidence of your professional development.
Assignment template – please type onto this document (delete content apart from the title to each section. Do not include any identifiable markers for example, your name as this will be marked anonymously. Total word count 2500 words plus or minus 10%. This essay should be written in the third person, use Ariel 12 font, 1.5 line spacing, include the page number at the end of the page, include the total word count at the end of the conclusion and present the reference list on a new page. Remember this is a level 6 piece of work and as such you need to support your discussion with relevant literature – a minimum of 20 references.
Title: Person-centred care delivery is a fundamental aspect of the nurse’s role. Critically reflect this statement in line with one of the four Nursing and Midwifery Council’s (NMC) domains as outlined in the NMC Code (2018): Prioritising people, Preserving safety, Practising effectively and Promoting professionalism and trust.
Introduction (approximately 250 words): In nursing profession, reflection is required to be purposeful, questioning and focussed regarding the activities to be performed at work. The nurses believe that regular reflection regarding the experiences at work helps in making better sense of the care environment and care delivery affecting the patients as well as performance of the nurses. It allows the nurses to determine the areas of development and learning to be further included in the objectives for professional development to ensure their continuous improvement in profession (Mildon, 2018). For those working on related topics, seeking healthcare dissertation help can provide valuable insights into enhancing reflective practices and professional growth. In nursing, person-centred care is one of the key aspects of care services. The Nursing and Midwifery Council (NMC) Code of Conduct mentions different responsibilities to be followed by nurses through four domains in ensuring quality care to be delivered to the patients. Thus, in this reflection, person-centred care guided by one of the domains (Prioritise People) of NMC Code of Conduct is to be discussed. Thereafter, a critical reflection regarding the domain and the related nurse’s role is to be mentioned. The critical reflection is the process of identifying, questioning and examining the deeply-held assumptions regarding knolwdege about events. It is important to be performed as critical reflection assist in developing meaning of the care process which helps in setting effective goals in care and use learning from the past to determine the actions to be performed in real-life implication.
Main body:
Overview of person-centred care (approximately 500 words): Person-centred care is referred to treating people receiving healthcare with respect and dignity along with involving them directly in making decision regarding their care. It is one of the 13 fundamental care standards mentioned to be met by nurses in care by the Care Quality Commission (CQC) (CQC, 2019). The four key principles of person-centred care are treating patients with compassion, respect and dignity; providing coordinated treatment, care and support; delivering personalised care, treatment and support and allowing service users for recognising and developing their ability and strength to be independently living their life (health.org.uk, 2014). The lack of following the principles of person-centred care leads to disrespecting the rights of the patients, violating the fundamental care standards set by the CQC and makes patients feel lack of independence as well as empowerment in taking their own care. It makes them feel and remain burden of care irrespective of their efficiency in taking their own care (Byrne, Baldwin & Harvey, 2020).
In my care practice environment, I performed many person-centred cares out of which one of the examples is of Michael who was 20 years old inpatient admitted to the hospital due to a car accident. The pseudonym Michael is used to indicate the patient with his prior verbal consent to maintain confidentiality and privacy as per NMC Code of Conduct (NMC, 2018). He was to undergo surgery on both of his arms due to a fracture on his left arm and superficial injuries on his right arm received during the accident. He is required to remain in the hospital for two weeks before being discharged indicating he is going to require significant assistance for his daily life activities. As a nurse I communicated with Michael to understand his needs and demands of care. He mentioned having options for personally executing everyday activities such as bathing dressing and others along with informed avoiding sitting and watching TV to pass his time. He informed me he would enjoy reading his law books and attending online lectures from the hospital. He also mentioned wish to get visited and spending time with his mother and friends who visit every evening.
On discussing with Michael, I reached the decision to make a care plan together. For bathing, he mentioned a male nurse to be taking care of his shower as he is not comfortable being naked and accepting bathing care from female nurse. However, I explained the way towels and separators would be used to ensure his privacy and way the male nurse could not always be present to which he understood the situation and accepted the condition. In regard to reading books and attending lecture, I asked his mother to bring his laptop from home and arranged setting of headphones so that he can attend the lectures. His daily management of personal hygiene was asked by Michael to be taken by him to which he was allowed to perform the act on his own as his right hand was okay to be used. I also allowed to keep his mobile with him to be used in case he wishes to talk with his friends and mothers beyond hours as requested to me but ensured it to be kept silent and not to be used beyond bed hours so that it does not disturb the other patients to which he accepted wholeheartedly.
A breakdown of the 1 domain you have chosen (approximately 500 words): “Prioritise People”
The first domain of NMC Code of Conduct is “Prioritise People” which mentions treating people as equal individuals and upholding their respect along with dignity is the initial role of the nurses (NMC, 2021). This aspect is related with person-centred care as one of the principles of the care was upholding the dignity and respect of the patients and offering them compassionate care (Haydon, Browne & van der Riet, 2018). Thus, this guidance in the domain supports my role in person-centred care to be fulfilled by allowing me to value the rights of the patient and respect their thoughts in care which would make patient feel increasingly satisfied. The section 2 of “Prioritise People” mentions listening to people and responding to their concerns and preferences in care (NMC, 2021). In order to achieve it, the nurses are to work in partnership with the patients and recognise their needs along with preferences. The nurses are to empower and encourage people in sharing decision regarding their care and treatment and respond to them in compassionate manner (Taylor et al., 2019). This section in related to person-centred care as it guides the nurses regarding the way to know the needs of patients and involve them in decision-making for care. It influenced my role in person-centred care by providing understanding regarding the way preference of the patients are to be known and they are to be involved in decision for care planning.
The section 3 of “Prioritise People” mentions patient’s physical, social and psychological needs to be examined and responded in care (NMC, 2021). It is applicable in person-centred care as the Code mentions the way holistic needs and demands of the patients are to be identified and fulfilled in promoting their well-being. The section of the domain influenced my role in person-centred care as a nurse by informing the aspects to be focussed on for patients in care so that proper advocacy can be reached for them in avoiding any vulnerable condition towards their health. The section 4 of “Prioritise People” mentions putting the patient’s interest in nursing care is to be key aspects followed by the nurses (NMC, 2021). This is applicable in person-centred care to ensure consent and relevant care practices are performed for the patient. It related with my role in the person-centred care as it leads me to deliver well-coordinated care to the patients with their involved leading to their best condition. The section 5 of “Prioritise People” mentions respecting the privacy and confidentiality of the patients (NMC, 2021). It is applicable in person-centred care to respect the privacy and confidentiality rights of the patients (Ballard et al., 2018). The aspect also influenced my role as a nurse in providing person-centred care by explaining the actions to be performed to avoid sensitive facts of the patients to be revealed in public.
The nurse’s role and the importance of critical reflection (approximately 1000 words): In the placement, by acting as a student nurse I was able to delivery person-centred care in the relation to the domain of “Prioritise People”. This is because the role allowed me to treat people with kindness, compassion and respect which is evident from the care of Michael where I compassionately interacted with him and kindly acted to fulfil his needs along with respected his priorities and demands of care. As asserted by Mechili et al. (2018), kind and compassionate care in person-centred support makes the patient more satisfied and willing to comply with the medical treatment. This leads to create better and positive care outcome for the patient. It is evident as Michael expressed enhanced compliance when I mention that male nurses could not always be present for bathing him which is understood and accepted by him out of my kind and compassionate gesture towards him throughout the care. As argued by Frankova (2018), failure of kind and compassionate care in person-centred care leads to violate the fundamental of care set by the CQC in the UK. Thus, failure to act kindly and compassionately with patients may lead the nurse face legal action.
As a student nurse, I was able to effectively deliver enhanced person-centred care in the domain of “Prioritise People” is evident as I worked in partnership with the patient to recognise their needs and preferences as mentioned under the domain. The working in partnership with the patient in person-centred care makes the patient feel recognised and effectively contribute to coordinate own care (Yuan & Murphy, 2019). However, it is argued that failure to form partnership with the patient leads the nurses to develop hindered therapeutic relationship with them which also creates conflicts in decision-making in care between them leading to chaotic care experience (Tallon et al., 2017). The case of Michael evidence that I was able to form partnership with him in deciding his care as I develop discussion with him and shared information regarding care delivery to collectively decide way care is to be coordinated towards him during his hospital stay. In “Prioritise People”, the refusal of any care or treatment is mentioned to be respected by nurses and any distress or anxiety of the patient is to be politely managed (NMC, 2021). My role as a student nurses helped me work in relation to the guidance mentioned in the domain which is evident as I respected Michaela’s decision of rejecting watching TV. Moreover, I accepted his request of allowing him to use mobile under some restrictions so that he does not feel distress out of loneliness in the hospital during care.
In relation to the domain of “Prioritise People”, the evidence that I was able to deliver effective person-centred care as a student nurse is I paid key attention and recognised the physical, social and psychological needs of the patient. It helped me to fulfil the achievement of holistic care delivery for the patient and compassionately meet the needs of the patient to avoid making their health remain vulnerable. This is beneficial because recognising and promoting holistic care of the patient helps in their overall health improvement and improved change in their well-being within short-time at all ages (Frisch & Rabinowitsch, 2019). However, argument is that failure to act with special attention to the holistic needs cause delivery of partial care support to the patients that hindered in promoting effective well-being and prevention of relapse of additional health condition (Vincensi, 2019). As a student nurse, I was able to act with “Prioritise People” domain in delivering person-centred care is evident as I avoided any discriminatory attitude or behaviour in care. For instance, in delivering person-centred care to Michael, I ensured arrangement of headset to hear lectures and mentioned his mobile use restriction so that I may not act in caring for him with favour while avoiding the peaceful care environment for other patients in the ward.
In the placement, while playing the role of student nurse it is evident I was able to delivery person-centred care in relation to the “Prioritise People” domain as I balanced the care delivery in best interest of the patient. This acted as benefit for effective person-centred care delivery because care delivery in the best interest of the patient ensures a standard approach is taken to personalise the care to most extent so that it allows individuals to have their personal needs and demands fulfilled (Dahlke, Hunter & Negrin, 2019). In contrast, failure to act in best interest of the patient would have led the nurse to include care services which are not needed by the patients that could have increased the cost of care for the individual and unnecessary care to be delivered (Hyland et al., 2020). The presence of informed consent regarding each aspect of person-centred care is essential so that action which conflicts the beliefs and thoughts of the individuals are not provided (Kunneman & Montori, 2017). As argued by Trachsel (2019), failure informed consent in person-centred care leads carry out actions that are not approved by patient’s leading to violating showing value towards their rights. In delivering person-centred care, I was always found to gather informed consent from Michael be it regarding sharing his health information or delivering him any specific care to ensure the care is provided prioritising his attitude and thoughts.
As a student, I was able to delivery person-centred care in relation to the domain of “Prioritise People” which is evident as always respected the individual’s rights to privacy in care. This is because privacy is regarded as a fundamental right to be met for any individual under the Human Rights Act 1998 (legislation.gov.uk, 1998). Thus, I never shared any original data of the real patients to explain his care and mentioned facts under his pseudonym. In person-centred care as well as in “Prioritise People” domain, it is mentioned that patients are to be informed in detail regarding their care opportunity and availability along with way care is to be provided (NMC, 2018). As argued by Cocanour (2017), failure to inform the patient regarding care delivery and its ways makes them develop hindered decisions in determining their care. This disrupts the person-centred care as the principle of offering patients to independently decide their care is not achieved in the support. However, in the care I delivered, effective information sharing was done with Michael so that he can make informed decision in accessing and approving any care. It led me as a nurse to be successful in delivering person-centred care with effectively prioritising the patients in all care aspects.
Conclusion (approximately 250 words): The reflection concludes that patient-centred care is effective part of nursing care which includes offering respect to the needs of the patients and including them in care planning to decide the final care to be received by them. On reflecting regarding my ability to deliver person-centred care in relation to the domain of “Prioritise Care” as a student nurse, I have found to show enhanced capability in the context. This is evident as while providing care I acted with kindness and compassion along with respected the dignity and rights of the individual by allowing them to mention their preference which is accepted in determining care for them. In addition, I listening to the preference of care and developed discussion with the patient to allow the person to make independent approval of the care suggested for them. I was also successful in meeting person-centred care under the domain of “Prioritise People” because I offered care in the best interest of the patient. The informed consent from the patients is also gathered and independent decision making was allowed with enhanced sharing of information regarding which nature of care could not be provided to them under what reason. It assists in clarified explanation of the nature of care provided to the individual which helps in avoiding any conflict to be raised in the person-centred care scenario.

Continue your journey with our comprehensive guide to Marketing in a Digital Age and Corporate Social Responsibility.
Reference list (should be presented on a new page – this is not included in the word count). Do visit the academic skills site and the school’s referencing handbook.
Ballard, C., Corbett, A., Orrell, M., Williams, G., Moniz-Cook, E., Romeo, R., ... & Fossey, J. (2018). Impact of person-centred care training and person-centred activities on quality of life, agitation, and antipsychotic use in people with dementia living in nursing homes: A cluster-randomised
Cocanour, C. S. (2017). Informed consent—It's more than a signature on a piece of paper. The American Journal of Surgery, 214(6), 993-997. Retrieved on 29 December 2021 from: http://publishingimages.s3.amazonaws.com/eZineImages/PracticePerfect/690/Informed-consent-Its-more.pdf CQC (2014), Our fundamental standards, Retrieved on 29 December 2021 from: https://www.cqc.org.uk/news/stories/our-fundamental-standards Dahlke, S. A., Hunter, K. F., & Negrin, K. (2019). Nursing practice with hospitalised older people: Safety and harm. International journal of older people nursing, 14(1), e12220. Retrieved on 29 December 2021 from: https://onlinelibrary.wiley.com/doi/abs/10.1111/opn.12220
Frankova, H. (2018). CQC's state of hospice services in England 2014–2017 report. Nursing and Residential Care, 20(2), 111-113. Retrieved on 29 December 2021 from: https://www.magonlinelibrary.com/doi/abs/10.12968/nrec.2018.20.2.111
Frisch, N. C., & Rabinowitsch, D. (2019). What’s in a definition? Holistic nursing, integrative health care, and integrative nursing: report of an integrated literature review. Journal of Holistic Nursing, 37(3), 260-272. Retrieved on 29 December 2021 from: https://journals.sagepub.com/doi/abs/10.1177/0898010119860685?journalCode=jhna
Haydon, G., Browne, G. & van der Riet, P., (2018). Narrative inquiry as a research methodology exploring person centred care in nursing. Collegian, 25(1), 125-129. Retrieved on 29 December 2021 from:
health.org.uk (2014), A quick guide to person-centred care, Retrieved on 29 December 2021 from: https://www.health.org.uk/newsletter-feature/a-quick-guide-to-person-centred-care
Kunneman, M., & Montori, V. M. (2017). When patient-centred care is worth doing well: informed consent or shared decision-making. BMJ Quality & Safety, 26(7), 522-524. Retrieved on 29 December 2021 from: https://qualitysafety.bmj.com/content/26/7/522
legislation.gov.uk 1998, Human Rights Act 1998, Retrieved on 29 December 2021 from: https://www.legislation.gov.uk/ukpga/1998/42/contents Mechili, E. A., Angelaki, A., Petelos, E., Sifaki-Pistolla, D., Chatzea, V. E., Dowrick, C., ... & Lionis, C. (2018). Compassionate care provision: an immense need during the refugee crisis: lessons learned from a European capacity-building project. Journal of Compassionate Health Care, 5(1), 1-8. Retrieved on 29 December 2021 from: https://link.springer.com/article/10.1186/s40639-018-0045-7
Mildon, B., (2018). Commentary: Regulation and the Nursing Profession: A Personal Reflection. Nursing Leadership (Toronto, Ont.), 31(3), 34-41. Retrieved on 29 December 2021 from: https://europepmc.org/article/med/30653453
NMC (2018), The Code, Retrieved on 29 December 2021 from: https://www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf Tallon, M. M., Kendall, G. E., Priddis, L., Newall, F., & Young, J. (2017). Barriers to addressing social determinants of health in pediatric nursing practice: An integrative review. journalCodernal of pediatric nursing, 37, 51-56. Retrieved on 29 December 2021 from:
Taylor, A., Lee, H.R., Kubota, A. & Riek, L.D., (2019). Coordinating clinical teams: Using robots to empower nurses to stop the line. Proceedings of the ACM on Human-Computer Interaction, 3(CSCW), 1-30. Retrieved on 29 December 2021 from: https://dl.acm.org/doi/pdf/10.1145/3359323
Trachsel, M. (2019). How to strengthen patients’ meaning response by an ethical informed consent in psychotherapy. Frontiers in psychology, 10, 1747. Retrieved on 29 December 2021 from: https://www.frontiersin.org/articles/10.3389/fpsyg.2019.01747/full
Vincensi, B. B. (2019). Interconnections: spirituality, spiritual care, and patient-centered care. Asia-Pacific journal of oncology nursing, 6(2), 104. Retrieved on 29 December 2021 from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6371669/
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



