OPD Practitioner's Role in Perioperative Environments
Introduction
Anaesthesia & Post Anaesthetic care services in the specially designed anaesthetic care units is the most crucial, sensitive and critical care provision sector in the medical field. The anaesthetic and post-operative services are handled very carefully through the experienced practitioners and not any new care worker can handle the entire situation after any operative or surgical event. The post anaesthetic state is that situation where the patient has undergone any kind of operation or surgery and after that they are shifter to the post anaesthesia care unit where they were kept under observation. Anaesthesia is a process which makes people senseless or unable to move or feel the operative actions going on him/her so that they won’t get affected and feel the pain. This assessment aims at focusing on all the care service requirements regarding the anaesthetic and post-operative care units in the perioperative environment. The role of an OPD practitioner in all the aspects of a post-operative care unit of a patient is deeply covered in this reflective writing, which may benefit from additional healthcare dissertation help to ensure thorough and effective analysis.
Description of the care services provided to patients in the anaesthetic room and post anaesthetic care unit (PACU)
The concepts of the post anaesthesia care unit services includes the postoperative instructions, intra operative medical history, cognitive state, circulatory volume status and the respiratory status regarding to the post-operative patient (Klyukin et al. 2018). The post anaesthesia care unit is that specially designed area where the Post Anaesthesia Recovery (PAR) of the patient is done with medical facilities and appropriate medicinal drugs (Aubrun et al. 2019). The post anaesthesia care unit is not just a ward or a normal place but it is said to contain special equipment set with operating devices. There is needed the presence of post-operative intensive care nurses, care workers and practitioners who are responsible for taking care of those patients who are transferred immediately from the operating room (Bezu et al. 2020). All the facilities are provided according to the standards and guidelines of the Association of Anaesthetists popularly known by the name of Association of Anaesthetists of Great Britain and Ireland (AAGBI) which is professional association of the professional association of Ireland & United Kingdom.

There are five most specific treating aspects of the post anaesthesia care unit listed as - Airway and breathing management, Homeostasis and haemodynamic monitoring, Assessing pain and pain management, Management of post-operative nausea and vomiting and the Discharge planning and criteria. According to Aviram and Samuelly-Leichtag (2017), the ABCDE assessment tool i.e. the Airway, Breathing, Circulation, Disability and Exposure approach is applicable in the emergency clinical situations for the immediate care treatments and intensive assessments of the patients. This approach guides in the anaesthetic and post-operative processes also in treating and handling the patients sensitively in emergency rooms or intensive care units in the perioperative environment.
Airway and Breathing Management
The airway and breathing management service is basically the evaluations and planning of the medical procedures ad devices that are specially used for restoring and maintaining the ventilation and smooth breathing of the post-operative patient. As expressed by Matioc (2019), the airway and breathing services of the PACU includes the acute airway obstruction in the windpipe and the respiratory failure of the patient who have undergone from the general anaesthesia indications. The airway and breathing management process is very critical procedure so for the OPD practitioners it is essential to undergo significant informative lessons, knowledge and rigorous training sessions for being able to handle all kinds of intensive and critical care responsibilities of pre & post anaesthesia care facilities in hospitals & care homes. It is the deep core duty of the OPD practitioners that no little chance also stays there to make any mistake in handling the patients of the perioperative status (ncbi.nlm.nih.gov, 2018). Without proper continuous practice, there will always be a little chance of mishandling or mistake by the practitioners. Although in the extremely complicated situations, highly trained professionals also commits small mistakes (Petkari et al. 2020). In the airways and breathing management setup, the most common side effect is the mild or moderate sore throat situation which stays for a day or two after recovering from the anaesthetic state and later on this status gets better day by day on its own except any unexpected situations or difficulties.
Homeostasis and haemodynamic monitoring
The Homeostasis or haemodynamic monitoring is the blood flow monitoring and can be referred as the assessment where a patient is observed on the circulatory status after the anaesthetic effect. The role of the OPD in the Hemodynamic monitoring in PACU includes the measuring of the intra-arterial pressure, heart rate, pulmonary artery, central venous pressure, blood volume, pulmonary capillary wedge pressures and the cardiac output. Cove and Pinsky (2012) stated that the Hemodynamic monitoring utilises the Homeostasis mechanisms for monitoring and controlling the circulatory system of the autoregulation. As an example of the Homeostasis mechanisms working for the haemodynamic monitoring, the hydraulic circuits can be pointed which are controlled by the continuous control systems. The haemodynamic monitoring and controlling gives responses that are continuously monitoring the patient health status and adjusts according to the conditional changes occurs in the body and the environment where the patient is present (Rodakowski et al. 2017). The basic Hemodynamic monitoring role of the OPD is to take notes of the ECG, non-invasive blood pressure monitoring & the oximetry on a continuous basis. These come under the basic cardiovascular and haemodynamic monitoring whereas the intermediate haemodynamic monitoring includes activities like Electrocardiogram (ECG). Measuring the Electrocardiogram (ECG) during the patient being in the perioperative period lowers the high risks on the patients. OPD uses advanced technologies to utilise the monitoring chances to its full extent on the post-operative patients in PACU (sciencedirect.com, 2018). One of the key aim of the OPD is to keep regular track of the oxygenation in the early period of the haemodynamic imbalance in the patients if occurs.
Assessing pain and pain management
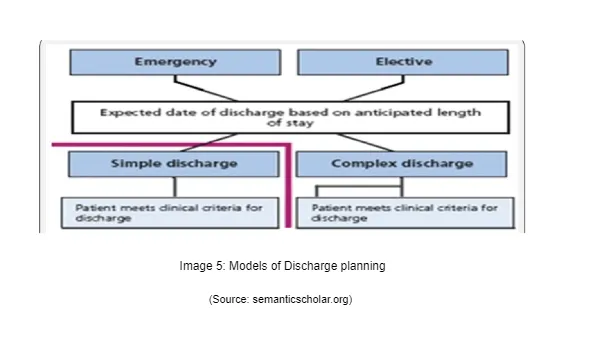
The role of the physician anaesthesiologists has always played the key role while managing the post-operative pain management. The physician anaesthesiologists first meets with the patient before the operation or surgery and assesses about the health conditions of the patients and decides that the anaesthesia care must be accurate and safe and also as effective as possible (Sunwoo et al. 2020). They management the pain by monitoring the vital signals in the patients while the surgery or operation process is going on. These vital signs are like how the heart is responding to the treatment, is the lungs functioning well during the procedure or not and all of these are done when the patient is unconscious and under the anaesthetic effect (Xu et al. 2018). They are equally responsible for the after operative care and comfort also as much as possible. Pains can be mild, severe or excessive, chronic or acute, burning, lancinating, dull or sharp and precisely or poorly localized (Seet et al. 2021). There are specific tools that help the physician anaesthesiologists to measure the pain effect on the patients like Numerical Rating Scale (NRS), Visual Analog Scale (VAS), Wong–Baker Face Pain Rating Scale and the Verbal Rating Scale (VRS) (Sunwoo et al. 2020). These tools read the intensity of the pain through observers and self-report scales which are sometimes used by the patients for self-reporting assessment for pain management.
Management of post-operative nausea and vomiting
The nausea and vomiting symptoms are varied from person to person where some people can be tolerant to the anaesthetic effects of the post the surgical or operative activities. Some people are intolerant and can’t adapt the changes in the body status which comes after the surgical activities in the perioperative environments. Aviram and Samuelly-Leichtag (2017) advised that the nausea and vomiting happens due to the anaesthesia that is applied to the patient in some cases. They patients have been found with symptoms like exhaustion and fatigue in their body and have frequent vomits due to the medical and chemical changes that occurred post the anaesthesia operations. The Post-Operative Nausea and Vomiting (PONV) is majorly triggered by the perioperative stimulations which includes volatile anaesthetics, opioids, adverse drug reactions, anxiety and unnecessary motions. The multiple types of neurotransmitter pathways which are implicated in the human body are the physiological effect that contributes to the nausea and vomiting effects in the patients (Seet et al. 2021).
There are certain factors that contributes to the vomiting and nausea symptoms such as age, specially the female gender, the body mass index (BMI), history of having migraine issues, smoking status of the patient, motion sickness, various type of anaesthesia (specifically the locoregional and the common type) and the most significant is the duration period of the operation or surgery (Seet et al. 2021). Matioc (2019) opined that the side effects of the general anaesthesia including the nausea and vomiting stays for the first few hours after the operative function in general scenario but sometimes it continues to a day or two.
Discharge planning and criteria
Hymel (2019) stated that the pain management as per the research records have been found in perioperative environment patients around 41 per cent who are shifter to the post-operative care units. These types of pains are reported to be either severe or moderate in their nature as felt and shared experiences of the patients. The discharge criteria and planning says that the patients who have been released under the discharging rule and guidelines. The discharge planning of the patients develops with the documentations that was driven by al written and approved information of the recovery status that the nurses or care practitioners suggests and also ensures consistency in the care facilities. The discharge guidelines also incorporates recovery charts which are used to keep track of the patient’s progress from the operating unit to the ward where they were shifted later on after the completion of the operative process. The primary aims of the discharge planning and criteria are:
To make sure that the patient is able to cough, breath, sneeze and do other nasal activities independently or not without any issues or problems.
The respiration level needs to be 10-20 per breaths in the adults with no sudden increasing or decreasing in the process.
Their blood pressure, urination, heart rate & electrocardiogram must be clinically normal and the skin colour and temperature of the patients is also checked before discharge.
Explanation of the care requirements of patients in the anaesthetic room and post anaesthetic care unit (PACU)
All the aspects that are mentioned in the above section are facilities of the PACU and have certain devices and equipment for providing the services to the patients so that the patients can adapt the chemical changes and medications that are given to them after the operative or surgical activities and all these aspects have specific nature in their process (biomedcentral.com, 2018). Every PACU facility has certain set of routine of the post anaesthesia observations which are required for the recognition and assessment of the patient’s medical and clinical deteriorations and improvements in the post-operative period which acknowledges the risk factors, complications and other health matters of the post anaesthetic procedures and surgeries (Brintz et al. 2020). The post anaesthetic care unit aims at –
the continuous monitoring of the cardio-respiratory status
the monitoring of the pulse oximetry device
using the inpatient victor graphs
body temperature, RR, SpO2 observation
vomit and nausea score
sedation status (AVPU, formal GCS records and Michigan sedation score as indicated)
pain status
linking the escalation process of care services with regards to the responses of the abnormal psychological observations (if happens)
All these observations and monitoring are recorded every fixed interval of time period at the early stage and the record duration increase according to the stability level of the patient body in the post anaesthetic care unit (Seet et al. 2021). Finally when the patient is normal in their health condition the discharge criterion planning is initiated.
Airway and breathing management
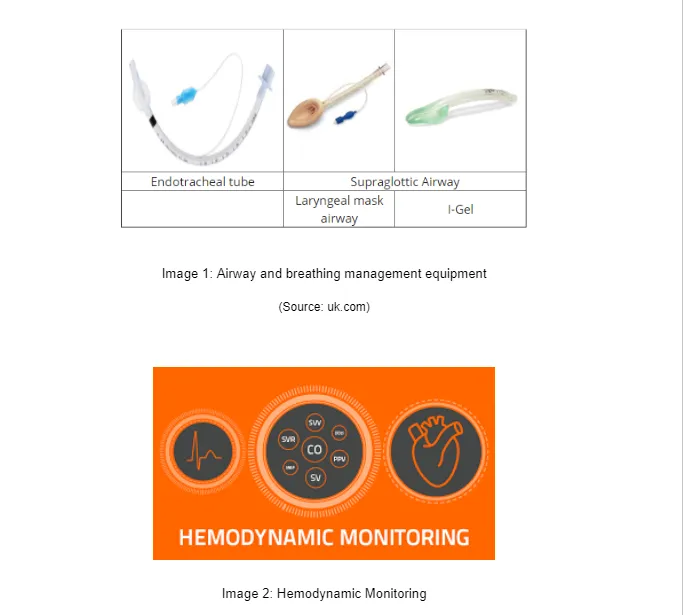
The process of the airway and breathing management is done in the windpipe breathing passage or is regarded with dealing the pathway from where the air passes or flows inside and outside into the lungs of the human body. According to Hymel (2019), the airway and breathing management functions are associated with initiating from the mouth, nose, and travels to the throat, windpipe and follows into the lungs. The equipment or devices used in the airway and breathing management are the Endotracheal tube, Laryngeal mask airway, I-Gel and the Supraglottic Airway (Klyukin et al. 2018). These devices are specially inserted in to the patients’ body when the patient is asleep or under the anaesthetic effect so that the insertion pan could not be felt by them. The immediate insertion of the airway and breathing devices are must in every aspect so that whenever the patient awakes, the instant and quick monitoring can be started and recorded within the fixed time intervals. Though there are some side effects also present in the breathing and airway management like damages in teeth, bleeding mouth or gums, damage in lips or nose, swelling in the windpipe, difficulty in opening mouth, moving of neck and sometimes they include brain damages and death due to starvation of oxygen (biomedcentral.com, 2018). These can be avoided with qualified and highly trained care workers and PACU professionals.
Continue your exploration of Online Audit of Surveys on Effects and Dangers of Non-Compliance with our related content.
Homeostasis and haemodynamic monitoring
The primary objective of the Hemodynamic monitoring with the Homeostasis mechanism is to keep ensuring that the oxygen delivery and the optimal tissue perfusion is properly maintained with the adequate status of the mean arterial blood pressure. The Hemodynamic monitoring keeps regular measurements of the detailed cardiac and also the intravascular pressure statuses and their volume levels that are interpreted directly to the therapeutic plan of the patient care (ncbi.nlm.nih.gov, 2019). The Hemodynamic monitoring observes and reflects the physiologic homeostasis and allows the appropriate prompt recognitions of the responses of all the therapeutic interventions of the overall post anaesthetic care unit processes. The basic and standard Hemodynamic monitoring and the Homeostasis mechanism equipment are the Capnography, Echo Cardio-graphy, Pulse Oximetry, body temperature and the Systemic Blood Pressure flow (Seet et al. 2021).
The hemodynamic and haemostasis monitoring includes the inspections of the skin where the capillary refill is normal or delayed is suggested and if found delayed then it can be considered as abnormal systematic circulation. The palpation of the pulse, skeleton muscle and skin is checked that whether they are warm or cold or clammy and is the pulse present or absent with checking of proper muscle fasciculation. The nail beds, surgical area, eyes, bodily movements and mucus membranes are regularly checked while the patient is in the post anaesthetic care unit (Sinha et al. 2020). In this regards, the ABCDE approach provides help for rapidly detecting and recognising the immediate need of assistances such as cardiac arrest team, medical emergency team and so on. This ABCDE approach has been helpful in reducing the problems and issues that arise during the anaesthesia and post anaesthetic effects.
Assessing pain and pain management
The post-operative or surgical pain has different dimensions and is of various types in various locations and types of sensations that the patients feel, all these can be described as:
Nociceptive-visceral pain is the first type whose location places are in all the visceral organs where this pain is being felt by the patients. The quality of pain felt kind of deep aching or sharply stabbing type of sensation (biomedcentral.com, 2018). The primary sources of this pain are like the Ischemia, muscle spasm, organ distension and inflammation. The examples which can be suggested are like Pancreatitis, gastric ulcers, appendicitis and bladder distensions.
Neuropathic pain is also another type of pain which happens in places like in the kinds of peripheral organs of the body. The pain is basically the type of aching, sensitivity, burning, sensations, shock, cramps, numbness, tingling and shooting type. The primary sources are lesions, peripheral nerve damages, trauma, compressive, circulatory, impairment, CNS disease and metabolic sources. Few instances of this type of pain are like neuropathy, diabetic, carpel tunnel syndrome, fibromyalgia, neuralgia, post-stroke, phantom limb pain and multiple sclerosis (sciencedirect.com, 2017).
Nociceptive-somatic pain is the third and last type of pain which happens due to the tissues, skin, muscles, bones and joints of the human body. This pain can be described by giving examples like burns, cuts, surgery, contusions, tendonitis and arthritis (biomedcentral.com, 2018). The quality of sensation occurs in this pain is like symptoms of burning, dull, sharp, cramping and aching type. And the main sources are like strain, injury, any traumatic incident, dermatological, inflammation and ischemia type of feelings which is felt by the patients after the operative actions and during the operative actions also if anaesthesia is not used (biomedcentral.com, 2018).
Other than these, there are two main categories of pain that are – acute and chronic, where acute is minimal in nature and the chronic is the highly sensitive in nature of the pain that patients feel post the operative action. According to the guidelines showed by the American Society of Anaesthesiologists, it is essential and important to have regular routine assessments and proper monitoring of all types of pain that can be detected with the complications and all of them must be reduced without any adverse effects.
Management of post-operative nausea and vomiting
The most effective way to manage the post-operative nausea and vomiting is to apply various types of drugs that are used in the management of the Post-Operative Nausea and Vomiting issues (Klyukin et al. 2018). Another way is to give frequent IV fluids to the patients in perioperative care environment if he/she is feeling dehydrated. The post-operative nausea and vomiting is considered to be the reasons behind the failure of prophylaxis or due to the lack of proper primary treatment after the post-operative intensive care facilities and services. The prophylaxis process needs to be given in the PACU within 24 hours of the post-operative process. Another way is to use the opioid analgesics while the perioperative period is going on to prevent the post-operative nausea and vomiting issues. The main causes of the post-operative nausea and vomiting are medications, dehydration, and empty stomach after the surgical or operative activities, an overly aggressive returning back to the regular and normal diet and lastly the factors also include the lack of preventative vomiting & nausea medications (Brintz et al. 2020).
The post-operative nausea and vomiting is said to be one of the most complex and significant issues while treating the anaesthesia and post-operative practices. PONV is basically influenced by the multiple factors where all of them are related to the patients undergone through any surgery or operation with anaesthesia effects (Klyukin et al. 2018). Few very restrictions are in this scenario is no smoking or alcoholic intake because these can make the patient more nausea tic and vomiting can be increased too with more adverse effects (Rodakowski et al. 2017).
Discharge planning and criteria

The proper and accurate discharge plan as per the guidelines of the Association of Anaesthetists of Great Britain and Ireland (AAGBI) declares that the discharge criteria and planning must be capable of fulfilling all the needs in their exact places in all types of recovery units (Sinha et al. 2020). The discharge planning and criteria must ensure that the patients are discharged safely towards the surgical wards. The discharge plans must provide all the practical guidance and the required advices to those staff members and care workers who are responsible for taking care of the patients who are in immediate postoperative period state. The aim of the Anaesthetists of Great Britain and Ireland (AAGBI) discharge planning and criteria of the Post-Operative Care Unit (PACU) is to maintain the high care standards in a consistent way reflecting the objectives of the NHS Plan also (Sunwoo et al. 2020). The patients should respond towards the verbal stimulations for being able to answer appropriately the questions asked and be oriented in their surroundings. One most vital noticing task is to track that whether the patient is having adequate gas exchange in the post-operative care unit or not & before discharge the patient must maintain his/her own airway and can breath and cough deeply without any problem.
Conclusion
The conclusion of this reflective assessment primarily represents the role of OPD practitioners in the pre and post anaesthetic care units which is a vital area of the hospital premises. The post anaesthesia care unit is not just a ward or a normal place but it is said to contain special equipment set with operating devices. Every PACU facility has certain set of routine of the post anaesthesia observations which are required for the recognition and assessment of the patient’s medical and clinical deteriorations and improvements in the post-operative period which acknowledges the risk factors, complications and other health matters of the post anaesthetic procedures and surgeries. And lastly it can be concluded that the role of OPD in every segment whether it is the airway and breathing management, the post-operative nausea and vomiting management, pain management or in the discharge planning and haemodynamic monitoring is very crucial in its place and must be maintained carefully and sensitively.
References
Aubrun, F., Ecoffey, C., Benhamou, D., Jouffroy, L., Diemunsch, P., Skaare, K., Bosson, J.L. and Albaladejo, P., (2019). Perioperative pain and post-operative nausea and vomiting (PONV) management after day-case surgery: The SFAR-OPERA national study. Anaesthesia Critical Care & Pain Medicine, 38(3), pp.223-229.
Aviram, J. and Samuelly-Leichtag, G., (2017). Efficacy of Cannabis-Based Medicines for Pain Management: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Pain Physician, 20(6), pp.E755-E796.
Bezu, L., Raineau, M., Deloménie, M., Cholley, B. and Pirracchio, R., (2020). Haemodynamic management during hyperthermic intraperitoneal chemotherapy: A systematic review. Anaesthesia Critical Care & Pain Medicine.
biomedcentral.com, (2018). Improved analgesia and reduced post-operative nausea and vomiting after implementation of an enhanced recovery after surgery (ERAS) pathway for total mastectomy, available at: https://bmcanesthesiol.biomedcentral.com/articles/10.1186/s12871-018-0505-9
Brintz, C.E., Roth, I., Faurot, K., Rao, S. and Gaylord, S.A., (2020). Feasibility and acceptability of an abbreviated, four-week mindfulness program for chronic pain management. Pain Medicine, 21(11), pp.2799-2810.
Cove, M.E. and Pinsky, M.R., (2012). Perioperative hemodynamic monitoring. Best practice & research Clinical anaesthesiology, 26(4), pp.453-462.
Hymel, N.D.M., (2019). The Development Of An Evidence-Based Anti-Emetic Tool For The Management Of Post-Operative Nausea And Vomiting In Patients At High Risk For Qt Prolongation And Patients Taking Neurotransmitter Modulating Medications.
Klyukin, M.I., Kulikov, A.S. and Lubnin, A.Y., (2018). THE PROBLEM OF POST-OPERATIVE NAUSEA AND VOMITING IN THE PATIENTS UNDERGOING NEUROSURGERY. Messenger of ANESTHESIOLOGY AND RESUSCITATION, 14(4), pp.43-51.
Matioc, A.A., (2019). An Anesthesiologist’s Perspective on the History of Basic Airway Management: The “Modern” Era, 1960 to Present. Anesthesiology, 130(5), pp.686-711.
ncbi.nlm.nih.gov, (2017). Moving Beyond Pain as the Fifth Vital Sign and Patient Satisfaction Scores to Improve Pain Care in the 21st Century, available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5878703/
ncbi.nlm.nih.gov, (2018). Haemodynamic Monitoring Devices in Heart Failure: Maximising Benefit with Digitally Enabled Patient Centric Care, available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6304789/
ncbi.nlm.nih.gov, (2019). Alternatives to Rapid Sequence Intubation: Contemporary Airway Management with Ketamine, available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6526883/
Petkari, E., Kaselionyte, J., Altun, S. and Giacco, D., (2020). Involvement of informal carers in discharge planning and transition between hospital and community mental health care: A systematic review. Journal of Psychiatric and Mental Health Nursing.
Rodakowski, J., Rocco, P.B., Ortiz, M., Folb, B., Schulz, R., Morton, S.C., Leathers, S.C., Hu, L. and James III, A.E., (2017). Caregiver integration during discharge planning for older adults to reduce resource use: a metaanalysis. Journal of the American Geriatrics Society, 65(8), pp.1748-1755.
sciencedirect.com, (2017). Providing chronic pain management in the “Fifth Vital Sign” Era: Historical and treatment perspectives on a modern-day medical dilemma, available at: https://www.sciencedirect.com/science/article/pii/S0376871617300030
Seet, E., Nagappa, M. and Wong, D.T., (2021). Airway management in surgical patients with obstructive sleep apnea. Anesthesia & Analgesia, 132(5), pp.1321-1327.
Sinha, V., Vivekanand, D. and Singh, S., (2020). Prevalence and risk factors of post-operative nausea and vomiting in a tertiary-care hospital: A cross-sectional observational study. Medical Journal Armed Forces India.
Sunwoo, B.Y., Light, M. and Malhotra, A., (2020). Strategies to augment adherence in the management of sleep‐disordered breathing. Respirology, 25(4), pp.363-371.
Xu, Z., Ma, W., Hester, D.L. and Jiang, Y., (2018). Anticipated and unanticipated difficult airway management. Current opinion in anaesthesiology, 31(1), pp.96-103.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



