The Impact of Work on Health
The Impact of Work on Health
Work has received and continues to receive growing attention due to its importance to man both socially and economically. The primary function of work is the production and distribution of goods and services. While work is a powerful force that plays a psychological role in shaping a person’s life, self-esteem, and routines (daily, weekly, monthly, annually), little attention has been accorded to it in terms of its importance to individuals. Even though the positive effects of work on the health of individuals is yet to be fully exploited, numerous adverse and hazardous impacts of work on health have been identified. This paper, therefore, seeks to examine the various diseases or illnesses and injuries that may occur to an individual as a result of their occupations. These are referred to as occupational diseases. The World Health Organization defines an occupational disease as that which arises from or in the course of a person’s employment, and which are caused majorly by the type of work they do. Work affects people’s health in two major ways: it puts them at a health risk through specific activities, and excess work will cause one to suffer physically and mentally. A 2016 Labor Force Survey estimated that about 1.3 million people who had worked between 2015 and 2016 suffered from conditions they believed resulted from or worsened as a result of the work they did. This issue also highlights the need for healthcare dissertation help to further investigate the intersection of work and health. RIDDOR (Reporting of Injuries, Diseases and Dangerous Occurrences Regulations, 2013) classifies some of these diseases as reportable, and they include:
Occupational Asthma
Asthma causes patients to suffer from shortness of breath. Although numerous substances found outside the work environment are known to cause asthma, several work exposures have also been linked to its occurrence. While occupational asthma is the most common occupational lung disorder and is prevalent in industrialized nations, it usually presents the symptoms of classic bronchial asthma such as cough, tightening of the chest, wheezing, and difficulty breathing. Work exposures may cause a new occurrence of asthma or cause previous latent childhood asthma to recur. Occupational asthma accounts for nearly 15% of new cases of asthma among adults (Tarlo, 2014; Beach et al., 2017; Baur et al., 2012), with a 2018 survey of over 200000 patients pointed to an approximated 1.9 million new occupational asthma cases (Center for Disease Control and Prevention, 2018). Occupational asthma has been found to cause nearly 38000 deaths and approximately 1.6 million life-years in disability adjustment every year (Tarlo, Liss, and Blanc, 2016). The triggers for occupational asthma have been identified and are more than 250000 (Beach et al., 2017). The common triggers including chlorine; respiratory sensitisers like solder fumes, flour, and high-level irritant wood dust; smoke; dust from flour, cereals or grain; fungal spores; gum arabics; platinum salts; antibiotics; tuleone diisocyanates; animal feeds or bedding, airborne substances from welding or grinding of metals. Sensitisers are substances that bring about an immune-mediated response and are claimed to be responsible for 90% of most cases. In contrast, irritant- substances that cause direct cell damage and inflammation even without sensitisers- are responsible for 10% of the occupational asthma cases (Tarlo, Liss and Blanc, 2016). These sensitisers may be classified as high-molecular or low-molecular-weight sensitisers. The CDC and National Institute for Occupational Safety and Health propose specific controls to mitigate the impact of this disease, causing hazards on employees. Where possible, these hazards should be removed entirely (eliminated) from the work environment, or the employees should avoid exposure to the hazardous agents. If this is not possible, the management should replace or find a substitute for the hazard or come up with engineering controls to keep the workers away from the threat.

Occupational Chronic Obstructive Pulmonary Disease (COPD)
Research attributes 15% occupational COPD, which is ranked the fourth leading course of global deaths, to occupational exposures. The National Health and Nutrition Examination Survey (Hnizdo, Sullivan, Bang and Wagner, 2015) found that several exposures caused nearly 19% of all occupational COPD; 31% of those were non-smokers. The major attributable causes of occupational COPD are gases, specks of dust, fumes, and nonspecific gases, although most cases are attributed to dust (Mastrangelo et al., 2013). This type of occupational illness is common among people working in coal mines or those exposed to cotton dust, silica, and cadmium fumes. Simultaneous exposure of these workers to cigarette smoke produces a synergistic effect, which makes them more vulnerable to COPD than they would be if they were just subjected to more risk of the exposures alone (Diaz-Guzman, Aryal, and Mannino, 2012). A recent study conducted concluded that the risk of COPD was higher among people aged 65 years, smokers and people exposed to the causal agents for increased periods. Occupational COPD first presents with breathlessness, then coughing and wheezing before progressing to fixed obstruction if not managed. The primary preventive measures proposed for COPD include identifying the causal agent and eliminating it, using personal protective gear to avoid exposure to these hazards as well as using a symptoms questionnaire for medical surveillance as a secondary preventive measure (Diaz-Guzman, Aryal, and Mannino, 2012; Boschetto et al., 2016).
Occupational Dermatitis (Contact Eczema)
Contact eczema occurs when a chemical or hazardous substance penetrates the upper layers of the epidermis- which is meant to protect the skin. The most common cause of this disease is working with wet hands and working with soaps or cleaning agents. Occupational contact dermatitis can be classified as either irritant or allergic-type. Irritant contact dermatitis refers to the inflammation that arises from phototoxic reactions or as a result of the skin coming into contact with chemicals like acids, detergents, bases, and reducing agents. In contrast, allergic contact dermatitis occurs due to an allergic skin reaction from exposure to certain metals, acrylic resins, agrochemicals, rubber additives, and commercial chemicals. Although the causes of the two types may vary, some causal agents have been found to bring about both. Occupational dermatitis or skin exposures rank second among the most common causes of occupational disorders, give that it affects about 3 in every 10000 workers (Bureau of Labor Statistics, 2014). Chemicals that can be taken in through the skin potentially expose up to 13 million workers to occupational dermatitis (Carøe, Ebbehøj, and Agner, 2014). However, several European countries have witnessed a reduction in the number of occupational dermatitis cases that are reported. Occupational contact dermatitis has been found to contribute to 90-9% of occupational skin illnesses. Hand eczema, which affects mostly hairdressers, florists, and beauticians, presents itself as swollen, flaking, dry and fissuring, or erythematous, blistering, and erosions. Whereas the illness can arise at any stage of the person’s career, it takes different clinical courses in different people. One-third of those affected usually have their symptoms revolve, another one-third show partial improvement even though symptoms persist, a quarter of the patients show no changes.
In contrast, a few may have their symptoms worsen. The CDC and National Institute for Occupational Safety and Health advise the implementation and use of the set hierarchy of controls alongside other preventive control programs such as avoidance of the irritants or allergen, the substitution of the hazardous agent for a safer alternative, limitation of glove use, use of cotton liners in cases of prolonged glove use, encouraging the use of alcohol-based hand sanitizers especially for health care workers, avoidance of pre-work creams, frequent application of post-work fragrance-free creams and implementation of various engineering controls- automation, use of personal protective equipment and ventilation (Adisesh, 2013; Nicholson, Llewellyn, and English, 2010). Pre-work creams are discouraged because they usually tend to result in other preventive measures being complacent and, therefore, ineffective.
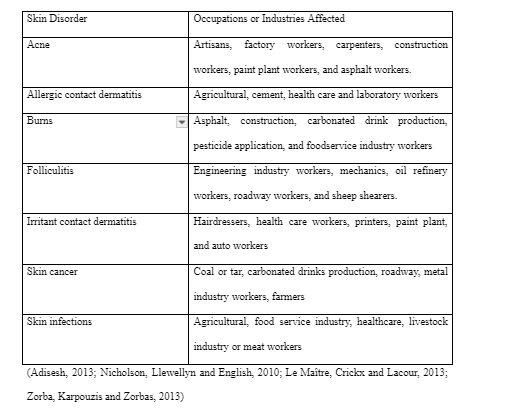
Below are some of the most common types of occupational skin disorders and the occupations most affected by them:
Occupational Musculoskeletal Disorders
These are injuries that affect the tendons, muscles, cartilage, joints, and nerves and which result from or are worsened by sudden movements or increased periods of force, awkward positions, repetitive movements, or vibrations. These injuries are also brought about by postures that must be maintained for extended periods, occasional bending, twisting, nursing, and policing. Most occupational musculoskeletal disorders affect the upper part of the body and include lateral epicondylitis, sprains, muscle tears, shoulder disorders, wrist tendinitis, carpal tunnel syndrome, hernias, and back pains. Research findings revealed that occupational musculoskeletal disorders contributed to approximately 38% of all occupational illnesses and injuries (Gerr, Fethke, and Merlino, 2014). While most occupations such as dock workers, heavy manual workers, material handlers, and miners are at risk of occupational musculoskeletal disorders, nearly half of those affected are people who worked in either the manufacturing or service industry (Descatha, Leclerc, Chastang and Roquelaure, 2013). Several determinant factors have been found to exacerbate the risk of occupational musculoskeletal disorders: congenital back defects, weak musculature, degenerative spine, and intervertebral discs, and rheumatic affection. Various safeguarding measures against occupational musculoskeletal disorders have been recommended. These include workplace adaptation, removal of the hazard, engineering controls that change factors of fixed body positions, controlling the force applied, speed of work and sudden movements, and administrative controls- job rotations, breaks, alterations of working speeds- that protect workers at risk.
Contagious Diseases
These are diseases that are easily passed from one person to another. Health workers of all types are the people most at risk of contracting these contagious diseases such as tuberculosis in the course of handling patients who are already infected by them. Activities such as blood testing and operating biological specimen expose the health workers to an even greater risk of contracting blood-borne diseases like Hepatitis B, Hepatitis C, and even HIV.
As a preventive measure, health workers- doctors, nurses, dentists, and so on, are advised to wear gloves when dealing with patients or when handling blood samples and appropriately handling and disposing of used needles.
Work-related Pulmonary Diseases or Respiratory Conditions
These are illnesses arising from inhaling harmful agents that are biological in nature, chemicals, gases, vapors, dust, or fumes. Pulmonary and lung diseases are a broad group of conditions that affect millions of people worldwide. While smoke, gas, dust, and fumes may affect the breathing system, tobacco smoking has been identified as the primary cause of preventable lung diseases or cancer. However, about 1-20% of lung diseases have been attributed to various occupational exposures. Examples of some occupational respiratory illnesses include silicosis, pneumonitis, asbestosis, rhinitis, pharyngitis, reactive airways dysfunction syndrome (RADS), beryllium disease, hypersensitivity, and other pneumoconioses. Miners are especially at a higher risk of developing silicosis and coal workers pneumoconiosis and other lung diseases such as cancer following extended periods of exposure to stone dust. Miners who develop silicosis are at an even greater risk of other infectious diseases like tuberculosis. The miners and coal workers blasting operations and mechanical mining processes
like drilling, barring, tipping, scraping, lashing, and loading produces large volumes of dust that expose both underground and surface workers to these airborne respiratory illnesses.
Pesticide Intoxications
Agricultural activities are an effective support system for the economies of developing countries. As a result, there has been increased use of chemical pesticides in the last few years. These pesticides, which are meant to kill and mitigate pests to increase yields, however, pose a severe health risk for many workers in those countries. The pesticides may be composed of biological or chemical agents who put their sprayers at increased intoxication risk levels should the failure to handle these toxic pesticides with care arise. The World Health Organization (WHO), while approximately 1.3 billion agricultural workers are exposed to intoxications annually, 60% of these cases are found in developing countries. The International Labor organization, on the other hand, suggests that a minimum of half a million acute poisonings occur globally each year, with about 9ooo of them being lethal. While the above statistics cover only the agricultural workers (the pesticide sprayers and farmers), those who manufacture these substances, as well as the farm supervisors and managers, could also be exposed to these hazardous chemicals. The airborne exposure by spraying using airplanes and contamination of water sources also affect the people living around these farms. Workers who develop these intoxications usually get them through; inhalation of the air containing these chemicals, peroral intake (mostly by unknowingly drinking them); and through the skin.
Preventive measures that could be taken include adopting safer pest control methods or substances, wearing of protective equipment when spraying pesticides, labeling pesticide bottles to prevent people from accidentally drinking them.

Continue your journey with our comprehensive guide to The Impact of Vitamin E, Fish Oil, and Protein Supplements.
References
- Adisesh A, Robinson E, Nicholson PJ, Sen D, Wilkinson M., 2013. Standards of Care Working Group. U.K. standards of care for occupational contact dermatitis and occupational contact urticaria. Br J Dermatol, 168(6):1167–1175.
- Baur, X., Bakehe, P., Vellguth,H., 2012. Bronchial asthma and COPD due to irritants in the workplace - an evidence-based approach. J Occup Med Toxicol, 7(1):19.
- Beach, J., Russell, K., Blitz, S., 2017. A systematic review of the diagnosis of occupational asthma. Chest, 131(2):569–578
- asthma. Chest, 131(2):569–578 Boschetto, P., Quintavalle, S., Miotto, D., Lo Cascio, N., Zeni, E., Mapp, C.E., 2016. Chronic obstructive pulmonary disease (COPD) and occupational exposures. J Occup Med Toxicol, 1:11.
- Bureau of Labor Statistics, 2014. U.S. Department of Labor. Employer-reported workplace injuries and illnesses. http://www.bls.gov/news.release/pdf/osh.pdf. Accessed 12 May 2020.
- Carøe TK, Ebbehøj N, Agner T., 2014. A survey of exposures related to recognized occupational contact dermatitis in Denmark in 2013. Contact Dermatitis, 70(1):56–62.
- Centers for Disease Control and Prevention, 2018. Work-related asthma–38 states and District of Columbia, 2010–2016. MMWR Morb Mortal Wkly Rep, 61(20):375–378. Cullinan, P., 2012. Occupation and chronic obstructive pulmonary disease (COPD). Br Med Bull, 104:143–161.
- Descatha, A., Leclerc, A., Chastang, J.F., Roquelaure. Y., 2013. Study Group on Repetitive Work. Medial epicondylitis in occupational settings: prevalence, incidence and associated risk factors. J Occup Environ Med, 45(9):993–1001.
- Diaz-Guzman, E., Aryal, S., Mannino, D.M., 2012. Occupational chronic obstructive pulmonary disease: an update. Clin Chest Med, 33(4):625–636. Gerr, F., Fethke, N.B., Merlino, L., 2014. A prospective study of musculoskeletal outcomes among manufacturing workers: I. Effects of physical risk factors. Hum Factors, 56(1):112–130.
- 56(1):112–130. Hnizdo, E., Sullivan, P.A., Bang, K.M., Wagner, G., 2015. Association between chronic obstructive pulmonary disease and employment by industry and occupation in the US population: a study of data from the Third National Health and Nutrition Examination Survey. Am J Epidemiol, 156(8):738–746.
- Survey. Am J Epidemiol, 156(8):738–746. Holness, D.L., 2013. Recent advances in occupational dermatitis. Curr Opin Allergy Clin Immunol, 13(2):145–150 Le Maître, M., Crickx, B., Lacour, J.P., 2013. Validation of a clinical evaluation score for irritative dermatitis: SCOREPI. J Eur Acad Dermatol Venereol, 27(9):1138–1142. Lewis, L., Fishwick, D., 2013. Health surveillance for occupational respiratory disease. Occup Med (Lond), 63(5):322–334.
- Mastrangelo, G., Tartari, M., Fedeli, U., Fadda, E., Saia, B., 2013. Ascertaining the risk of chronic obstructive pulmonary disease in relation to occupation using a case-control design. Occup Med (Lond), 53(3):165–172.
- Nicholson, P.J., Llewellyn, D., English, JS., 2010. Guidelines Development Group. Evidence-based guidelines for the prevention, identification and management of occupational contact dermatitis and urticaria. Contact Dermatitis, 63(4):177–186. Tarlo, S.M, Lemiere, C., 2014. Occupational asthma. N Engl J Med, 370(7):640–649.
- Tarlo, S.M., Liss, G.M., Blanc, P.D., 2013. How to diagnose and treat work-related asthma: key messages for clinical practice from the American College of Chest Physicians consensus statement. Pol Arch Med Wewn, 119(10):660–666.
- Van Eerd, D., Munhall, C., Irvin, E., 2016. Effectiveness of workplace interventions in the prevention of upper extremity musculoskeletal disorders and symptoms: an update of the evidence. Occup Environ Med, 73(1):62–70.
- Zorba, E., Karpouzis, A, Zorbas A., 2013. Occupational dermatoses by type of work in Greece. Safe Health Work, 4(3):142–148.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



