Safeguarding Vulnerable Adults under the Care Act
How different legislation impact the PCC:
Health and safety and safeguarding are the two important system in health and social care that ensure the promotion of health as well as wellbeing through providing PCC and protection of every service user from any harm (Carayon, 2016)). There are several legislation and policies on health and safety and safeguarding that reflect on the provision of PCC.
Under the Care Act 2014: Safeguarding Adults, sets the highly effective legislative framework that makes it obligatory for the local health and social care authorities and other parts of this system to work together to ensure the safeguarding of vulnerable adults in relation to provide PCC to them (Valentine et al. 2015). Under Care Act 2014, the local health and social care authority must protect adults from any kind of abuse, harm and neglect. This act makes it mandatory for local healthcare officials and authority to run a multiagency adult safeguarding system that must prevent the neglect and abuse in the society towards vulnerable adults.
The Care act 2014, also emphasizes on establishing the Adult Safeguarding Board (ASB) in locality which will include local health and social care authority, police ad NHS for developing, sharing and implementing effective safeguarding strategies (Zingg et al. 2015).
Under Health and safety at Work act 1974 or HASAWA sets outs principles that caregivers must implement while for maintaining workplace safety v while proving PCC to patients. under this health and safety regulation, while providing PCC to services users, care givers must ensure that they use the right techniques and equipment’s in terms of safety of their clients as well as colleagues.
Under Workplace (Health, Safety and Welfare) Regulations 1992, in terms of providing the high quality PCC to service users, healthcare authority must ensure that there is proper safety framework for both care providers and service users in terms of avoiding risk of any kind of hazards (Singh and Graber, 2015). Under this act the local health and social care authority must ensure that, all the care givers are properly trained and skilled in terms of handling and managing the safety equipment and process to ensure effective personalised care to patients.
The safeguarding vulnerable group act 2006 sets out principles for all local healthcare authority, voluntary and statuary health and social care agencies for developing such a PCC framework which will protect each vulnerable adult from any kind of harm of abuse (Hall, et al. 2016). Under this act, while providing the personalised care to vulnerable adults, care givers must determine the risk factors that are associated with the safety and health needs of vulnerable adult (Bigi, 2016). Under this act, health and social care staffs work together with local authority to empower vulnerable adult through providing them effective person centred care (PCC) under which self-management skill will be developed in them for making them independent in terms of dealing tier own health needs (Sweeney et al. 2015).
The safeguarding Strategy 2019 to 2025 is developed in the UK for implementing the principles set under the Care at 2014 and Social Services and Wellbeing Act (Wales) 2014 for ensuring safeguarding for vulnerable adults and children (Sweeney et al. 2015). Under this strategy, PCC will be deliver to vulnerable adults and children in relation to meet their safety needs along with meeting their health needs. Care givers must check whether there is any sign of any kind of abuse, harm neglect, physical assault, and discrimination and mental harassment.
Problems that occur while implementing legislation for providing PCC:
While implementing the above-mentioned legislation and acts for providing an effective PCC, services providers’ can face different challenges (Valentine et al. 2015). Lack of skill and professional knowledge of service providers regarding the legislation the major problem in terms of implementing these legislation in delivery of PCC. As mentioned by Carayon (2016), while it comes to implement the policies and provision for providing a high quality PCC, care givers must have clear understanding on the health and safety and safeguarding acts and legislation. In this regard, the lack of professional knowledge, and skill of care givers regarding the principles of safeguarding acts and health and safety legislation makes it difficult for them to maintain their professional accountability and integrity towards their clients while providing PCC.
Another challenge that caregiver often face regarding implementing legislation in delivery of PCC is the poor interaction and communication with patients and colleagues. As mentioned by Valentine et al. (2015), the quality of PCC is dependent on how effectively all the health and safety and safeguarding legislations are implemented into practices for meeting personalised health and safety needs of patients. Many nursing professional and healthcare staffs do not have excellent communication skill, which makes it difficult for them to determine the safety and health needs their patients (Zingg et al. 2015). Lack of transparent information delivery with colleagues makes it difficult for caregivers to discuss the process of implementing legislations, get reviews from each other regarding improving the PCC by complying with the provision.
The unhealthy competition and team conflict are het potential problem that makes a multidisciplinary team to fail to implement the effective legislation and acts regarding delivering high quality PCC (Singh and Graber, 2015). In modern health and social care system, care givers work in multidisciplinary team I which they work with diverse team members, which enhances the risk of unhealthy competition among them. There are also risk of severe opinion mismatches, argument and disagreement regarding the compliance of legislation and acts in relating to delivery PCC.

Challenges that health professional face during interpreting legislation during provision and planning of PCC in own setting:
In my practice as a senior caregiver I have faced many challenges in terms of implementing different legislations during the provision and planning of PCC. The first challenge that I faced in this regard is the lack of training nod skill development opportunities in my workplace for improving my understating regarding implementing and interpreting of different legislation regarding delivering PCC. As mentioned by Singh and Graber (2015), healthcare authority must conduct effective training and development program for caregivers which will enable them to be involved in a continuous professional development (CPED), CPD is important for caregivers to improve the knowledge and understanding regarding how the different legislation can be implemented into practices for developing effective care plan for PCC. Another challenge that I have faced is poor task delegation process in my workplace, which pose overburden of work on me, that makes me unable to manage times for maintain an effective implementation of appropriate legislation regarding delivery of PCC. On the contrary Hall, et al. (2016) argue that, although task delegation is an important issues in health and safety framework, caregivers must develop an excellent time management skill for managing enough times to implement and interpret appropriate legislation for delivering high quality PCC to their clients. In my workplace, due to shortage of staffs, I have to do many tasks regarding care delivery which sometimes make me unable to comply with all the principles and legislation regarding PCC. Poor cooperation from service users is the major challenge that I face while complying with legislation of PCC in relation to promote health and safety of patients. As mentioned by Dudeck et al. (2015), while it comes to provide a high quality PCC to client it is also important that caregivers would receive the proper cooperation from the patients regarding obtaining the information regarding the medical condition, pervious medical history and the health needs of the patients. During my practices with critical patients, many times I face difficulties in obtaining the proper support and cooperation from patients and their family members regarding providing the clear information that are required for delivery PCC.
Strategies for complying with legislation f PCC:
While it comes to promote health and safety ad safeguarding for patients regarding providing the high quality PCC to them (Dudeck et al. 2015). Caregivers must use appropriate strategies for complying with all the legislation regarding PCC. First of all, an effective communication framework is highly crucial for complying with all legislation and regulation of PCC, in relation to promote health and safety of patients. In this context, caregivers must maintain a healthy and effective communication with patients and colleagues, thereby maintaining good information delivery (Couët et al. (2015). An effective information deliver within team, will enable, team ,embers to discuss and share information regarding how to implement and comply with all legislation of PCC thereby promoting health and safety and safeguarding of patients. Another important strategy is conducting Continuous professional development (CPD) training for caregivers which will enable them to improve their professional knowledge and skill in interpreting ad implementing all the legislation ad principles regarding PCC thereby meeing health and safety needs of services users.
Reflective log book:
Scenario 1: Give a brief description of the patient or service user or individual in need that you have provided person-centred care to:
During my practice as a senior care giver I was assigned to take care of a patient with complex health condition. The patient suffered from COPD (chronic obstructive pulmonary disease) and diabetes type 2. The patient had been admitted to the emergency ward with shortness of breathing and chest pain. After assessing patient’s health condition and the previous medical history it was seen that the patient had been suffering from COPD and type 2 diabetes since 5 years. These two chronic health conditions posed adverse impacts on patient’s mental and physical health. The patient lived alone with a community care nurse who took care of her from morning to night. While admitting to the emergency ward the patient had an oxygen saturation of 85% (normal in COPD patients is 95-98%) and the blood glucose level was 250 mg/dL (normal is 120 mg/dL). After admission to the emergency ward the patient was supported with nebuliser for improving the breathing condition. In the nebuliser SABA and LAMA medicines are used. SABA and LAMA are two bronchodilators which are used to treat COPD patients. These two medicine worked directly on the airways and cause dilatation of bronchioles thereby letting more air (oxygen to pass through e airways towards long thereby improving the breathing condition. Immediate after the admission, the ABCDE (airways, breathing, circulation, disability and exposure) health assessment had been done for checking the physiological health condition of patients.
How to provide person centred care by considering different key principles:
How to provide person centred care by considering different key principles: While providing Person Centred Care (PCC) to the above-mentioned patients I have considered different important aspects such as patient’s dignity, autonomy, coordinated care delivery, effective support to patient and personalised care delivery to patients (Scales et al. 2017). I ensured that the major principles of PCC are maintained throughout the care delivery to this patient. During taking care of this patients, I respected the choices, autonomy and preference of this patient. I ensured that I provide the compassionated care to this patient by protecting patient’s right to confidentiality. In this context, I complied with all the guidelines and principles of general data protection act (2018) for ensuring that all the professional and personal detail of the patient are maintained with proper confidentiality thereby avoiding a risk of unauthorised access (Kortteisto et al. 2018). I ensured that, the treatment and health related information and all the personal details of the patient is not shared with any third person except the authorised health and social care professional. I had provided the coordinated care to the patients by involving the patient into the treatment and health promotion process. As mentioned by Gaber (2019), coordinated care is the integrated care framework in which care givers work closely and synergistically with patients thereby involving patients in decision making of their own treatment process. In this regard, I maintained a clear and concise communication with patient regularly to maintain a systematic information-receiving system regarding patient’s health condition, feeling, current health issues and preferences. Under GDPR (2018), while conducting communication with patients for obtaining data, care givers must provide the detail and clear information to the patients regarding the reason of data collection and the process in which the data is going to be used (Gaber, 2019). Throughout the care deliver I adhered to all the principles of GDPR (2018), in which I took proper consent from the patient before starting an interaction to know that whether the patient is comfortable and agreed to the terms and condition as well as process of the treatment. During providing the coordinated care to the patients, I adhered to the principles of GDPR (2018) in terms of reviewing the entre procedures of the care delivery, interaction and assessment of the patients. As mentioned by Slotterback and Lauria (2019), while providing person centred care, reviewing of process regularly is important which enables caregivers to understand the usefulness and benefits of the care delivery for patients. In this regard, I checked regularly that whether the patient feel better breathing situation after using the bronchodilators and what is patient’s feeling during receiving the treatment. Personalised care is the important principle of PCC that I always maintained while taking care of the above-mentioned patients (Mccarthy and Muthuri, 2018). Under GDPR (2018), while conducting PCC, caregiver. In this regard, I emphasized on empowering patients by providing patient with proper health education regarding how to manage COPD and diabetes at homes by maintaining a systematic life and following proper medical regimen. Under GDPR (2018), I ensured that, I conducted an effective impacts assessment and analysis of personal data of patients which will enable me to understand the holistic needs of patients thereby enabling me to develop a proper care plan for the patient (Laverack 2019). I conducted a need assessment for determining the health and safety needs of the patient, such as determining which foods are recommended for patients, what medicine are prescribed for managing COPD and diabetes and how the lifestyle needs to be maintained for this patient to have a healthy life.
Scenario 1: Give a brief description of the patient or service user or individual in need that you have provided person-centred care to:
Scenario 1: Give a brief description of the patient or service user or individual in need that you have provided person-centred care to: I worked with a patient who suffered from dementia and anxiety. I was assigned at the night shift for this patients. This patient wad 65 years old and had short time memory loss. The patient was residing with her husband but no children. They had a caretaker who managed all the housing staffs for them such as cooking, cleaning, washing and food serving. The health assessment report showed that, the patient had been suffering from dementia since 4 years which impacted adversely on her decision making, problem solving and memorising skill. She had a poor cognitive skill. Due to osteoarthritis she was unable to move freely from one place to another thereby unable to perform her activities of daily living. Before admitted the hospital, she suffered from severe anxiety, depression and mood swing that made her so aggressive that she could harm anyone around her. Even she tried to hurt her husband while her husband did not fulfil her demand for letting her go out for a trip alone. During taking care of this patients I faced difficulties in implementing PCC, as this patient was highly uncooperative and aggressive. She most of the times refused to take the prescribed medicines. She could not share proper information regarding her health issues, feeling and premedical history. At night, most of the time she desperately tried to go to toilet alone , which could led to falls in bathroom. Therefore, it was difficult for me and other health staffs to provide a systematic and effective person centred care to her. How to provide person centred care by considering different key principles: While providing person centred care [PCC] to the patient in the second scenario, the first thing that I emphasised is treating the patient with proper respect and dignity by proving her a compassionate care (Laverack, 2019). Under GDPR (2018), while providing PCC to service users, caregivers must ensure that, they take proper consent from patient while obtaining data regarding the health of patients for providing coordinated care. In this scenario, as the patient was mentally ill and could not take the right decision regarding her consent, I took the consent from her husband on her behalf. Under GDPR (2018), if the service user is a minor or mentally ill who could not take the right decision, care giver can receive the consent from the legal guardian of the service users (Method, Laverack, 2019). Although the patients was high uncooperative, I tried my best to show polite and respectful gesture towards her which enabled me to gain her trust and build a strong relation with her. For providing coordinated care to the patient, I had used both the verbal and written communication with this patient. The verbal communication enabled me to make regular interaction with the patient by obtaining all the data regarding her feeling, her choice for treatment, her pain and health issues and her personal and professional life (Barnes, 2019). Under GDPR (2018) I adhered to the principles of confidentiality and informed consent in terms of ensuring that the patients is infirmed regarding the purpose of this data collection and all the collected data are handled by authorised person. The most important factors of person centred care is personalised care delivery to patients. In this context, I worked hard to empower this patient both mentally and physiologically to enable her to perform all the activities of daily living independently rather than being a passive recipient of care (Mccarthy and Muthuri, 2018). In this context, I motivated and encouraged the patient to be involved in her treatment and share her own thoughts and decision regarding her health promotion. I supported the patients by guiding her on how to maintain a healthy, independent and systematic lifestyle that share important for having a healthy body and mind. I also emphasized o developing a good self-management skill. For improving her condition, I referred the patient to a good psychiatrist for attending cognitive behavioural theory (CBT), which was proved to be high effective for improving the memory, decision making and behavioural changes in this patient (Wurm and Napier, 2017).
SWOT analysis:
By conducting this SWOT analysis, I can determine my strength and weaknesses.



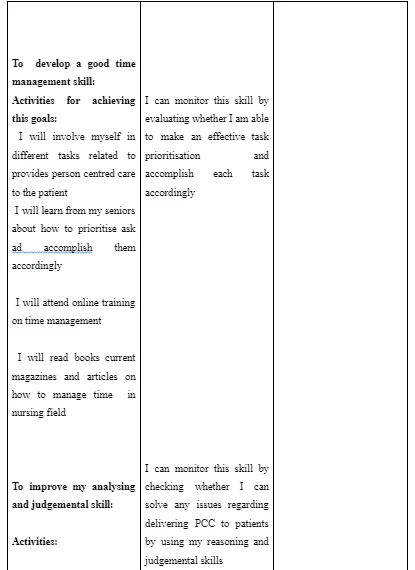
Personal development plan:






Reference list:
- Akpotor, M.E. and Johnson, E.A., 2018. Client empowerment: A concept analysis. International Journal of Caring Sciences, 11(2), p.743.
- Barnes, M., 2019. Contesting and transforming care: An introduction to a critical ethics of care. Theorizing Feminist Ethics of Care in Early Childhood Practice: Possibilities and Dangers. London: Bloomsbury Academic, pp.17-36.
- Big, S., 2016. Communication skills for patient engagement: argumentation competencies as means to prevent or limit reactance arousal, with an example from the Italian healthcare system. Frontiers in psychology, 7(2), pp.13-34
- Bölenius, K., Lämås, K., Sandman, P.O. and Edvardsson, D., 2017. Effects and meanings of a person-centred and health-promoting intervention in home care services-a study protocol of a non-randomised controlled trial. BMC geriatrics, 17(1), pp.1-9.
- Bristowe, K., Clift, P., James, R., Josh, J., Platt, M., Whetham, J., Nixon, E., Post, F.A., McQuillan, K., Ní Cheallaigh, C. and Murtagh, F.E.M., 2019. Towards person‐centred care for people living with HIV: what core outcomes matter, and how might we assess them? A cross‐national multi‐centre qualitative study with key stakeholders. HIV medicine, 20(8), pp.542-554.
- Burton, C.D., Entwistle, V.A., Elliott, A.M., Krucien, N., Porteous, T. and Ryan, M., 2017. The value of different aspects of person-centred care: a series of discrete choice experiments in people with long-term conditions. BMJ open, 7(4), p.e015689.
- Carayon, P., Wetterneck, T.B., Rivera-Rodriguez, A.J., Hundt, A.S., Hoonakker, P., Holden, R. and Gurses, A.P., 2014. Human factors systems approach to healthcare quality and patient safety. Applied Ergonomics, 45(1), pp.14-25.
- Couët, N., Desroches, S., Robitaille, H., Vaillancourt, H., Leblanc, A., Turcotte, S., Elwyn, G. and Légaré, F., 2015. Assessments of the extent to which health‐care providers involve patients in decision making: a systematic review of studies using the OPTION instrument. Health Expectations, 18(4), pp.542-561.
- Couët, N., Desroches, S., Robitaille, H., Vaillancourt, H., Leblanc, A., Turcotte, S., Elwyn, G. and Légaré, F., 2015. Assessments of the extent to which health‐care providers involve patients in decision making: a systematic review of studies using the OPTION instrument. Health Expectations, 18(4), pp.542-561.
- Dudeck, M.A., Edwards, J.R., Allen-Bridson, K., Gross, C., Malpiedi, P.J., Peterson, K.D., Pollock, D.A., Weiner, L.M. and Sievert, D.M., 2015. National Healthcare Safety Network report, data summary for 2013, device-associated module. American journal of infection control, 43(3), pp.206-221.
- Eton, D.T., Ridgeway, J.L., Linzer, M., Boehm, D.H., Rogers, E.A., Yost, K.J., Rutten, L.J.F. and Sauver, J.L., 2017. healthcare provider relational quality is associated with better self-management and less treatment burden in people with multiple chronic conditions. Patient preference and adherence, 11(2), pp.16-35.
- Eton, D.T., Ridgeway, J.L., Linzer, M., Boehm, D.H., Rogers, E.A., Yost, K.J., Rutten, L.J.F. and Sauver, J.L., 2017. healthcare provider relational quality is associated with better self-management and less treatment burden in people with multiple chronic conditions. Patient preference and adherence, 11(2), pp.16-35.
- Gondek, D., Edbrooke‐Childs, J., Velikonja, T., Chapman, L., Saunders, F., Hayes, D. and Wolpert, M., 2017. Facilitators and barriers to person‐centred care in child and young people mental health services: A systematic review. Clinical psychology & psychotherapy, 24(4), pp.870-886.
- Henry, S.G., Holmboe, E.S. and Frankel, R.M., 2013. Evidence-based competencies for improving communication skills in graduate medical education: a review with suggestions for implementation. Medical Teacher, 35(5), pp.39-40
- Hutton, B., Salanti, G., Caldwell, D.M., Chaimani, A., Schmid, C.H., Cameron, C., Ioannidis, J.P., Straus, S., Thorlund, K., Jansen, J.P. and Mulrow, C., 2015. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Annals of internal medicine, 162(11), pp.777-784.
- Hutton, B., Salanti, G., Caldwell, D.M., Chaimani, A., Schmid, C.H., Cameron, C., Ioannidis, J.P., Straus, S., Thorlund, K., Jansen, J.P. and Mulrow, C., 2015. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Annals of internal medicine, 162(11), pp.777-784.
- Keselman, A., Chase, R.A., Rewolinski, J., Dutton, Y.C. and Kelly, J.E., 2019. Lessons learned from multisite implementation and evaluation of Project SHARE, a teen health information literacy, empowerment, and leadership program. Journal of the Medical Library Association: JMLA, 107(1), p.72.
- Lindacher, V., Curbach, J., Warrelmann, B., Brandstetter, S. and Loss, J., 2018. Evaluation of empowerment in health promotion interventions: a systematic review. Evaluation & the health professions, 41(3), pp.351-392.
- Naldemirci, Ö., Lydahl, D., Britten, N., Elam, M., Moore, L. and Wolf, A., 2018. Tenacious assumptions of person-centred care? Exploring tensions and variations in practice. Health, 22(1), pp.54-71.
- O'hara, J.K., Armitage, G., Reynolds, C., Coulson, C., Thorp, L., Din, I., Watt, I. and Wright, J., 2016. How might health services capture patient-reported safety concerns in a hospital setting? An exploratory pilot study of three mechanisms. BMJ Qual Saf, pp.bmjqs-2015.
- Oppert, M.L., O'Keeffe, V.J. and Duong, D., 2018. Knowledge, facilitators and barriers to the practice of person-centred care in aged care workers: a qualitative study. Geriatric Nursing, 39(6), pp.683-688.
- Reedy, G.B., Lavelle, M., Simpson, T. and Anderson, J.E., 2017. Development of the Human Factors Skills for Healthcare Instrument: a valid and reliable tool for assessing interprofessional learning across healthcare practice settings. BMJ Simulation and Technology Enhanced Learning, 3(4), pp.135-141.
- Reedy, G.B., Lavelle, M., Simpson, T. and Anderson, J.E., 2017. Development of the Human Factors Skills for Healthcare Instrument: a valid and reliable tool for assessing interprofessional learning across healthcare practice settings. BMJ Simulation and Technology Enhanced Learning, 3(4), pp.135-141.
- Skene, K.R., 2021. What is the Unit of Empowerment? An Ecological Perspective. The British Journal of Social Work.
- Sweeney, J.C., Danaher, T.S. and McColl-Kennedy, J.R., 2015. Customer effort in value cocreation activities: improving quality of life and behavioral intentions of health care customers. Journal of Service Research, 18(3), pp.318-335.
- Tanekenov, A., Fitzpatrick, S. and Johnsen, S., 2018. Empowerment, capabilities and homelessness: The limitations of employment-focused social enterprises in addressing complex needs. Housing, Theory and Society, 35(1), pp.137-155.
- Zingg, W., Holmes, A., Dettenkofer, M., Goetting, T., Secci, F., Clack, L., Allegranzi, B., Magiorakos, A.P. and Pittet, D., 2015. Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. The Lancet Infectious Diseases, 15(2), pp.212-224.
- Zingg, W., Holmes, A., Dettenkofer, M., Goetting, T., Secci, F., Clack, L., Allegranzi, B., Magiorakos, A.P. and Pittet, D., 2015. Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. The Lancet Infectious Diseases, 15(2), pp.212-224.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



