A Holistic Approach for Elderly Patients
Introduction
Palliative care is associated with improving the quality of life of patients suffering from preventable or chronic illness. this care approach is widely used by modern health professionals in managing the different types of symptoms of patients thereby providing the psychological support to the patients and their family members. In the modern healthcare context, the deteriorating psychological and physical wellbeing of people suffering from lifetime illness impacts adversely on their living standard and quality of life. The deteriorating quality of life in patients suffering from long term illness becomes a matter of great concern in the modern nursing field. In this context, the palliative care approach is highly useful that applies holistic care framework that is not confined to manage not only the disease of patients, rather it is associated with building up a strong connection between body and mind of patients thereby improving their physical, emotional and spiritual wellbeing. For those seeking healthcare dissertation help, understanding these aspects of palliative care can be crucial. This report is going to discuss that how palliative care for the elderly patient, Aileen, in the case study will improve her quality of life thereby promoting her physical, psychological and emotional wellbeing.
Case study:
Aileen is an 85 years old Italian lady who lives alone at her home after the death of her husband four years ago. From the last three years, she suffers from Chronic obstructive pulmonary disease COPD and high BP. She also has the medical history of dementia, depression and anxiety. She loved to play golf, cook innovative dishes and play the guitar in her free tomes, which she stopped to do after her husband died. Due to her husband died; she suffers from a high level of depression and loneliness that enhances her vulnerability toward severe mental disorders such as dementia and motor neuron disease [MND].  She has a brother, Alex, who is involved in taking all the decision on behalf of Aileen. Aileen has poor decision-making skill, short times memory loss and lack of problem-solving skill that deteriorates her quality of living. In most of the times, she skips meals, medicines and inhalers, which lead to the development of many other symptoms such as breathlessness, anxiety, drowsiness and exhaustion. she spends all her day by staying at home which makes her overweight that deteriorates the quality of her life.
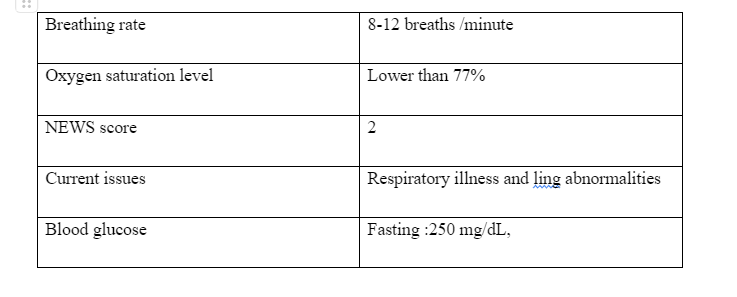
Aileen is diagnosed with chronic obstructive pulmonary disease (COPD) five eyers ago. Although she is prescribed by the doctors to use the inhalers (Tiomist 120 and Foracort 200), since her husband had passed away, she uses to skip the prescribed medicines as well as inhalers regularly that impacts adversely on her breathing condition. While examining her physical health it has been seen that Aileen is overweight with 85 kgs which poses adverse impact on her quality of life such as reducing her ability to do regular functions. As mentioned by Kunz and Minder (2020), overweight is the condition in which extra fats are accumulated into the body thereby increasing the BMI (body mass index). BMI is the measure that can be gathered through dividing a person's weight by the square of the height of that person. If the BMI of a person is within a range of 25-30 kg/m2, the person is considered overweight. Aileen has been suffered from the heavy cough, wheezing, shortness of breathing and chest tightness from last three days and has been admitted in the emergency ward with severe breathing issues. Through conducting the physical health assessment, Aileen has been diagnosed that long with COPD, Aileen has other chronic health condition such as lung infection and Type 2 diabetes as her blood glucose level is 250mg/dl which is far higher than the normal range. Flowing are the result of the physical health examination of Aileen:
She has a brother, Alex, who is involved in taking all the decision on behalf of Aileen. Aileen has poor decision-making skill, short times memory loss and lack of problem-solving skill that deteriorates her quality of living. In most of the times, she skips meals, medicines and inhalers, which lead to the development of many other symptoms such as breathlessness, anxiety, drowsiness and exhaustion. she spends all her day by staying at home which makes her overweight that deteriorates the quality of her life.
Aileen is diagnosed with chronic obstructive pulmonary disease (COPD) five eyers ago. Although she is prescribed by the doctors to use the inhalers (Tiomist 120 and Foracort 200), since her husband had passed away, she uses to skip the prescribed medicines as well as inhalers regularly that impacts adversely on her breathing condition. While examining her physical health it has been seen that Aileen is overweight with 85 kgs which poses adverse impact on her quality of life such as reducing her ability to do regular functions. As mentioned by Kunz and Minder (2020), overweight is the condition in which extra fats are accumulated into the body thereby increasing the BMI (body mass index). BMI is the measure that can be gathered through dividing a person's weight by the square of the height of that person. If the BMI of a person is within a range of 25-30 kg/m2, the person is considered overweight. Aileen has been suffered from the heavy cough, wheezing, shortness of breathing and chest tightness from last three days and has been admitted in the emergency ward with severe breathing issues. Through conducting the physical health assessment, Aileen has been diagnosed that long with COPD, Aileen has other chronic health condition such as lung infection and Type 2 diabetes as her blood glucose level is 250mg/dl which is far higher than the normal range. Flowing are the result of the physical health examination of Aileen:
Dig deeper into Undernourished Elderly Patients with our selection of articles.
This tool is widely used holistic assessment tools that assails health professional to assess the overall health condition in patients with complex critical health need. this tool designed under the national Gold Standard Framework Centre 2009. This tool assists health professionals in analysing the flowing holistic needs of patients:
Physical
Emotional
Personal
Social support
Information and communication
Control and autonomy
Out of hours
Living with illness
aftercare
The rationale for using the assessment tool:
PEPSI COLA is the effective health assessment tool that can be used by palliatives care providers to provide the person-centred holistic care to patients in terms of meeting all this critical need. in case of Aileen, PEPSI COLA tools can be used by the health professionals which will enable them to focus on different health domain such as potential anticipated health issues of Aileen, the health-related question asked to the patients and important resources needed to improve the outcomes the health assessment tool. PEPSI COLA tools are based on some healthcare principles that need to implemented and followed by the healthcare professionals while providing palliatives care to patients. in Aileen's case, palliative care providers need to prioritise individual health needs of patients. before using this assessment tool in case of Aileen, health professional needs to take proper consent from her guardian in family members. therefore, health professional needs to take consent from Alex regarding applying the PEPSI COLA tool in terms of assessing the health needs of Aileen. Under this assessment tool, health professionals will assess physical, emotional personal and social needs of Aileen which will enable the health professionals to develop such care plan that will be highly effective for promoting positive health and well-being in Aileen. As mentioned by Benyahia et al. (2017), PEPSI COLA tool is not only associated with assessing the physical, emotional and personal health needs of patients but also is associated with proving proper health education to patients in terms of enhancing their ability to lead their independently which improve their quality of living. Palliative care to elderly patients is highly effective when it is based on improving the quality of life of the patients by enhancing the ability to manage their basic needs and current health condition. In the above-mentioned case study, Aileen has more than one long-term illness such as COPD, type 2 diabetes and lung infection that not only minimises the quality of her life but also makes her emotionally and psychologically distressed. At her age (78 years), the development of more than one chronic health condition enhances her comorbidity. On the other hand, the breathlessness, increasing pains and inability to perform any regular activity deteriorates her mental, emotional and psychological wellbeing which enhance her vulnerability to serve mental disorders such as MND (motor neuron disease).
In case of the patient like Aileen who has a history of bereavement and loss and is highly vulnerable to morbidity due to deteriorating physical health condition, use of conventional treatment process is not effective, rather Aileen needs such care framework that will assist her to redeem her physical, emotional and psychological health condition thereby making her independent to perform her regular activities. In this context the selection of the assessment tool, PEPSI COLA, is expected to be relevant to the current health condition of Aileen, that will provide her with the proper psychological and emotional support that he needs to live a healthy; life. As mentioned by Benyahia et al. (2017), assessment through using the PEPSI COLA tool in palliative care to the elderly people is associated with multifaceted roles such as management and promotion of psychological and emotional wellbeing, educate patients regarding their self-management, medicines management, improve the decision making and cognitive skill of patients and promote the holistic development of patients. By using PEPSI COLA assessment tools, it is possible to improve the overall living standard and quality of life of Aileen, through improving her decision making, problem-solving skill, emotional and physical wellbeing and her reasoning ability. the PEPSI COLA tool that will not only focus on assessing the holistic needs of Aileen but educate her to make effective changes in her overall food pattern, lifestyle, culture, sleeping pattern, regular exercise, regular habits, thoughts and perception. Through using the assessment tools PEPSI COLA in palliative care in the case of Aileen, nurses can promote holistic development through conducting positive transformation of thoughts, decision and perception of Aileen. Through using assessment tool PEPSI COLA, it's possible for the health professionals to expose her into the external society in which he can make friends and interact with her neighbours to share her thoughts and decisions. In the context, the use of PEPSI COLA tool is highly appropriate in terms of not only providing the psychological and mental support to Aileen but also enhances her decision making, problem-solving and reasoning ability that will assist her to deal with any issue in life thereby improving her quality of living. On the contrary Bolt et al. (2020) argued that quality of life in palliatives care although is highly useful assessment tool in case of elderly people, in neds to be implemented with holistic care approach which provides elderly patients with the improved connection between their mind and body that is important to enhance inner strength of patients.
Factors associated with quality of life through using PESPSI COLA tool:
While it comes to improve the quality of in elderly people through providing palliative care, it is crucial for the palliative care providers to consider the factors that have a potential impact on the quality. These factors are, ethnicity, social class, age, social and family support, gender, spiritual values, culture, economic status of people. In the case study, while providing the palliative care to Aileen, palliative nurses need to determine her socio-economic status, social relationship, family relationship, her perception, values and culture, her beliefs and spiritual values that have a potential impact on her ability to be healthy and fit. As mentioned by Fausto et al. (2020), for improving the quality of life through providing palliative care to elderly patients it is important to improve the socio-economic condition, social position and spiritual values of the patients. In case of Aileen, as he suffers from high of depression, anxiety and restlessness, due to the past experiences of bereavement and loss, he needs proper sipper from her family members and society, which assists her to share her decisions and knowledge with the other people. In the context, palliative care providers need to emphasize on socialising Aileen by encouraging her to meet with neighbours and attending the social function that will assist her to normalise her life.
For better implementation of PEPSI COLA tool into practice to improve the quality of life of Aileen, palliative care providers need to use the important care framework, the holistic care framework. through using PEPSI COLA tool, the holistic needs of patients are determined and met. The palliatives care providers can use this assessment tool, to develop an effective holistic care plan for Aileen who will assist the care providers to dreaminess and met the complex holistic needs of Aileen such as the physical, emotional and spiritual needs. Holistic care framework through using PEPSI COLA tool, will not only focus on managing diseases of patients but also it is associated with promoting the physical, emotional, psychological and spiritual wellbeing of the person as a whole. Through promoting holistic care process, nurses can improve the connection between the body and mind of Aileen, which will assist her to develop positive thoughts, decision-making and positive spiritual thoughts. On the contrary Ebenau et al. (2017) argued that through holistic care although it is possible to treat the entire body and mind of a person, in case of considering the factors influencing the quality of life of people, holistic care sometimes can be irrelevant. In case of Aileen, as she suffers from the long-term illnesses such as lung infection, COPD and types 2 diabetes, it not only impact on her physical and psychological wellbeing but also in her economic, social, and cultural stats. In the context, the holistic care framework will emphasize on elevating the standard of living of Aileen by improving her economic, social, cultural and spiritual condition. Through psychotherapies and Cognitive Behavioural Therapy (CBT), palliative care providers can improve the behavioural, emotional and cognitive condition of Aileen which will improve her socio-cultural status. Through using the holistic care framework in the palliative care process, it is possible to improve the psychology, thoughts and decision-making ability of Aileen by exposing her to a different environment such as society, neighbourhoods and hospitals setting which will improve her overall behavioural pattern and interaction with the external world. On the other hand, through providing the financial guidance, holistic care providers can assist her to utilise her saving in a proper way which is useful in providing her psychological relaxation.
As mentioned by De Boer et al. (2017), holistic care process assists nurses and healthcare providers to educate the elderly patients that by improving their living standard. Through applying holistic care framework in the palliative care process, care providers can educate Aileen, in managing the impact of the above-mentioned factors by using her positive decision-making, positive thoughts and problem-solving skill. For example, throughout the CBT, Aileen will be trained about how he will react and interact with society people if any embarrassing situation comes. Through the holistic care approach, Aileen will be trained how to carry out self-management of own health, which will assist Aileen to realise her health condition, take necessary steps to improve the health condition such as immediately call the neighbours or local doctors. While improving the quality of life, palliative care providers will provide Aileen with knowledge about her rights and dignity.
Consultation and referral pathway in palliative care:
While providing palliative care to patients with lifetime illness, nurses sometimes need to follow the effective consultation as well as referral pathways in terms of optimising the care outcomes. In the case study, as oh has a critical health condition, here n palliative nurse need to conduct effective consultation with the other healthcare professionals in the multidisciplinary team. In the case of Aileen, the palliative care is provided by various care professionals such a general physician, nurses, pulmonologist, diabetologist, psychotherapists and carers and volunteers. As mentioned by Daya et al. (2017), through the proper referral process and consultation pathways, palliatives nurses can implement the person-centred approach in terms of meeting the complex health needs of patients. In the case study, as Aileen is highly vulnerable to morbidity due to existence of more than one long term health condition such as lung infection, type 2 diabetes and COPD, in which nurses needs to conduct the well-organised consultation process with pulmonologists, dieticians and psychotherapist in terms of developing a relevant care plan. Through consulting with the pulmonologist and diabetics, the palliative nurse can set the effective person-centred care approach for Aileen in which they will use the referred care process, foods, exercises, medicines and activities Aileen which is improved for improving her physical, psychological ad mental wellbeing.
The management plan for Aileen by using liaison model of palliative care:
As mentioned by Button et al (2019), palliative care is associated with effective management of disease and various symptom is patients. While providing palliative care to patients the most important things is to develop effective management through which care providers will follow the systematic process to determine the current health needs of patents and meet the needs accordingly. In the case of Aileen, the Liaison model of palliative care needs to be used in the case of Aileen in terms of carrying out proper management of physical, mental and emotional wellbeing. As mentioned by Brazil et al. (2017), the Liason model of palliative care is based on providing such a care-process in which there is the effective management of the health condition of patients by educating them in proper ways that will assist them to manage their health by themselves. In case Aileen, the palliative nurses and health professionals will develop such a care plan that will educate her about the importance of proper food selection and nutritional diet to have healthy mind and body, through providing healthy as well as nutritious foods, timely medicines, proper psychological, emotional and physical support, health education and self-confidence, care providers can make the positive transformation of the thoughts, decision making and perception of Aileen. In addition to this, by educating her about the self-health management care outcomes can be improved.
In the context, the Stress and Coping Theory can be used by the palliative nurse and health professionals in terms of reducing the stress and depression of Aileen. As mentioned by Gómez-Batiste et al. (2017), Liason model although is effective in developing knowledge of patients regarding their self-health management, the model does not focus so stress management and psychological development of patients. In the context, the nurse can use the concept of Stress and coping theory in the care plan of Aileen, which will assist them to reduces the depression, anxiety and stress level of Aileen thereby managing a positive health status of her.
Reflect on the commination barriers:
Good communication is considered as the foundation for developing effectives therapeutic relationship between the patients and health professionals (Brazil et al. 2017). as mentioned by effective communication will not only enhance the skill of health and nursing professionals to interact effectively with patients and their family members but also assists the health professionals to find out the barriers associated with person centred care. During my placement in a palliative care unit, I have emphasized on developing my effective communication skill. here I developed effects communication strategies in terms of managing the difficult communication with patients with life limiting illness. I focus on finding out the potential barriers that are associated with effectives communicating thereby assisting me to overcome the barriers through conducting the effective and clear interaction. While it comes to develop effective communication in palliatives care framework, the important thing is to develop an effective and strong patient-nurse communication system. I always believe that, the foundation of the palliatives care framework is dependent on how much the communication between the patients and nurses is compassionate and effective that assists nurse to determine holistic needs and issues of patients’ follow the different stages in terms of developing effectives communication with patients and their family members.
While imparting information to patients many factors influence the ability of the giver ad receivers to give and receive the information systematically. These factors are, the education level of both information giver and receiver, time constraints, stress level and developmental skill. in my workplace, before providing the information to patients regarding their health, I always check that whether the patients would be able to understand the information and if not than I develop effective strategies that will assist me to use simple words to simplify the information so that patients can understand them. on the other hand, in the second stage, information gathering need to be carried out in such a way that will assists both the information collector and information giver to perform the duties easily. Here I always use open ended questionnaire process, through which I use simple question to the patients whether the patients can answer the question through saying simply yes or no. the last stage, listening is the most important stage in which nurses need to listen to the response of the patients and interpret the nonverbal clues.
While carrying out the difficult communication nurses need to be prepared to make open as well as honest communication with patient. while communicating with patients with life limiting illness, I always ensure that I have the abilities and skill to make effective and transparent communication with them. while carrying out the different communication with palliative patients’ nurses need to determine the following aspects:
Diagnosis of patients
Deterioration of health
The advance care processes
Deciding when the enough is enough
I always shape my communication skill, before carrying out communication with palliatives patients in terms of determining the above-mentioned aspects. here I also use the following process while carrying out the effective communication in palliative care unt:
Ask-Tell ask process:
Tell: here I will tell new information to patients regarding their health that will enhance their knowledge about their health
Ask: here I will ask patients, whether they have understood what have been told to them
Nurse Mnemonic:

I will use this framework I erm sf dealing with emotion of patients while having difficult communication with them. Naming: here I will name the emotion of patients by observing their response, body movement and facial expression Understanding: during this communication process, I will try to understand what patients say, what are their queries and their pain. Respect: I will respect and value the motion of patients
Conclusion
From the above-mentioned discussion, it can be concluded that palliative care is associated with promoting the physical, emotional and psychological wellbeing of patients with lifetime illness thereby improving their quality of life. Palliative care providers need to consider many factors that can influence the quality of life of patients such as economic and social status, values, perception, beliefs and social support. Therefore, while providing palliative care to patients with long term illness, nurse and health professionals need to set highly effective management plan that will assist them to consider these factors to meet the current health needs of the patient
- Healthcare organisations need to conduct skill development training for palliative care nurses which will improve their knowledge and skill in developing the appropriate health management plan for the patient with long term illness
- Improve healthcare infrastructure of healthcare centres thereby using the modern medical equipment and modern technologies to improve the care outcomes in the palliative care process
- Improvement in the information delivery system in the multidisciplinary team s needed to transfer the right patient-related information to the other health professionals within an MDT at rights time, which will assist health professionals to track the overall health progress of patients.
Reference list:
Atreya, S., Kumar, R. and Salins, N., 2020. Community-based palliative care during the COVID 19 pandemic. Journal of family medicine and primary care, 9(7), p.3169.
Benyahia, S., N'Fissi, K., Sahut-D'Izarn, M. and Cudennec, T., 2017. Cancer and elderly people, what palliative care?. Revue de l'infirmiere, 66(233), pp.35-38.
Bolt, S.R., van der Steen, J.T., Mujezinović, I., Janssen, D.J., Schols, J.M., Zwakhalen, S.M., Khemai, C., Knapen, P.A.G.M., Dijkstra, L. and Meijers, J.M., 2020. Practical nursing recommendations for palliative care for people with dementia living in long-term care facilities during the COVID-19 pandemic: A rapid scoping review. International journal of nursing studies, p.103781.
Brazil, K., Galway, K., Carter, G. and van der Steen, J.T., 2017. Providing optimal palliative care for persons living with dementia: a comparison of physician perceptions in the Netherlands and the United Kingdom. Journal of palliative medicine, 20(5), pp.473-477.
Button, E., Bolton, M., Chan, R.J., Chambers, S., Butler, J. and Yates, P., 2019. A palliative care model and conceptual approach suited to clinical malignant haematology.
Daya, A.P., Sarkar, S. and Kar, S.S., 2017. Estimation of palliative care need in the urban community of Puducherry. Indian journal of palliative care, 23(1), p.81.
De Boer, D., Hofstede, J.M., De Veer, A.J., Raijmakers, N.J. and Francke, A.L., 2017. Relatives' perceived quality of palliative care: comparisons between care settings in which patients die. BMC Palliative care, 16(1), p.41.
Ebenau, A., van Gurp, J. and Hasselaar, J., 2017. Life values of elderly people suffering from incurable cancer: A literature review. Patient Education and Counseling, 100(10), pp.1778-1786.
Etkind, S.N., Bone, A.E., Gomes, B., Lovell, N., Evans, C.J., Higginson, I.J. and Murtagh, F.E.M., 2017. How many people will need palliative care in 2040? Past trends, future projections and implications for services. BMC medicine, 15(1), pp.1-10.
Fausto, J., Hirano, L., Lam, D., Mehta, A., Mills, B., Owens, D., Perry, E. and Curtis, J.R., 2020. Creating a palliative care Inpatient Response plan for COVID19–the UW medicine experience. Journal of Pain and Symptom Management
Gómez-Batiste, X., Murray, S.A., Thomas, K., Blay, C., Boyd, K., Moine, S., Gignon, M., Van den Eynden, B., Leysen, B., Wens, J. and Engels, Y., 2017. Comprehensive and integrated palliative care for people with advanced chronic conditions: an update from several European initiatives and recommendations for policy. Journal of Pain and Symptom Management, 53(3), pp.509-517.
Kunz, R. and Minder, M., 2020. COVID-19 pandemic: palliative care for elderly and frail patients at home and in residential and nursing homes. Swiss Medical Weekly, 150(1314).
Murray, S.A., Kendall, M., Mitchell, G., Moine, S., Amblàs-Novellas, J. and Boyd, K., 2017. Palliative care from diagnosis to death. Bmj, 356.
Paul, L.R., Salmon, C., Sinnarajah, A. and Spice, R., 2019. Web-based videoconferencing for rural palliative care consultation with elderly patients at home. Supportive Care in Cancer, 27(9), pp.3321-3330.
Sanvezzo, V.M.D.S., Montandon, D.S. and Esteves, L.S.F., 2018. Instruments for the functional assessment of elderly persons in palliative care: an integrative review. Revista Brasileira de Geriatria e Gerontologia, 21(5), pp.604-615.
Smets, T., Onwuteaka-Philipsen, B.B., Miranda, R., Pivodic, L., Tanghe, M., Van Hout, H., Pasman, R.H., Oosterveld-Vlug, M., Piers, R., Van Den Noortgate, N. and Wichmann, A.B., 2018. Integrating palliative care in long-term care facilities across Europe (PACE): protocol of a cluster randomized controlled trial of the 'PACE Steps to Success' intervention in seven countries. BMC palliative care, 17(1), p.47.
Sobański, P.Z., Brzezińska Rajszys, G. and Grodzicki, T., 2020. Palliative care for people living with cardiac disease. Kardiol Pol, 78(4), pp.364-373.
Stow, D., Spiers, G., Matthews, F.E. and Hanratty, B., 2019. What is the evidence that people with frailty have needs for palliative care at the end of life? A systematic review and narrative synthesis. Palliative medicine, 33(4), pp.399-414.
Continue your exploration of William's Complex Health Condition and Multidisciplinary Approach with our related content.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



