Rate of Depression in Thurrock
Introduction
Depression is the term used to describe feelings of low mood lasting more than two weeks that has an impact on daily activities of an individual (England and Mughal 2019). It is a common mental disorder and one of the factors leading to disability globally. Worldwide, approximately 264 million individuals are affected by depression (Wang et al 2014). There is a growing concern of how depression as one of the common mental health problem is. According to World Health Organization, mental health problems are the major causes of disability globally. Since time immemorial, there has been severe stigmatization of mental health problems. Due to this, many mental health disorders have gone without being recognized and untreated. Also, treatment of mental health has been done in separate silos form physical health and has been affected by lack of investment. The aim of this report is to analyse available information on depression in Thurrock to improve proper understanding of mental health problems in Thurrock which will help in building better systems in the United Kingdom as a whole. If you are seeking healthcare dissertation help, then you are going to have a thorough examination of topics related to depression and mental health. It is going to give you valuable insights into mental health challenges at a broader level within the UK.

Specifically, this report reviews the services and healthcare that are available for dealing with depression problem in Thurrock; demonstration of mental health statistics in Thurrock and UK, and compare it with global mental health statistics; and identification of the determinants, inequalities and barriers of mental health in Thurrock. To accomplish this, a virtual research tour of Thurrock is undertaken to identify the available social services (effective treatment like psychotherapy or cognitive behavior therapy) and key areas of mental health concern as far as depression is concerned. For instance, the inquiry is done to determine of Thurrock has services that can support people with urgent health needs, and whether the present adult mental health treatment system in Thurrock as a whole is fit to meet this purpose and requires significant system wide reforms.
About Thurrock County
Thurrock County has about 160,000 inhabitants. The unemployment rate stands at about 8.1%. The Economic Development Strategy of 2007 identified the economic challenges of Thurrock including areas like enterprise performance, growth of jobs, employment, and skills (Wake 2018). There is some concentration of socio-economic disadvantage in Thurrock County. Mental health is strongly related to income levels of residents as shown in the chat below.

Many specific communities within this area experience especially harsh levels of disadvantage on a par with large inner-city urban areas. For instance, Tilbury and Ockendon have identifiable communities where many forms of deprivation are apparent (Wake 2018). The main challenge here making sure that communities widely within Thurrock County can take advantage of new opportunities such as improved mental health screening (Carers UK 2015). Compared to its geographical neighbors, Thurrock County has the highest percentage of population with no skills and qualifications.
Studies indicate that depression in Thurrock is worsening among all age groups. One of the major factors that lead to this is that many people do not get the deserved treatment for mental illness (England and Mughal 2019). In addition, lack of access to care and stigma around mental health drive many individuals away from receiving the needed care. Currently, Thurrock experiences rising demand for mental health services compounded with commissioning organisations with vital saving challenges to deliver which contributes to several challenges of service delivery (N.H.S 2018). With this high level of need for mental health services, only a small percentage of individuals with mental health problems get any therapy while even a smaller percentage receive interventions to promote mental wellbeing or prevent mental health problems.
Health and social care data
The 2014 Survey of Mental Health and Wellbeing in England discovered that 1 in 6 individuals aged above 16 years experienced symptoms of mental health problems like depression. Women experienced depression more than men. Of these, 4.4% screened positive for post-traumatic stress disorder, 2% had experienced bipolar disorder while 0.7% had psychotic disorder in the last year. This prevalence has risen since 1993.

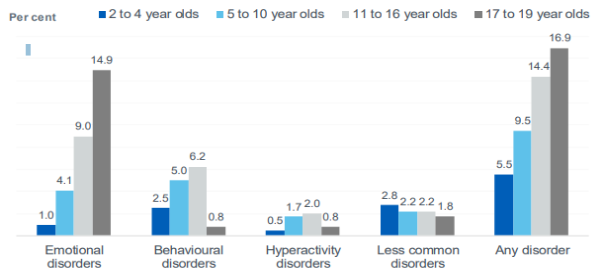
The 2017 survey gathered information about mental health from a sample of young people living in England. Data from the survey revealed a slight rise over time in the prevalence of mental health in 5 to 15 year olds rising from 9.7% in 1999 and 10.1% in 2004 to 11% in 2017.

The same survey indicated that young people aged 17 to 1 years were three times more likely to have a disorder (16.9%) than pre-school children aged 2 to years at 5.5%
Globally, more than 300 million people are approximated to suffer from depression, equating to 4.4% of the world’s total population. According to the Organisation for Economic Co-operation and Development (OECD), British people are amongst the most depressed people in the Western part of the continent. The UK percentage has doubled other countries such as Italy, Greece, Poland and Slovak Republic.in the American region, as many as 7.7% of the female population are depressed compared to males at 3.6%.
The main signs of depression include sadness, feeling of guilt or low self-worth, loss of interest or pleasure, tiredness, poor concentration, and disturbed sleep or appetite (Carers UK 2015). Researchers have noted the higher prevalence of depression in patients than in the general public. This is attributed to the illness itself as well as the unsatisfactory medical care service, heavy medical cost, and poor doctor-patient relationship. Depression is a notable comorbidity of chronic medical disorders. Researchers estimate the prevalence of depression in chronic medical conditions as: chronic obstructive pulmonary disease (24.6%), asthma (27%), gouty arthritis (20%), rheumatoid arthritis (15%), stroke (30%), systematic lupus erythematosus (22%), and atopic dermatitis (5%) (Wake 2018). Experts have shown that prevention programmes can reduce depression, both in adults and children. There are also effective therapies. Moderate or mild depression can be treated effectively with taking therapies like psychotherapy or cognitive behavior therapy. Even though antidepressants are not the first line of treating depression in adolescents, they can be an effective form of treatment foe moderate to severe depression.
In the United Kingdom, the disability caused by mental illness amounts to 22.8% of the total burden of morbidity compared to 16.2% for cardiovascular disease and 15.9% for cancer (N.H.S, 2018). Confirmed figures indicate that 1 in 6 individuals experiences mental health problems during their lifetime. Mental illness affects the health of population to a greater extent leading to health inequalities. A bi-directional relationship exists between poor physical health and poor mental health. Individuals with mental health issues are at the highest risk of experiencing notable physical health problems and are more likely to develop other conditions such as heart disease, diabetes, breast cancer, and bowel cancer. On the other hand, individuals with long-term physical health conditions are at higher risk pf mental health problems especially anxiety and depression.
At the national level, the number of people reporting their long terms mental health problems is rising. The rates in Thurrock are slightly lower than the national level figures but the rising trend seems to be affecting Thurrock also (Wake 2018). More positively, other data indicate that the number of adults reporting lower levels of happiness reduced in Thurrock from just over 13% to under 10% in 2011/12 and 2016/17 respectively (HM Government 2015).

The above data suggest that rate of mental illness may be rising partly because of mental health concerns and that rates of rising illness are not necessarily incompatible with improvements in quality of life.
The Projecting Adult Needs and Services Information estimated that the number of adults with CMHD in Thurrock will rise by 10 percent between 2015 and 2030.
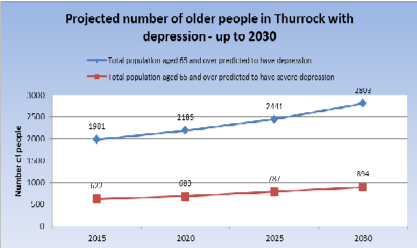
The rise is likely to be steeper in the older population. For instance, the number of adults above 65 years with depression is likely to rise from 1981 to 2803 between 2015 and 2030 (England and Mughal 2019). The graph indicates that there is a growing number of people affected with mental illness especially in vulnerable groups like adults which partly shows that there is growing recognition of mental illness.
Furthermore, people with mental illness are not able to manage their health properly and also do not interact well with services. They are more likely to misuse substances such as smoking which reduces their physical activity (HM Government 2015). Tied to this, such people are likely to miss medical appointments and cannot adhere to self-care regimens and treatment as required. Such people are likely to die at an earlier age compared to the general population. On the other hand, rate of mental illness especially depression is about two or three times more prevalent in people who have long-term conditions such as cancer, coronary heart disease, osteoporosis, arthritis, immunological problems, and multiple sclerosis compared to the general population (Wang et al 2014). These co-morbidities due to mental illness lead to higher treatment costs and poor physical health outcomes. It is approximated that one in every eight pounds spent on treatment of long-term conditions is related to co-morbid mental illnesses.
In general, treating mental ill-health in UK has been approximated to be around 105 billion pounds of which 30 billion is devoted to work related illness (N.H.S 2018). This is anticipated to rise and double over the next 30 years. The costs to Social Care for individuals with mental health amounts to 2 billion pounds yearly and is also likely to rise if there is no effective re-organisation and management. This is likely to add more pressure on an already overburdened Social Care and NHS systems. Care packages in Thurrock in this financial year rose to over 4.55 million pounds.
Health systems have not yet sufficiently responded to the burden of mental disorders. As a result, the gap between the need for treatment and its provision is wide globally. In middle-income areas, about 76% of people suffering from depression receive no treatment for their disorder. This is further compounded by the poor care quality for most of the people who do not get therapy. W.H.O’s Menthe mental Health Gap Action Programme launched by WHO proposes use of evidence-based technical guidance, training packages, and tools to expand services in settings with poor resources. The focus is to prioritize directing capacity building and set of conditions toward non-specialized health care providers. The Health Action Plan identifies the important role of mental health in attaining health for all individuals. One of the objectives of this strategy is the provision of integrated, comprehensive mental health and social care services in healthcare settings.
Determinants, inequalities and barriers to health
Determinants of mental health do not only include attributes like the ability to manage one’s emotions, thoughts, interactions, and behaviors with other people, but also, cultural, social, economic, environmental, and political factors like social protection, national policies, living standards, community support, and working conditions (N.H.S 2018). Other contributing factors include genetics, stress, nutrition, exposure to environmental hazards, and perinatal infections. Social determinant of health, according to World Health Organization, are the situations in which people are born, grow, live, work and age. These conditions are influenced by the distribution of power, money and resources operating at global, national and local levels (Carers UK 2015). The groups who experience inequalities due to social determinants include people with learning disabilities, black, Asian, and minority ethnic groups, people with physical health problems, refugees and asylum seekers, LGBT people, the homeless, substance abusers, and those experiencing domestic violence (Wang et al 2014).
The cause of poor mental health are complex but it is known that there are particular groups at high risk of mental health illness. Some of the key groups are those who live in deprivation, the unemployed, and those with long term conditions (N.H.S 2018). There is also evidence of intergenerational cycles in mental health. For instance, children whose parents have mental illness are, themselves, more likely to suffer from poor mental health. Furthermore, according to the Mental Health Taskforce (2016), 40 percent of individuals living in nursing or care services suffer depression compared to those living in their families.
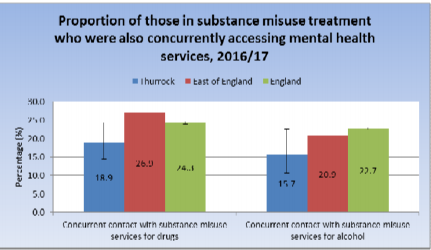
A high number of people suffering from mental illness in Thurrock County misuse drugs and alcohol.
In Thurrock County, there is a stronger correlation between obesity and poor mental health. The increasing rate of obesity in the area implies that the co-occurrence of obesity and mental illness will become more common (Wake 2018).

Exclusion is the main cause of depression in Thurrock County. The present emphasis on medical factors as a way of preventing depression is not enough. Social exclusion, including processes of material deprivation, exclusion from decision making, lack of participation in common activities in the society, is the way in which low income causes depression.
Review of current service provision
A wide range of settings are available for the treatment of mental illness. They include: hospitals, specialist mental health hospital, General Practice, community services, and IAPT (Improving Access to Psychological Therapies). 13.9% of registered depression patients entered IAPT services (Carers UK 2015). The mental healthcare system in Thurrock has traditionally been divided into tiers with each step of care showing the appropriate proportion of the prevalent population with common mental health disorders.

The recent numbers indicate that 742 newly diagnosed depression patients did not receive a timely review of their condition. The same survey shows that about 490 treatment interventions for patients with severe mental illness were not recorded.
Some of the patients were treated with prescribed medications. For instance, in 2016/17, 169,202 anti-depressant items were prescribed to Thurrock patients (N.H.S 2018). The total prescribing cost of mental health-related medications was 896564 pounds which was reduced by 637628 pounds over the last four years (England and Mughal 2019). Some of the patients received support from Adult Social care. 566 adult social care clients cited mental Health as their main support. In addition, 73.5% of adult social care clients felt they had control over their daily lives. Furthermore, only 50% of adult social care clients felts they had as much social contact as they would like (Wang et al 2014).
Currently in Thurrock, the Adult Mental Health Service provider landscape is fragmented and complex. It signals absence of continuity of care relationships, implying that care for an individual is dealt with by many different health and care professionals. This makes them to tell their stories several times (N.H.S 2018). The common mental health disorders that make up the vast majority of mental health issues among residents in Thurrock include anxiety, depression, obsessive compulsive disorder and depression (Carers UK 2015). These problems are majorly dealt with in primary care. The present therapy provided is limited to referral to social prescriber, prescription of anti-depressant medication, or psychological therapies. Patients who know EPUT can access phone lines everyday where they can seek advice (Wang et al 2014). A share care protocol is used for service users discharged form secondary to primary care. This is essential in case the patient deteriorates because it allows for a comprehensive handover of care and rapid access back into services (Wake 2018). Thurrock has a recovery college “Inclusion Thurrock” made up of courses which assist individuals to recover from mental health problems and self-manage their mental problems (Carers UK 2015). This involves programmes on understanding anxiety, mindfulness, and mood. In addition, Thurrock MIND, the largest of the sector organisations providing support to mentally ill people. Thurrock MIND offers various interventions such as supported housing, talking therapies, advocacy, positive pathways, and peer mentoring. They also participate in shared care protocol to aid people discharged from Essex Partnership University Foundation Trust (EPUT) services to live well and decrease secondary care re-admissions. At Grays Hill, the EPUT provides services for serious mental ill-health like bi-polar and schizophrenia disorder.
Different universal services are accessed by service users who are mentally ill. These include drug and alcohol treatment services, social prescribing, Healthy Lifestyle Services including NHS Health Checks operating in MIND and EPUT. Thurrock also has several specialists who provide care for given conditions which include individuals with personality disorders, eating disorders, and specialist perinatal mental health care. Mentally ill patients within Thurrock can access adult acute inpatient beds, assessment units, psychiatric intensive care beds, and older people functional beds.
Thurrock Mind and Inclusion Thurrock also offer a Recovery College to individuals living in Thurrock. The college offers helpful educational courses that assist people in learning what gives them the best opportunity of staying well (Wake 2018). The courses are open to all but especially benefit people who experience depression. They include understanding depression and anxiety, stating well, and caring for carers.
Role of the nurse in health promotion and screening
According to W.H.O, health promotion process enables individuals to increase control over and to improve their health. Facilitating this process requires that people be provided with relevant information (England and Mughal 2019). Nurses have a major role in providing this information in the form of mental health teaching. Nurses are accessible through many settings given their level of education and experience. Being an educator is one of the critical roles that nurses have in promotion of mental health (Smith and Bevan 2021). Nurses are consistently working to prevent illnesses like stroke, heart disease, obstructive pulmonary disease, and diabetes. They do this via different tactics including risk factor prevention, education, and monitoring of safety risks either in the community, workplace, or home.

A number of dimensions can be envisaged in comprehending the roles of nurses in primary care towards meeting the complexity of need arising from the individuals with mental health issues. The first dimension is screening for psychic and emotional distress; as the main problem or related to presentation of physical complaint (Smith and Bevan 2021). The second dimension is providing intervention support within boundaries of competence. Thirdly, nurses have the role to detect and manage physical and mental distress related to physical illness. In addition, they are tasked with engaging and supporting service user’s family members (Wang et al 2014). Finally, the nurses establish and maintain non-discriminatory practices towards people with mental health problems to identify and meet relevant professional needs across the team.
Conclusion and Recommendations for Practice
Mental illness is the single factor that leads to disability in the United Kingdom and the main cause of health inequalities. While there are several instances of good practice among health care providers, the present adult mental health treatment system in Thurrock as a whole is not fit to meet this purpose and requires significant system wide reforms. The latest Local Government Association Peer Review and Adult Mental Health Joint Strategic Needs Assessment came up with some strong assets to build on such as good service provision by Thurock MIND and Inclusion Thurrock to patients being treated, Thurrock First, Local Area Coordination, and Public Health Intelligence (Wake 2018). The five main priority areas addressed in the aforementioned pieces of work and which target areas of action for improvement of local mental health series include: improving access to timely treatment, addressing the issue of under-diagnosis of mental health problems, developing new models for common mental health disorders, developing new enhanced treatment and recovery model for people with serious mental ill-health conditions, and integrating commissioning and developing single common outcomes framework supported with improved commissioning intelligence.
Recommendations
The mental health problem issue requires a stronger lead at the national level. The “Five Year Forward View for Mental Health” promises a national mental health workforce strategy with the recommendation that the Department of Health should continue supporting the expansion of programmes that train people to qualify as social workers and contribute to make sure the workforce is prepared to offer high quality social work services in mental health.
There is need to make sure that everyone requiring support in Thurrock including carers and families get the right service at the right time from the right people in the right way. Thurrock should continue to remodel its services to make sure individuals get support at the earliest opportunity, promoting inclusion, supporting recovery, and empowerment.
According to Healthwatch Thurrock, the following recommendations will ensure that mental health issues are dealt with in the county: giving parents the support they need, improving children’s emotional health and well-being, reducing social isolation and loneliness, and improving the identification and treatment of depression in his risk groups (Thurrock Council 2016). Giving parents the support they require can be done by increasing awareness of support for children and parents who have disabilities and make it to access, and providing the disability support group. On the second theme, the emotional health and wellbeing of children can be improved by ensuring that activities like youth groups, clubs, and sports for teenagers are equitable across the Borough, considering subsidizing activities for young people, and urging schools and colleges to raise the profile of the support they offer. To reduce loneliness and social isolation, more publications of local community activities should be made available since many people are not aware of what is going on. Finally, identifying and treating depression in high risk groups can be improved by making sure that counselling services are able to recognize and understand the connections between LTCs and mental health. According to the Stroke Group in Thurrock, counsellors did not understand that having a LTC can be the main cause of depression.
References
- Benzeval, M., Judge, K. and Whitehead, M., 1995. Tackling inequalities in health: an agenda for action.
- Carers UK. 2015. State of Caring. Available at: https://www.carersuk.org/forprofessionals/policy/policy-library/state-of-caring-2015.
- Centre for Mental Health, DrugScope, UK Drug Policy Commission (2011). Dual diagnosis: a challenge for the reformed NHS and for Public Health England: A discussion paper. Available at: www.ukdpc.org.uk/wp-content/uploads/dual-diagnosis-achallenge-for-the-reformed-nhs-and-forpublic-health-englan.pdf.
- Department of Health (2020). Improving the Health and Well-being of People with Long-term Conditions. World class services for people with long-term conditions: Information tool for commissioners. London: Department of Health.
- England, E. and Mughal, F., 2019. Underprovision of mental health services for children and young people.
- England, N.H.S., Improvement, N.H.S. and National Collaborating Centre for Mental Health, 2018. The perinatal mental health care pathways. London: NHS England.
- HM Government. (2015) Healthy lives, Healthy people strategy for Public Health England; Delivering better health for all people. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216096/dh_12742 4.pdf.
- HSCIC 2014. Statistics on Drug Misuse: England 2014. Available at: http://digital.nhs.uk/ catalogue/PUB15943/drug-misu-eng-2014-rep.pdf
- NICE, England 2020. https://www.nice.org.uk/guidance/cg90/chapter/Context#care-of-all-people-with-depression
- Smith, S. and Bevan, A., 2021. Role of school nurses in identifying and supporting children and young people with mental health issues. Nursing children and young people, 33(1).
- Strategy, W., Health and Wellbeing Strategy.
- Thurrock Council 2016. Thurrock Joint Health and Wellbeing Strategy. Available at: https://www.thurrock.gov.uk/sites/default/files/assets/documents/hwb-strategy-2016-v01.pdf.
- Thurrock Council. 2016. Annual Public Health Report: A Sustainable Adult Health and Social Care System for Thurrock- Executive Summary. Available at: - https://www.thurrock.gov.uk/sites/default/files/assets/documents/annual_health_report_2016_su mmary.pdf
- Wake, I., 2018. Mental Health Service Transformation in Thurrock–The Next Steps.
- Wang, J., Wu, X., Lai, W., Long, E., Zhang, X., Li, W., Zhu, Y., Chen, C., Zhong, X., Liu, Z. and Wang, D., 2017. Prevalence of depression and depressive symptoms among outpatients: a systematic review and meta-analysis. BMJ open, 7(8), p.e017173.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



