Enhancing Stroke Patient Admissions and Metrics in UHL Stroke Services
Abstract
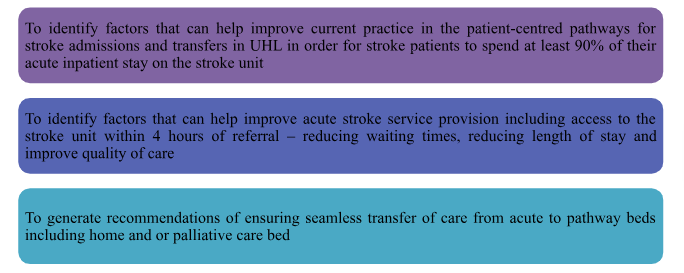
Focus of Service Improvement Project
The focus of this Audit is to determine the reasons behind a delay in the rapid admission and transfer of stroke patients to specialised stroke beds
Methods
Data will be derived from Sentinel Stroke National Audit Programme (SSNAP), this will be accessed via the audit team. There will be no patient identifiable information as the data will already be anonymised. The proposed sample population will comprise of 100% patients admitted to UHL presenting with acute stroke from October 2020 and June 2021, this covers three quarters of the SSNAP audit data available. Collecting three quarterly information will help in comparison between winter into summer.
Study population: Sampling
Approach: Quantitative and descriptive research
Method: Clinical Audit using secondary data from SSNAP
Data analysis: Analysis
Findings: The analysis of the audit mentions that more than half of the patient admitted in the hospital have suffered acute stroke with increased expression of adverse symptoms compared to all patients who have suffered stroke. The audit further indicates that nearly all patients who suffered stroke in Leicester spend most of their time in the stroke unit, but they are not transferred to the stroke unit within the stipulated time mentioned in the standards of care. Moreover, lesser number of patients are reviewed by stroke consultant compared to stroke nurse informing few stroke patients received specialised analysis from the physician. The audit indicates that lesser number of stroke patients received effective multi-disciplinary care and in majority of them the rehabilitation goals were fulfilled. The audit also informs that most of the standards of care for discharge are met in nearly all the admitted stroke patients ensuring their safe discharge.
Introduction
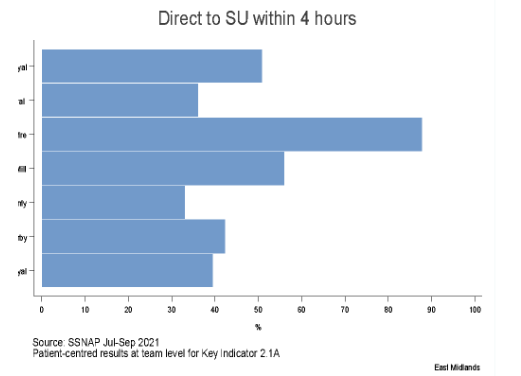
The project has been designed to address the persistent issue of high proportions of stroke patients being admitting to medical wards instead of the hyper-acute stroke ward. This has implications including but not limited to mortality and morbidity following an acute stroke and impact on local stroke metrics. The core issue is the admission of non-stroke medical patients/ outliers to acute stroke beds. Stroke units in the country are driven by targets, our metrics in the recent SSNAP data indicate that improvements in services we offer which include rapid access to the stroke unit, access to stroke specialist assessments are crucial (SSNAP,2021). Currently the UHL stroke services in the last quarter SSNAP results published June 2021 scored a D in the proportion of stroke patients admitted to the stroke unit within the first four and a half hours of admission, also for stroke patients that have spent at least 90 % of their inpatient stay on the stroke unit. For those seeking assistance in this realm, accessing reliable sources like healthcare dissertation help will provide you the invaluable support in navigating these complex challenges and bringing meaningful change within healthcare systems.

Sentinel Stroke National Audit Programme (SSNAP) is a crucial national healthcare quality improvement programme that measures performance management, quality improvement, and financial reimbursement for one hundred and eighty-nine stroke Units across England, Wales and Northern Ireland (Bhala et al, 2020). The role of SSNAP is to monitor and evaluate the organisation and quality of stroke care in the NHS (Royal College of Physician, 2016). According to the RCP (2016) SSNAP is currently the only source of stroke organisational and clinical audit data in England, Wales, and Northern Ireland. SSNAP data is used to inform patients, the public commissioners and clinicians on the standards of stroke care provision for the purposes of care quality improvement (Bhala et al, 2020). The data is benchmarked against the National average, relevant data audited is inclusive but not exhaustive of nurse to bed ratio, number of stroke beds available to stroke patients, stroke acute treatments, access to the stroke unit within the first 4 hours of admission, access to specialised stroke nurses, doctors and allied health professionals using Evidence-based standards (National clinical guideline for stroke, 2016).
Rationale
In the UK, stroke is one of the leading health issues which affects most of people who are adults and elderly. Stroke is regarded as one of the key reasons for untimely development of disability and death in individuals (Kuriakose and Xiao, 2020). It is evident as in the UK, more than 113,000 individuals suffer from stroke each year in the UK and at the present there are 1.3 million stroke survivors. In the UK, stroke occurs every five minutes leading many individuals to be admitted due to stroke in the hospital in a day (King et al., 2020). In hospital admission of the stroke patients, the individuals are required to be admitted directly to the stroke unit for receiving specialised care so that their risk of disability and death can be reduced (Patel et al., 2020). However, between July 2021 and September 2021, 12.5% less patients who suffered stroke were found to be directly admitted to the stroke unit within four hours of admission at the hospital (strokeaudit.org, 2022). This indicates that more stroke patients in the UK in the latest condition were found unable to receive specialised care within the stipulated time of four hours after stroke on being admitted to the hospital. Thus, it is considered to be a key issue raised within the care environment for stroke patients.
The immediate admission of stroke patients to stroke unit within four hours is a key issue because lack of fulfilment of the condition creates increased risk for the stroke patient for life and disability. It is required as best care is needed to avoid the negative consequences if health to be caused by stroke could not be prevented (Fekadu et al., 2019). Moreover, the condition leads to delayed specific health assessment of stroke patients by specialist physicians (Fekadu et al., 2019). It is evident as the data between July 2021 and September 2021 informed that lack of timely transfer of stroke patients in the stroke unit in the hospital has led to increased 1hr and 38min additional time to be added to median time of consultation which is 10hr 04 min (strokeaudit.org, 2022). This indicates that discussion regarding the detailed prevalence and further effect of rapid admission of stroke patients in the specialised stroke unit for stroke patients is to be reviewed to under if it does have an actual impact on improving or deteriorating the health of the stroke patients.
Aim and purpose of the SIP set within clinical background
Literature Search Strategy
Search Strategy
The literature review is referred to the way of investigating and examining the existing evidence related to a current topic for allowing the researchers to identify the known and the unknown facts regarding the research topic (Shalaby and Agyapong, 2020). The literature review is to be used in gathering existing information for the study because it informs increased clarity regarding the background and current scenario of the topic which would help the researcher in broadening their knowledge for the analysis of the study topic to reach contextualised findings. This in turn would help the researcher to develop better idea about the way auditing is to be performed so that true information regarding the raised problem can be identified. The execution of effective literature review assists in gathering consolidated ideas regarding any study and determining the gaps in them to be fulfilled (Wang et al., 2019).
The literature review would be performed through electronic search strategy. This is because the gathering of information electronic searching helps in saving the increased amount of time as the use of specific keywords helps in identifying the variety of related information in any study platform (Ohlwein et al., 2019). The other reason of using electronic search strategy is that it is cost-effective as most of the data are freely available with few information being charged with nominal amount to be used. In addition, electronic searching helps in avoiding geographical barriers which leads to create obstacles towards gathering potential data regarding a topic from worldwide or specific country or locality due to hindered reach to the area. However, electronic searching avoids any obstacles by helping key access to various relevant data all over the world through specific platforms. The keywords to be used in executing the search are “stroke patients”, “cardiac patients”, “specialised stroke units”, “admission of cardiac patients”, “ischemic stroke” and others. The Boolean operator AND and OR are to be used in linking the search terms to frame a meaningful search of the selected electronic platform.
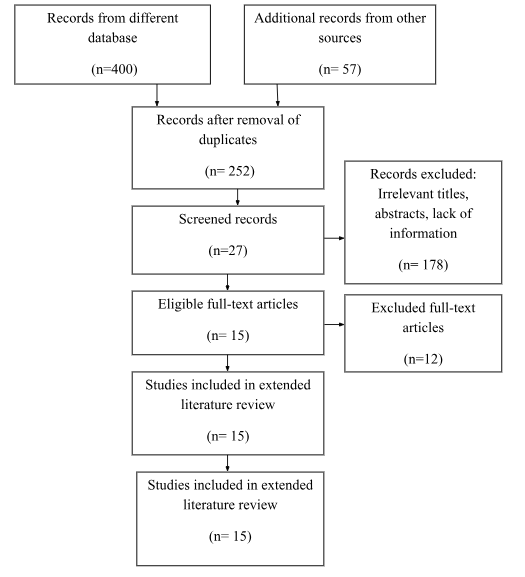
The platforms used for performing electronic search are CINAHL, MEDLINE (PubMed) and British National Index (BNI) and Cochrane Library. The CINHAL is a potential database to be used in gathering potential healthcare information because it allows access to wide number of nursing journals based on various topics (ebsco, 2021). The MEDLINE database is to be used because it contains various authoritative, complete and peer-reviewed journals and articles which permits to determine the way the research is effectively conducted, way and who wrote the results and place where the research is being executed for gathering the results (medline.com, 2021). The BNI database is also to be used because it contains data regarding any topic that support enhanced education, practice and development and research of health visitors, nurses and healthcare staff (bniresearchgroup.com, 2021). The Cochrane Library is also used in framing the literature review as it reflects the findings of new information helping valuable evidence to reach the researcher for enriched understanding regarding any topic. It is also a good database because it contains information that are of golden standards due to which information used from the database leads to reduced error in data presentation (cochrane.org, 2021).
In selecting the articles for developing the literature review, the inclusion and exclusion criteria are to be followed. The inclusion criteria set the characteristics to be present in the study for its exclusion whereas exclusion criteria set the characteristics which are to be avoided from the study for its enriched and error-free execution. The specification of the criteria is important as it informs the reader regarding the aspects chosen by the researcher to be included and avoided in the study. The inclusion criteria for the review are articles published on and after 2017, containing information regarding admission to stroke unit of stroke patients, written in English, containing qualitative and quantitative data and academic in nature. The articles to be excluded are written in languages other than English, published before 2017, non-academic, contains information regarding cardiac disease patients and contains systematic data. The articles published on and after 2017 are included because they contain current updated information regarding the study topic with better overview presented through advanced scientific experimentation. The articles published before 2017 would be excluded as it contains backdated information that may be modified through current scientific analysis leading the data previously identified to be with error.
The articles which are written in English would be included as the researchers belong from UK where the key language spoken and understood is English. Therefore, for effective data presentation from the existing articles with understanding of their meaning, the choice of language is to be maintained. The articles written in language other than English would be excluded as they contain information that are unable to be understood for presentation by the researchers. The articles which are academic in nature would be included as they have data presented in a logical and analytical manner which helps the researcher is better interpretation of facts to be presented in the study. The articles which are non-academic such as newspaper, magazines and others would be excluded because they contain descriptive data that are not well-supported through facts to understand their true nature for presentation in the study. The articles containing qualitative and quantitative data would be included as it would help in a descriptive and objective understanding of the topic.
Types of Evidence for Consideration
In research, there are different types of evidence that are considered, and they are levelled accordingly. According to Ackley et al. (2008), the type of evidence which is levelled at 1 is systematic review or meta-analysis of randomised control trial or evidence-based clinical practice. The type of evidence considered at level II is evidence which are gathered from well-designed randomised control trial study. The quasi-experimental is another type of evidence which is regarded as level III by Auckley et al. (2008). The other type of evidence considered in research is case-control studies, cohort studies, descriptive or quantitative studies and evidence of opinion regarding topics by authorities.
Data Extraction Process
Data extraction is referred to the process through which researchers gathers necessary information regarding study characteristics and findings from the studies included in the review. The requirements for data extraction vary from one review to another as they are needed to be tailored to the review question set in the study. The initial step of data extraction process is planning the nature of analysis and listing the tables to be included in the report. It will assist in identifying the data to be extracted in the study (Wang et al., 2018). The data extraction required to be reliable and unbiased as possible, but it is prone to human error and are found to be often subjected for requirement of decision towards its inclusion in the study. The number of researchers who are involved with the study to perform data extraction are likely to be subjected to time and resource constraints. Thus, it is ideal that two researchers perform the data extraction process in independent manner. The accepted minimum is that one of the researchers extracts data with the other researcher independently examining the data extraction for judging its completeness and accuracy. The method may result in creating more error in performing data extraction but may provide better data collection in limited amount of time (Büchter et al., 2020).
The disagreements of the data are to be noted and resolved by forming consensus by the researchers or through arbitration by any independent researcher. The record of amendments or corrections related to data extraction are to be kept in record for future references mainly for condition when internal inconsistency in results are unable to be resolved during discussion (Büchter et al., 2020). The studies to be included for extraction are to be screened based on the inclusion and exclusion criteria so that the best journals and articles are chosen for executing the study (Wang et al., 2018). The reviews to be included in the study from which data are to be extracted through descriptive analysis may led to overestimation of results for which data from other studies are to be included to minimise the bias in the study. The methodological evaluation of the selected studies is to be made to determine its accuracy to be used in data extraction for the current study (Wang et al., 2018).
PRISMA/Search Tables
Literature Review
Overview of Stroke
A stroke is referred to a medical condition in which poor flow of blood occurs to the brain cells leading them to be damaged resulting in hindered functioning of the brain tissues in supporting the health of the individuals (Mach et al., 2018). There are mainly two types of stroke which are ischemic stroke and haemorrhagic stroke. In ischemic stroke, blood clot is formed which causes blockage or narrowing of the artery supplying blood to the brain. The blood clot is formed in the artery due to build-up of plaques in the them. In this nature of stroke, the blood supply to the brain is decreased and not entirely blocked causing dysfunction of the tissues in the brain area (Campbell et al., 2019). The symptoms of ischemic stroke are sudden numbness or weakness of the arms, legs or face, sudden trouble in speaking, sudden confusion, and others (Campbell et al., 2019). The ischemic stroke may also occur due to obstruction caused by embolus in other parts of the body apart from blood vessels as well as may be caused by systematic hypoperfusion that is generally reduction in blood supply as a result of sudden experience of shock (Campbell et al., 2019).
In contrast, Haemorrhagic stroke occurs as a result of the bursting out of the blood vessels leading to cause bleeding in the brain. The build-up of pressure on the brain cells due to oozing out of blood causes damage to them leading the patients to develop hindered neurological health. The haemorrhagic stroke is of two types which include intracerebral haemorrhage in which the bleeding mainly occurs in the brain that floods the surroundings brain tissues due to intraparenchymal or intraventricular haemorrhage. The other type is subarachnoid haemorrhage in which the bleeding happens outside of the brain in between the pia matter and arachnoid matter (Mach et al., 2018). The symptoms of haemorrhagic stroke include sudden and severe headache in the back of the head, losing consciousness, confusion and irritability, inability to love, muscle pain in the neck and shoulders and nausea and vomiting (Mach et al., 2018).
Global incidence and prevalence of Stroke
In the global context, Stroke is considered to be a health issue that has reached epidemic proportions of prevalence indicating it is widely present among people of various nations. The reports in 2021 inform that nearly 13.7 million new cases of stroke are reported every year around the world with 1 in 4 of them being aged 25 years. It is also reported that 60% of all the nature of stroke occurs among individuals who are below 70 years of age with 8% of them being under 44 years of age (WSO, 2019). This indicates that development of stroke is mostly found in adult population before they reach the elderly stage. The reports disclose that 52% of individuals affected over the world by stroke are men and 48% of them are female (WSO, 2019). This informs that men are more prone to develop stroke compared to women. The global data regarding all form of stroke further inform that 80 million people are currently living in different countries who have experienced stroke. Among the people, 60% of them who have suffered stroke and still living are below the age of 70years and 10% of them are below the age of 44%. In respect to gender, 49% of individuals who have suffered stroke and currently living over the world are men whereas 51% of them are female (WSO, 2019). This indicates that globally female act as half of the person who has suffered stroke similar to men informing there is not much gender differences present in respect to the experience of stroke among people.
The mortality incidence in regard to stroke informs that five and half million of people annually die due to stroke. Among the deaths reported, 39% of them occurs in people who have suffered stroke under 70 years and 4% of the deaths have occurred to people who are under 44 years of age. in respect to gender, 53% of all stroke-related death has occurred in men whereas 47% of the deaths have occurred in women (WSO, 2019). This informs that men are more vulnerable to experience death out of stroke compared to women and people who are above the age of 44 years. In regard to disability-adjusted life years, 116 million years of healthy life is mentioned to be lost due to death and disability caused among people out of stroke. It is further identified that 63% of the healthy life as a result of stroke-related health issue and disability is caused in people who are lower than 70 years of age with 18% of the health life lost out of stroke-related complications is among people who are under 44 years of age (WSO, 2019). This indicates that the increased disability and death is faced by people who are older than the younger adults as a result of stroke. In respect to gender, it is identified that 56% of the healthy life as a result of stroke-related health issue is lost among men whereas 44% of the health life due to disability years out of stroke occurs among women (WSO, 2019). This informs that men are prone to experience more disability year and hindered health consequences as a result of stroke compared to women.
The global reports mention that ischemic stroke is the commonest form of stroke compared to haemorrhagic stroke. It is evident as of 2016, nearly 9.5 million new cases of ischemic stroke are reported worldwide whereas only 4.1 million new cases of haemorrhagic stroke are reported in the time (WSO, 2019). This indicates that the incidence of ischemic stroke in people is double the haemorrhagic stroke making it the commonest nature of stroke to be faced by people. However, compared to ischemic stroke, the people who suffer a haemorrhagic stroke are found to lose more health years of life and facing increased year of death and disability. It is evident as per reports where it is mentioned that 51.9 million healthy years are lost each year due ischemic stroke-related disability and death compared to the loss of 64.6 million healthy life each year due to haemorrhagic stroke-related disability and death in people (WSO, 2019).
Factors influencing occurrence of Stroke
The occurrence of stroke in patients are caused by various factors such as socio-economic status, genetic construct, lifestyle management and others. In the study by Rutten-Jacobs et al. (2018), the key aim was to evaluate the association of lifestyle and polygenetic risk score with incidence of stroke in patients. For this purpose, the researchers performed a prospective population-based cohort study with collection of information about 306,473 women and men who are aged 40-73 years from the UK biobank. The results presented in the study mentions that after medial follow-up for 7.1 years, 2077 incidence of strokes are ascertained. The incidence of stroke was found to be 35% more among people who are placed at the higher genetic risk or placed in top third of the polygenic score compared to the people who have low polygenetic score (Rutten-Jacobs et al., 2018). This indicates that genetic scores and constructs in people are a responsible risk factor towards making individuals experience stroke. The results further revealed that people who followed unfavourable lifestyle actions such as unhealthy food intake, smoking, alcohol intake and others are 66% increased risk of developing stroke compared to the people who follow favourable lifestyle (Rutten-Jacobs et al., 2018). This informs that way of leading life has a key contribution towards making individual be at risk of stroke.
The study by Price et al. (2018) aimed to explore the behavioural and related risk factors that influence the incidence of haemorrhage and ischemic stroke in people. For this purpose, total of 712,433 women study participants are included in the study prior to the occurrence of heart disease, stroke or cancer with reported behavioural and related factors at the initiation of the study or baseline. They were follow-up for gathering results and cox regression analysis was performed to relate factors with type of stroke. The results revealed that on follow-up after 12.9 years, 8,128 women mentioned suffering incidence of ischemic stroke, 1,536 women expressed incidence of subarachnoid haemorrhage and 2,032 women reported intracerebral haemorrhage. The women who had diabetes mellitus were seen to show increased risk of ischemic stroke but reduced risk of subarachnoid haemorrhage. The stroke risk was found to be more among women who mentioned their health to be fair or poor compared to the women who rated their health to be good and excellent. Among the 565,580 women who mentioned their health to be good or excellent, smokers were mentioned to be at increased risk of development of stroke. The results also revealed that obesity is associated with increased risk of stroke in women.
The study by Markidan et al. (2018) mentions that tobacco smoke contains nearly 7000 and more chemicals which include arsenic, carbon monoxide, cyanide, formaldehyde and others. The chemicals on getting transferred to the lungs enter the blood stream which moves to different parts of the body causing damage to the healthy cells. The changes in cellular structured created by the chemicals of the cigarette leads the individuals to be at risk of facing stroke. As argued by Chen and Xu (2020), the cigarette smoke leads to raise the cholesterol levels in the body. The cholesterol is a key substance in the body whose presence in increased amount causes deposition of fatty substances in the arteries leading to development of heart diseases and stroke in patients. Thus, smoking is seen to lower the good cholesterol level in the body and enhanced bad cholesterol that has high chances of deposition in the arteries to make them narrowed leading to hindered blood flow.
In contrast, the study by Pan et al., (2019) mentions that inhalation of cigarette smoke which contains nicotine and carbon monoxide on entering the blood reduces the amount of oxygenation of the blood. Moreover, nicotine causes the heart to beat faster and raises the overall blood pressure. The increased blood pressure creates tension in the arteries leading the individual who smoke to be at increased risk of developing stroke. The smoking also may lead to episode of atrial fibrillation which is a condition that raises the risk for stroke in individuals (Chen et al., 2019). In addition, the chemicals present in the cigarette smoke leads to development of sticky platelets which increased formation of blood clot creating risk for stroke in people (Chen et al., 2019). In the study by Oesch et al. (2017), it is mentioned that obesity or high BMI rate of the individuals creates risk for them to develop stroke. This is because obesity leads to increased deposition of fats in the body compared to people with normal weight condition. The increased fat deposition leads the body to require increased nutrients and oxygen. The blood vessels in the body cause circulation of more blood to the extra fat tissues making the heart to work harder in pumping blood around the body. The increased need of blood circulation and increased pressure on the walls of the arteries creates risk for stroke.
The study by Wang et al., (2021) mentions that alcohol does acts as a potential risk factor development of stroke incidence in people. This is because excessive alcohol consumption causes atrial fibrillation which is irregular and rapid beating of the heart that can form blood clots. The atrial fibrillation increases the risk of stroke in people by five times as it supports the formation of blood clots which is the key element for incidence of the disease. In the study by Xia et al. (2019), the key aim is to determine the risk factors for stroke in patients. For this purpose, data from the National Stroke Screening survey is taken. The findings inform that hypertension is most prevalent factor among patients who suffered stroke. This ensured that people with high blood pressure are at increased risk of develop stroke. The findings further mention that rural stroke survivors expressed increased rate of alcohol consumption and smoking indicating them to be risk factors for the condition. The presence of obesity, diabetes, atrial fibrillation and others influences the risk of stroke incidence in people.
Hospital admission of Stroke patients
The admission of stroke patients is found to be done inappropriately which often leads to challenging health consequences for the patients out of the delayed and improper care. In the study by Alegiani et al. (2019), the researchers aimed to explore the reason for delayed admission of the patients after stroke. In this purpose, 15 patients are interviewed who presented more than 4.5 hours presence of symptom onset for stroke. The interviews are recorded and analysed through standardised descriptive analysis. The findings inform that most of the patients reported they predominantly noticed the symptoms of stroke on their own due to which they could not decide the steps to be taken to get admission out of confusion regarding the symptoms being exclusively of stroke. The presence of fear, shame and uncertainty regarding stroke symptoms also led the patients to get delayed admission and care. The lack of adequate information regarding stroke is found to create added hindrance towards timely admission of the patients who suffered stroke. Moreover, increased waiting time was regarded as a contributing factor towards delayed admission of stroke patients in hospital.
The study by Al Khathaami et al., (2018) also aimed to determine the factors related with late admission of stroke patients in the emergency department. The study is a cross-sectional survey which is performed for a period of 6 months. The structured questionnaire is used for questioning the stroke patients and their relatives for exploring the factors leading to delay in their care. The study findings mention that nearly 56.4% of the 227 patients received care after 4.5 hours onset of the stroke symptoms. The reason for delayed care delivery includes being alone during the onset of stroke, delayed during transportation in the hospital out of lack of ambulance, not knowing the patients are experiencing stroke and residing outside the city limits. Thus, it can be seen that delayed admission is mainly influenced by hindered transportation of the patients to the hospital as well as lack of adequate education in detecting the symptoms of stroke to apply for immediate admission to the hospital. The study Machin and Hamdan (2018) also aimed to explore the factors related with the onset of hospital delay in people who suffered stroke. For this purpose, 107 subjects were included in the study who were interviewed. The findings informed that distance between the hospital and the patient’s home acted as a potential reason behind the delay in hospital admission in stroke patients. Moreover, the delay in referral of the patients and the lack of awareness about stroke symptoms in the patient led to delay in hospital admission for stroke.
Gaps in Literature
The existing literature provide overview regarding stroke and factors related to its occurrence among patients along with barriers faced by them in getting admitted to stroke ward. However, the literature fails to inform the key challenges which are causing stroke patients to be admitted to the general ward rather than being cared for in the stroke ward of the hospital. Further, the literature fails to inform the nature of complications created for the patients and nurses for not allowing rapid and effective admission of the stroke patients in the specialised stroke units. Thus, to develop information regarding the gaps, the current study is being developed. This is because irrespective of the admission of the stroke patients in the hospital various complaints are placed by them for not being treated in stroke specialist units.
Design and Methods
The research design is the framework informing the research methods and techniques used by the researcher in formulating the study (Vecchi et al., 2020). In this study, the deductive research approach is to be used in formulating the research instead of the inductive research approach. The deductive research approach is mainly related with the people who are typically associated with scientific investigation of existing phenomenon and theories to gather information in testing the hypothesis which emerges from the theories and information. Thus, the approach is concerned with deriving propositions from the conclusion derived from the existing theories and contexts (Alomran, 2019). In contrast, the inductive research approach involves proposing observation and theories at the end of the research based on the results of review and analysis of the facts and information presented as the result. The approach leads to the development of the theories and concepts at the end of the study (Gordon and Pollack, 2018). The deductive approach is mainly used for perceiving information related to quantitative methods whereas inductive approach is used to perceive information related with qualitative methods (Gao et al., 2018). In this research, the quantitative data from the SSNAP (Sentinel Stroke Audit National Programme) are to be audited to understand the extent of impact of rapid admission and care on the stroke patients in the hospital. Thus, the deductive approach is to be used as it is suitable according to the type of data to be reviewed.
The advantage of deductive approach is that it allows straightforward gathering of data and support time-effectiveness (Pype et al., 2018). Thus, it is used in the current study as it would provide clarified and specific data regarding the rapid admission impact on stroke patients in the hospital within limited time. The other advantage of using deductive approach is that it helps in measuring the validity of the concepts in statistical manner in turn informing clear indication of priorities of the pieces of information gathered for the study. Moreover, the deductive approach assists in generalising the data and allow effective explanation of the causal relationship between different concepts and variables (Azzopardi et al., 2020). Since the study is related to identifying the cause and effect of rapid admission of stroke patients in the hospital on their health, thus the current study is using deductive approach. The indictive approach is not used because it initiates with single observation or inference drawn from similar situation which cannot lead any individual to achieve effective judgement in the diverse world. Thus, its use may lead to develop false conclusions even with the presence of accurate observation due to the incomplete observation developed through the approach (Farghaly, 2018).
Methodology
The evidence from the audit is gathered through a systematic process which includes inspection of the facts as the initial step. The inspection is referred to minute and thorough viewing of the existing data in a careful manner to determine the key factors that are supporting the flow of certain nature of services in the care and avoiding successive operation of actions for the patients (Souliotis et al., 2019). Thus, inspection of all the available records, documents along with physical assets presented by the SSNAP report are to be executed to determine and correct the errors in care delivered. The execution of effective inspection is required as it provides varying degree of opportunity in analysing the reliability, dependability and source of the facts (strokeaudit.org, 2022).
The next step to be followed for gathering evidence from the audit is making a minute observation of the gathered data through inspection. This is because observation is to be made to prioritise the identified issues so that pin points of truth behind the occurrence of certain results can be revealed (Boyle and Keep, 2018). Thereafter, confirmation of the gathered evidence from the audit is to be made to ensure the evidence gathered are evident and similar to the facts presented in the audit. For this purpose, the confirmation is to be made by inclusion of third parties such as other researchers in comparing the data to assure no changes are present between the original information and evidence gathered from the audit. The gathered evident from the audit are to be recalculated to determine confirm its truth.
Research Design
In healthcare, the purpose of the clinical audit is to identify the extent to which the care support is provided as per mentioned governmental standards and procedure to know the extent of efficiency of the services in health improvement of patients. It is also performed to gather evidence for further service improvement to be made in care so that better quality support can be provided to the patient (Burgess, 2020). The benefit of performing clinical audit is that it helps in making more enhanced use of clinical time in delivering care to patients. This is because it helps in understanding the key ways in which the care is to be provided within less time and more efficiency to the patients (Perry et al., 2019). The other need of performing clinical audit is that it assists in demonstrating the positive and negative aspect of any care intervention to others. This is because auditing assists in identifying the extent of success regarding any care delivered along with the negative aspects of the care which led to the lack of fulfilling of the support for the patient (Barnes et al., 2020).
The clinical audit helps in enhancing the number of satisfied patients and enhance the quality of existing care. This is because data gathered in the audit contains specific concerns or issues in care faced by the patients in receiving care along with inform the aspects which were responsible for causing the hindrance in care equality. The information is used in developing service improvement which gradually led to enhancement of the care delivered to the patients where their concerns raised in care are resolved (Paton et al., 2018). The clinical audit also assists in informing the areas in care which are to be improved in practice to make the care delivery more efficient for the patient. Moreover, it helps in providing effective information for continued professional development to professionals responsible in delivering care (Thakor et al., 2020). Thus, the clinical audit is used in the study because it would help in gathering key information regarding the extent to which rapid admission impact the health of stroke patients and factors related to the occurrence of rapid admission.
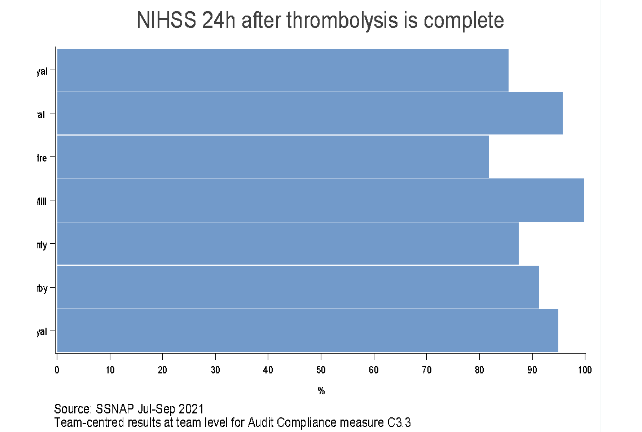
The clinical audit is performed from July to September 2021 involving the routinely admitting team who are responsible in providing stroke services to stroke patients in the hospital. The audit is executed in the Leicester Royal Infirmary, the UK during which the results regarding care of the stroke patients is gathered and represented under 10 domains to inform to the extent the hospital act in delivering care to the patients who suffered stroke. The SSNAP score sheet is used to gather the evidence of audit at the Leicester Royal Infirmary, UK for the care of stroke patients. The SSNAP audit score in the Leicester Royal Infirmary, UK is been focused as it is one of the places where lowest for, of care for stroke patients is identified. Therefore, analysis is to be made to determine the reason behind the low scoring and performance regarding the management of stroke patients in the hospital.
Data Analysis
The key aim of the data analysis in research is converting raw data into effective information while looking at the pattern and anomalies of which complied with the audit standards to be used for analysis (Bourne et al., 2019). In this study, the data analysis of the clinical data developed through clinical audit is to be made through percentage evaluation in which the data are to be converted into percentage for comprising to reach decision. The percentage data are to be presented through existing graphs and charts developed in the audit. This is because it would help to provide pictorial representation of the results gathered and ensure easy comparison with other data to determine its validity (Fast et al., 2020).
Ethical Consideration
In DMU, prior ethical consent is to be gathered before conducting any study. the ethical consideration is important because it indicates the study is performed by following all the moral values and codes (dmu.ac.uk, 2022). Thus, the confidentiality of all the participants in the audit is to be ensured. This is to be executed by avoiding to share any names or details regarding the individual who have provided valued information in the audit. The confidentiality is to be maintained so that no information of the patients can be known by the public which may used for humiliating the individuals and harm them in any context (dmu.ac.uk, 2022). The informed consent from the participant is taken during the audit by mentioning the way their information is to be used and is necessary in the medical field. Since the study is performed for submission at the DMU, thus the ethical consideration followed in the university is being followed.
In healthcare, the four ethical principles to be followed are autonomy, beneficence, non-maleficence and justice. The autonomy is maintained in the audit by avoiding the patients who neglected to provide information for the study. The beneficence which is obligation of creating beneficial care for the patients under all condition is followed in the study by avoiding to share any information that have harm the welfare of the individuals. The non-maleficence is ensured in the study by creating actions that avoids any harm to the participants. The justice is maintained in the study by providing equal opportunity to all patients in informing their opinions regarding the domains used for gathering data.
Findings
The audit data presented by the SSNAP is used because the effectively provide measurement of the efficiency of stroke care in hospitals for stroke patients from the time they arrive at the hospitals until 6 months after they have experienced stroke. The latest data available for stroke care measurement in Leicester Royal Infirmary, UK from the SSNAP report is between July to September 2021 where it is mentioned 314 patients are admitted during the tenure and 208 patients were discharged. Since De Montfort University is in Leicester, therefore, performance of the main hospital in the area to care for stroke patient is evaluated. In addition, it is the place were least care efficiency regarding stroke care is recorded. This is evident from the SSNAP audit where Leicester Royal Infirmary, UK is indicated at level E and marked red compared to others. The E indicates the hospital which have not met the highest standards of care for stroke patients (strokeaudit.org, 2022).
The care standards for stroke patients informs that brain scanning of the individuals who are very sick because of stroke is to be made within one hour of hospitalisation and all stroke patients are to be brain scanned within 12 hours. The brain scanning is important to understand the extent of damage made to the brain due to stroke which is the condition in which blood supply to the brain is reduced or interrupted leading the brain to lack oxygen and nutrients for its effective functioning (Melnychuk et al., 2019). In Leicester Royal Infirmary, nearly 54% of patients are brain scanned within one hour and nearly 91% patients are brain scanned within 12 hours. This indicates that more than half of the patient admitted to the hospital has suffered acute stroke with increased expression of adverse symptoms compared to all patients who have suffered stroke. Moreover, most of the stroke patients admitted in the hospital are brain scanned within 12 hours ensuring faster treatment to most of the individuals.

The stroke unit domain mentions that patients who suffered stroke are to be immediately shifted to stroke unit and 90% of their time are to be spent in the unit. They are to be shifted to the unit within four hours of arriving for care at the hospital. The stroke units are preferred for stroke patients because in the unit the best care is delivered to them which can reduce their occurrence of disability and save their life (Cumming et al., 2019). In Leicester Royal Infirmary, nearly 39% of patients were transferred directly to the stroke unit within four hours as per standard care. This indicates that not all acutely suffering stroke patients are transferred to the stroke unit within the required time. The audit also informs that nearly 79.5% of the stroke patients spent 90% of their time in stroke unit. This indicates that nearly all patients who suffered stroke in Leicester spend most of their time in the stroke unit, but they are not transferred to the stroke unit within the stipulated time mentioned in the standards of care.
The thrombolysis treatment is to be provided to 15-20% of patients at the earliest. It is to be administered up to four and half hours to patients who suffered stroke due to blood clot as is helps in reducing disability (Alper et al., 2020). In Leicester Royal Infirmary, nearly 88% of the patients who required thrombolysis were provided the treatment and nearly 62% of the patients were provided thrombolysis within one hour whereas nearly 39% of patients in the stroke unit were provided thrombolysis within four hours and if required. This indicates that major number of all stroke patients who required thrombolysis treated were provided the intervention with the standard time of 4 hours but few of them were transferred by the time in stroke unit.
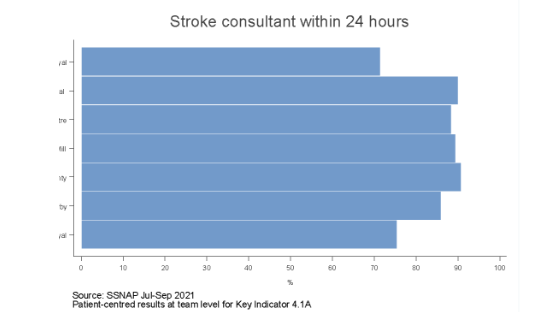
The specialist assessment mentions that stroke patients are to be screened for swallow safety within four hours and allowed to see a stroke nurse and consultant within one day. In case swallow assessment is needed, it is to be performed within 3 days of admission in any stroke patient. It is to assure stroke patients received specialised care and their safety is assessed for swallowing food and drinking (Douiri et al., 2021). The audit results inform that 74% of stroke patients are assessed by stroke consultants within one day and nearly 45% of them were assessed within 14 hours. Moreover, nearly 88% stroke patients were reviewed by stroke nurse within one day and nearly 63% of patients were swallow screened within four hours and nearly 74% of patients were swallowed screened within three days. This indicates that lesser number of patients are reviewed by stroke consultant compared to stroke nurse informing few stroke patients received specialised analysis from the physician.
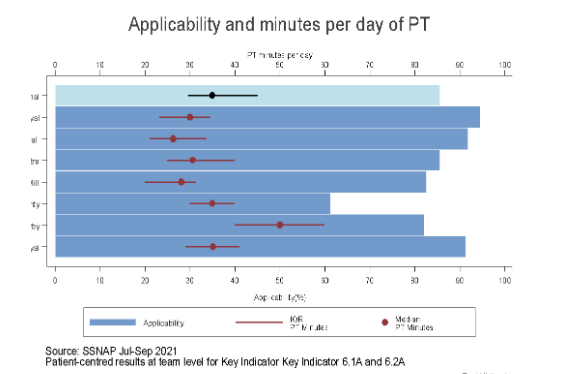
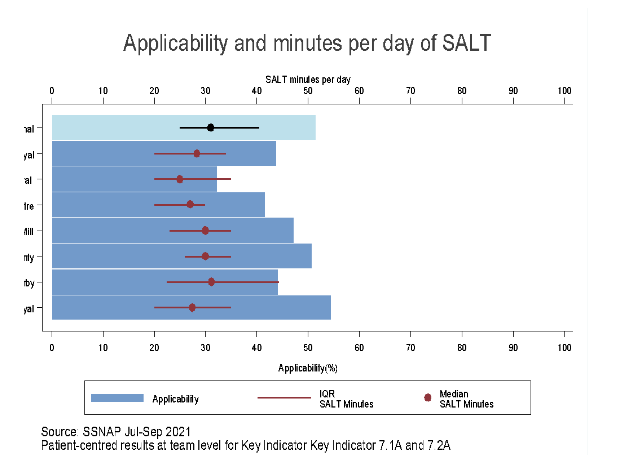
The occupational therapy, physiotherapy and speech & language therapy domains for stroke patients indicates that minimum of 45min of each of the therapy is to be received by stroke patients for at least 5 days in a week during the stroke care. It is required to improve the physical efficiency, balance and movement and speech & language ability of stroke patients (Gittins et al., 2020). The audit data reveals that nearly 91% of stroke patients in the hospital received occupational therapy (OT) and physiotherapy each day for 45 minutes and nearly 90% of patients received OT and 88% of stroke patient received physiotherapy for 5 times a week. This indicates that effective occupational therapy and physiotherapy on daily as well as weekly basis is provided to nearly all stroke patients in the Leicester Royal infirmary. However, nearly 55% of stroke patients are provided speech & language therapy for 45 mins and nearly 36% of patient were provided speech & language therapy for 5 days a week. This indicates that the frequency of providing speech & language therapy among stroke patients is low compared to the other two therapies.

The team working domain mentions stroke patients are to receive health assessment by stroke nurse and at the least one therapist within 24 hours. Moreover, they are to receive all require therapies within three days and all their rehabilitation goals are to be agreed within five days (Whitehead and Baalbergen, 2019). The audit data reveals that nearly 96% of the stroke patients received the agreement of rehabilitation goal within five days and nearly 60% of all stroke patients received nursing, therapy and rehabilitation goals within the limited time set for standard care. This indicates that lesser number of stroke patients received effective multi-disciplinary care and in majority of them the rehabilitation goals were fulfilled.
The standards to be met for discharging stroke patients is nutrition and mood screening of the individual by discharge and continence plan for the patients developed within 3 weeks of arrival at the hospital. This is required as nutrition screening helps in determining risk of malnourishment in the patient whereas mood screening helps in determining their distress level and depression whereas continence screening is essential for care management (Boden-Albala et al., 2019). In nearly 91%, 94% and 99% of stroke patients nutrition screening, continence plan within three weeks and mood assessment is done respectively. This informs that most of the standards of care for discharge are met in nearly all the admitted stroke patients ensuring their safe discharge. The discharge process informs joint health and social care plan to be made with one person who can be contacted in case of emergency is informed (Kable et al., 2019). In nearly 95% of stroke patients in the hospital all these aspects in the domain are fulfilled. This indicates that enhanced discharge process is followed nearly for all the stroke patients in the hospital for their safe discharge.
Service Improvement
The study of the data from the SSNAP audit mention that the concerned areas of practice which is required to be changed are improving patient-centred pathway for admission of all stroke patients in Leicester Infirmary Royal Hospital. The improvement is ensuring stroke patients would remain 90% of their time in the specialised Stroke Unit with allocation of them in the unit within 4 hours and be reviewed by the stroke physician within one day of their admission. This is because 79% of the stroke patients are seen to spent 90% of their time in stroke unit in the hospital but only 39% of the patients are rapidly admitted to the stroke unit (strokeaudit.org, 2022). The lack of quick admission (within 4hours after stroke) of stroke patients in the stroke unit creates risk of low-quality care for them and increases risk regarding their ability to face disability and death (Bhatt et al., 2021). Moreover, the delayed admission of most of the patients in the stroke unit may have lower the percentage of stroke patients being reviewed by the stroke consultant or physicians within one day in the Leicester Infirmary Royal Hospital. According to national figures, 84.4% of the stroke patients are reviewed in the UK one day as per care standards whereas in the Leicester hospital 74% of stroke were assessed within one day indicating low performance of care quality for the patients (strokeaudit.org, 2022). The delayed health assessment of the stroke patients leads the individuals to be at increased risk of experiencing delayed care making them vulnerable to suffer from disability, physical issues and others.
In Leicester Infirmary Royal Hospital, risk to be experienced due to suggested improvement in patient-centred care for stroke patient is that lack of bed availability for normal patients with severe health issues in the hospital. This is because to increase the percentage of early admission of stroke patients, the number of free beds in the stroke units are to be increased so that delay in their admission in the unit is avoided (Anåker et al., 2018). Moreover, it would create risk of early discharge of stroke patients from the specialised unit with the intention of creating bed availability for new patients with stroke in maintaining care standards for them (Jones et al., 2021). The other risk to be created is that increased responsibility and workload would be created on the existing low number of stroke physicians in reviewing many patients at a time in meeting the 4 hours standard time of review. At the current state in Leicester Infirmary Royal Hospital, the ethical consideration to be maintained is ensuring confidentiality of the newly admitted stroke patients while trying to increase their referral to stroke unit within 4 hours of stroke. This is because in increasing the early referral to the stroke unit, the nurses may fail to maintain confidentiality due to carelessness or workload.
In making the service improvement or change management, there are different change models available which could be used in developing strategies to accomplish the change such as Kotter’s change model, Lewin’s change model and others. The Kotter’s model is not to be used because leads to increased use of time in accomplishing service improvement (Fuller, 2019). Thus, the model cannot be followed in performing quick change required in the current settings regarding stroke care management for patients. The Kotter’s model is a top-down step model which discourages any scope for co-creation in achieving change management. It leads to create increased frustration as well as dissatisfaction among the employees as they feel lack of value out of their inability to contribute their views in supporting the change or improvement in the organisation (Wong et al., 2019). In contrast, Lewin’s Change Management model is simple and easy to be used which enhances service improvement to be made within limited time by unfreezing the existing way of working and including new methods of action to deliver services (Gottwald and Lansdown, 2021). The model also includes minimum steps to be followed in achieving change and provides opportunity in making collaborative actions in making the change (Ten Have et al., 2018). The three key stages of Lewin’s Change Model are unfreezing, change and refreezing (Gottwald and Lansdown, 2021).
In the unfreezing stage, the process includes execution of actions so that employees or individuals who are to make the change become prepared and show willingness in making the change. It is the phase in which the employees to make the change in services within an organisation yet express lack of commitment and certainty in making the change but understand the need for change (Antoniou and Vryonides, 2018). The use of SWOT (strength, weakness, opportunity, threat) analysis will be effective way in making individuals to be involved in the change understand its need and feel sense of urgency to execute the change. This is because SWOT analysis assists individuals to identify the requirement and need for change along with invigorate the purpose which breaks the resistance to change. Thus, it helps people involved in the change understand the reason behind the change to be made instead of the actions needed to be changed for the process (Hollingsworth and Reynolds, 2020). Therefore, SWOT analysis of current suggested change improvement which is enhancing patient-centred care for stroke patients so that they can spend 90% of their time in the stroke unit with early referral to the unit and immediate health assessment by the stroke physicians apart from nurses is to be performed. The results are to be communicated to the healthcare employees in the hospital to make them determine the reason for executing the service improvement.
The second stage of Lewin’s model is the phase in which the way actual change to be made is determined and the challenges to be faced in making the change are identified. The stage includes individuals to make the change discuss their role and responsibilities to be played to achieve the common goal for successful change (Canfield and Galvin, 2018). In the change phase, the initial step includes collaboratively working as a team to determine the vision and strategy for the change. In the change, collaboration is important along with effective communication because it assists the team members to share their views and identify the issues along with raise objections regarding the change, enhance trust towards one another and build shared message in making the change (Schot et al., 2020). As argued by Tang et al., (2018), lack of collaboration in making service improvement slower the process of change and raise confusion among employees to make the change. This is because it leads failure of sharing of advanced and strategic ideas and skills from one employee to another for making the change. Moreover, it raises confusion in making the change as employees become disengaged and demotivated leading them unable to decide the way to be followed in reaching the change (Wade, 2020).
The communication is essential in change management because it helps in sharing goals and vision of the change along with communicate the strategies of change between all individuals. It helps in creating mutual understanding and trust between employees in making the change as through interaction they are able to sort out their differences and reach common decision regarding the way to make the change (Davis and Walsh, 2019). However, failure to make effective communication in making change leads the employees to remain unaware of the roles and responsibilities to be played by each of them. It contributes towards duplication of action and disruptive working environment where increased obstacles are faced in making the change (Flach et al., 2020). Thus, in the current service improvement or change management, the use of intranet facility will be allowed so that the employees making the change can privately communicate their roles and change strategies along with goals of care to be reached. In addition, collaboration in making the change will be attained by organising a meeting in the hospital by the leader where the employees are to share their though and know one another to develop trust and collaboration in making the change.
In the change process, the presence of clarified vision and change strategy is important because it indicates the employees making the change regarding the path to be followed and actions to be achieved in making the change in a successful way (Baracchini et al., 2020). The goals of the current change are early admission of the stroke patients in the Stroke Unit on hospitalisation and achievement of early treatment for them with the help of early health assessment by the specialist stroke physicians. The vision is to improve person-centred care for the stroke patients in the Leicester Infirmary Royal hospital. The strategy to be used in achieving the early admission to the Stroke Unit of stroke patients is increasing the number of beds in the unit so that free space is available for the stroke patients to get admitted in the specialised ward instead of the common units. Moreover, the nurses are to be trained to effectively identify the patients who suffered stroke so that they can be immediately referred to the Stroke Unit. The early health assessment of stroke patients within first day of admission is to be achieved through recruitment of increased stroke physicians for evaluating the patients. This is because it would avoid creating workload on the existing stroke physicians and create opportunity for stroke patients to be attended by stroke physicians in time (Gallacher et al., 2018). Moreover, stroke physicians are to be trained regarding the way they can assess and monitor more new stroke patients in a single day without creating any error in the analysis of the patient’s health condition.
In making the change, the obstacles to be experienced are to be identified so that unnecessary barrier in execution of the change is not faced which leads to avoid its successful implementation (Gottwald and Lansdown, 2021). In making the current change, the key obstacle to be faced is lack of space in the stroke unit to implement additional bed so that more stroke patients are admitted in the ward within 4 hours of their stroke as per care standards. In this condition, extra financial resource is to be gathered to ensure extension of space in the Stroke Unit so that specialised care is delivered to the stroke patients. The other obstacle to be face in making the change is lack of concern of the stroke physicians in making early assessment of the patients. This is because they intend to rely on the patient report made by the nurse and determine initial action based on the facts. In order to remove the obstacle, the stroke physicians is to be made aware regarding the gaps in care created for the patients due to their late diagnosis so that they can feel encourage to participate in making the change.
The last stage of Lewin’s model is implementation of change and refreezing actions to be performed in the organisation (Gottwald and Lansdown, 2021). This indicates that the change is to be implemented and the employees are to be made to follow the altered way of working in delivering further care. In order to stabilise the change and refreeze actions, the success stories regarding the change are to be communicated to all at every opportunity. This is to boost all the employees understand the importance of continuation of the change actions in delivering further care to the patients. In refreezing the action, the leaders managing the change are to provide support to all in following the change action and avoid returning to the older measures in delivering care. In leading the change, effective leadership style is to be followed so that the leaders can direct the followers in making the change in a seamless way (Fatima et al., 2020).
In the current change management, the democratic leadership style will be followed instead of the autocratic leadership. This is because autocratic leaders are found to make micromanagement in making change or service improvement in organisation. It is evident as autocratic leaders work alone and have full control to make decisions for strategies of change within minimum scope created for their subordinates to make ideas and choices for change (Burkle, 2019). However, democratic leaders are found to support decision making by allowing bringing various viewpoints from group members to collaboratively decide the way of making service improvement (Idelji-Tehrani and Al-Jawad, 2019). Since in the current service improvement, Lewin’s model is used which states to make collaborative decision for change and overcoming obstacles, thus, the democratic leadership is to be used. The autocratic leadership makes the leader fail to create trust between their followers or team members because of the lack of development of collaboration in decision-making for change. The leadership creates a culture of work based on the views of the leaders which makes their followers feel lack of value at work and show disinterest as well as commitment in executing duties out of disappointment and demotivation (Stanley, 2019). However, democratic leaders support team building and values the opinions of the followers which increases their morale and feeling of being valued. It leads them to have increased zeal and develop better team relationship in working coordinatively to achieve change (Lumbers, 2018). Thus, democratic leadership is to be followed in leading the change.

The democratic leadership is to be followed for encouraging empowerment of medical staffs such as the stroke physician and nurses to ensure 90% time of the stroke patients is spent in the stroke unit where they are admitted directly within fourth pours of their stroke initiation. This is because empowering the subordinates in making the change makes the leaders create a collaborative work environment where no individuals are solely dependent on the leader to make the decision in executing their work. It leads to create greater trust on the leaders and makes the employees feel motivated to show greater creativity in achieving the change (Grzesik and Piwowar-Sulej, 2018). Democratic leadership is to be used in distributing the responsibilities of change among different subordinates based on their skill and knowledge. This is because distribution of responsibilities avoids creating work pressure on the leader or single followers in turn creating a favourable working environment. It helps to create positive working environment where responsibility to make change is shared (Szeto, 2021).
Democratic leadership is also to be followed to create employee engagement in which the subordinates are to engage in decision making process for change in collaborative manner. This is to ensure most effective strategies are followed in achieving the vision and gaols of change (Häyry, 2021). The democratic leaders are also seen to create many opportunities of brainstorming for the subordinates. In case it is executed effectively, the brainstorming leads to development of creative solution for the obstacles to be faced in making the change in turn ensuring smooth service improvement (Ofei and Paarima, 2022). Thus, while acting as democratic leader in the current change management, brainstorming session is to be executed where subordinates are to be asked to share ideas to resolve the raised obstacles in making the change.
Evaluation Strategy
In evaluating the success of the mentioned change regarding stroke patients, the initial strategy to be followed in surveying the stroke specialists and nurses in gathering objective information of their readiness in following the service improvement in care. This is because assessing the readiness of the employee in following the change indicates the extent to which is included in the working culture to be used in delivering care to the patients (Habibzadeh et al., 2019). Moreover, survey will be used for executing the evaluation because it is less time consuming and cost-effective which helps in gathering wider information within limited time and expenditure (Singh et al., 2021). The survey will also be used in making the evaluation because it helps in gathering practical solution for the gathered data. It is evident as survey allows gathering information based on demographic factors in population in different ways and allows the researchers to have freedom in asking any questions to be answered through polls in real-time condition (Habibzadeh et al., 2019). Thus, its use would help to specifically target stroke patients based on their age to determine the extent to which they are able to access early care with the implemented service improvement. The survey is also to be executed as it helps in comparing data from previous to current condition. This assist in measuring the extent of benefit experience due to any change (Singh et al., 2021). Thus, the survey is to be used so that the level of improvement in health of the stroke patients due to implementation of the current service improvement compared to previous service delivery ways for them in the hospital.
The other evaluation strategy to be implemented is accessing patient feedback as well as employee feedback regarding the success of the change through interview and survey questionnaires. This is because accessing feedback regarding change in care from patients helps in determining the extent to which the improvement is being followed in practice after implementation (McAleavey et al., 2021). However, employee feedback assists in evaluating change in care by specifying the rate of effectiveness with which the change process is followed, and additional support required to make the change permanent (Gibbons et al., 2021). In accessing feedback, interview method is to be used because it creates opportunity for the interviewer to examine the non-verbal behaviour of the respondent and develop better understanding of their responses. it also provides flexibility to the researchers in resolve doubts in responses gathered and generate in-depth data regarding success of any service improvement (Adam et al., 2020). In order to assess the change, the compliance and adherence reports of the improvement in care is to be developed. This is because such reports inform regarding the extent to which professionals have followed the improved care ways to deliver support to the patient (Gibbons et al., 2021). Thus, it would mention the extent to which the stroke patients are rapidly admitted to the stroke unit and if the stroke physicians assessing all the new stroke patients in a day which is the standard procedure of care.
Conclusion
The execution of the study concluded that stroke is a leading health issues in the UK as well as all over the world which affects mainly the elderly and adults with minimum chances of affecting the children and younger adults. The stroke leads to create barriers of blood flow to the brain which causes the brain cells to experience lack of oxygen and nutrients. It results them to get damaged and function inappropriately leading individual to develop disability and chances of death. However, the adversities related to stroke in adult are found to be limited with early care and intervention in the hospital.
The admission of the stroke patients within four hours of stroke in the Stroke Unit leads them to get specialised care and support that assist in resolving the blood clot as well as limit the changes of health adversities such as disability and death. However, the searching and analysis of different studies mention that rapid hospitalisation of stroke patients in the Stroke Unit are still not effectively achieved in care. It is evident as in many cases it is seen that the stroke patients are being cared in the general ward and later shifted in the stroke unit on the basis of bed availability to continue their care in the unit. Moreover, acute stroke patients in many cases are found to receive late specialist care which made them vulnerable to experience adverse health consequences. The information is derived through electronic searching of articles based on the keywords and the articles from which this information is shared are involved in the study on the basis of inclusion and exclusion criteria. It has led the information gathered from the articles to be exclusive in providing an overview regarding the hospitalisation condition of stroke patients in the healthcare environment.
A clinical audit performed by the SSNAP regarding stroke patient’s care in the UK from July 2021 to September 2021 is used as evidence to understand the current condition of the care in the UK. The evidence from the clinical audit is shared from the Leicester Infirmary Royal hospital. This is because it is the hospital that was mentioned in the report to have least care standards compared to other areas. The evidence from the clinical audit is gathered through inspection, observation, evaluation and processing. The confidentiality of patients in the clinical audit is effectively maintained by avoiding to share any personal data regarding them in the study or any statistical report. In the SSNAP audit report, the performance of care for stroke patient is evaluated under ten key domains which are brain scanning, stroke unit, thrombolysis, specialist assessment, occupational therapy, speech and language therapy, physiotherapy, team working, standards met by discharge and discharge process.
The analysis of audit data in each of the domain mentioned that the performance was low in stroke unit recruitment, specialist assessment and speech and language therapy. In this context, service improvement is planned in which person-centred care to the stroke patients is intended to be improved by increasing higher stroke patient’s referral to stroke unit and increased stroke patients to receive specialist assessment. In order to achieve the service improvement, Lewin’s Change Management model is being followed. The democratic leadership is used in directing the healthcare staffs regarding the way to achieve the change in services. the leadership style is being followed because it helps the leaders to allow the followers to be equally engaged in deciding the way to achieve the change which makes them work with increased commitment and productivity to support the success of the change.
Recommendations
Improve stroke practice guidelines:
In the Leicester Infirmary Royal Hospital, the stroke practice guidelines are recommended to be improved so that rapid identification of the vascular events in patients can be done and determined which patients have suffered stroke to refer and place them in the stroke unit. In this purpose, the nurses are to be trained regarding the way they can assess the suspected stroke patients within 10 minutes of their arrival to ensure confirmation of the stroke. Thereafter, the stroke patients are to be immediately sent for diagnosis by activation of the Stroke Alter approach in which the EEC and CT scan are immediately executed. The diagnosis reports are to be immediately generated to be reviewed by the healthcare professionals and instructions are to be provided to the nurses to admit the stroke patients in the Stroke Unit and in no other ward.
Increasing speech and language therapy for the stroke patients:
In stroke patients, their ability to communicate their thoughts and words or facing difficulty in understanding words or speech referred to them are dependent on the part of the brain affected by the stroke. However, in either way, speech language therapist makes the stroke patients get equipped with the ability to manage both the issues. The speech-language therapist uses different techniques as well as exercises to assist patients overcome their disabilities of interacting and mentioning their thoughts helping them relearn their communication ways. In Leicester Infirmary Royal Hospital, it is seen that the speech and language therapy is provided to lesser number of stroke patients and it is recommended the services are to be increased. This is because speech-language therapy also leads to increase the self-awareness of the stroke patients in improving their contribution to rehabilitation plan apart from improvement in their ability to communicate. It also helps the stroke patient’s life to feel less frustrating and enhances their recovery process.
Reflection
The personal reflection regarding the process used in developing the study is to be informed through Gibb’s Reflective Cycle. This is because the model allows reflection of situation in systematic manner and determine the actions to be performed to resolve the identified weaknesses along with implement current strength in managing similar situation in future (McCarthy et al., 2021).
Description
In the UK, stroke patients are found to receive delayed admission in the Stroke Unit and early care which led to deteriorate their health and well-being. In this context, a service improvement is planned so that better person-centred care can be ensured for stroke patients in enhancing their health. As a researcher, clinical audit is being performed drawing data from the SSNAP report and factors creating the issues are identified. A change management plan is also developed and evaluation for the success of the change is determined.
Feelings
During the development of the service improvement, I initially felt confused regarding the way factors are to be identified that are creating the deterioration of stroke care services which are to be improved. This is because of watching such huge data presented in the SSNAP report regarding stroke management in different areas and hospitals. However, later on communicating regarding the report with the lecturer, I gained understanding regarding the way to manage the data which led me to feel comfortable and confident in continuing the data analysis of the gathered evidence. Moreover, during gathering of evident from the SSNAP report I felt I lacked effective strategic thinking as I was not able to concisely present all the information.
Evaluation
The thing which went well was that I was able to make effective communication in gathering vital details regarding the formation of service improvement. The communication in change management is important because it helps in generating synergy which promotes enhanced understanding of the actions to be achieved (Chichirez and Purcărea, 2018). The other thing which went well was that active listening was maintained in all context due to which way to evaluate the clinical audit data was easily understood by me when explained by the lecturer. The other thing which went well was that enhanced researching skill was showcased in the study. The researching skill is important because it helps in gathering enhanced evidence to be used in understanding any topic of care and determine effective decision regarding the improvement to be made to provide enhanced quality support to patients (Horntvedt et al., 2018). However, the thing which did not went well was that effective strategic thinking was not made. The lack of strategic thinking in service improvement may lead to avoid use of valuable data to determine the change to be made (Lehane et al., 2019). The other thing which did not went well was effective time management due to which parts of the change management strategies are to be developed in hurried manner which may have led to take wrong decision in service improvement.
Analysis
The communication and active listening went well because I had enhanced understanding of the way verbal and non-verbal interaction are to be made and any interferences in making interactions are to be avoided. The lack of interference and enhanced use of interaction strategy creates smooth flow of data between the communicator and listener leading to enhanced communication to be established (Aceto et al., 2018). Moreover, researching went well because I have enhanced idea regarding the way keywords are to be formulated and articles are to be evaluated along with clinical audit data rare to eb analysed to be presented in the study. However, the strategic thinking did not go well because there was lack of monitoring and controlling. The monitoring and control of any problem helps individuals making change remain focused and have enhanced decision-making ability of the strategies to be implement for successful change (Chilingerian, 2021). The time management did not go well because I was unable to prioritise task and maintain effective schedule.
Conclusion
The learning from the reflection is that effective communication, active listening and researching was established. However, strategic thinking and time management was unable to be achieved in the study process.
Action Plan
In future, under similar condition, the strategic thinking skill is to be improved by being proactive in determining the problems to understand the countermeasures to be taken so that they can optimised and avoided to influence the task. The time management improvement is also to be achieved through effective prioritisation of task and making proper plan to schedule tasks and actions so that they are accomplished within time.
References
- Aceto, G., Persico, V. and Pescapé, A., 2018. The role of Information and Communication Technologies in healthcare: taxonomies, perspectives, and challenges. Journal of Network and Computer Applications, 107, pp.125-154.
- Adam, G.A., Chang, C.H.K., Haibe-Kains, B. and Goldenberg, A., 2020, September. Hidden risks of machine learning applied to healthcare: unintended feedback loops between models and future data causing model degradation. In Machine Learning for Healthcare Conference (pp. 710-731). PMLR.
- Al Khathaami, A.M., Mohammad, Y.O., Alibrahim, F.S. and Jradi, H.A., 2018. Factors associated with late arrival of acute stroke patients to emergency department in Saudi Arabia. SAGE open medicine, 6, p.2050312118776719.
- Alegiani, A.C., Albrecht, S., Rahn, A.C., Köpke, S., Thomalla, G. and Heesen, C., 2019. Reasons for delayed admission after stroke: results of a qualitative and quantitative survey. Patient preference and adherence, 13, p.739.
- Alomran, M., 2019. Implementation of strategic management practices in healthcare sector in Saudi Arabia. Int J Bus Adm Stud, 5(3), pp.131-144.
- Alper, B.S., Foster, G., Thabane, L., Rae-Grant, A., Malone-Moses, M. and Manheimer, E., 2020. Thrombolysis with alteplase 3–4.5 hours after acute ischaemic stroke: trial reanalysis adjusted for baseline imbalances. BMJ evidence-based medicine, 25(5), pp.168-171.
- Anåker, A., von Koch, L., Sjöstrand, C., Heylighen, A. and Elf, M., 2018. The physical environment and patients’ activities and care: A comparative case study at three newly built stroke units. Journal of advanced nursing, 74(8), pp.1919-1931.
- Antoniou, T. and Vryonides, S., 2018. Educational preparation and training of the family caregivers of elderly patients with stroke in the pre-discharge period: A proposed innovation. Cyprus Nursing Chronicles, 18(1), pp.17-31.
- Azzopardi, P.J., Upshur, R.E., Luca, S., Venkataramanan, V., Potter, B.K., Chakraborty, P.K. and Hayeems, R.Z., 2020. Health-care providers’ perspectives on uncertainty generated by variant forms of newborn screening targets. Genetics in Medicine, 22(3), pp.566-573.
- Baracchini, C., Pieroni, A., Viaro, F., Cianci, V., Cattelan, A.M., Tiberio, I., Munari, M. and Causin, F., 2020. Acute stroke management pathway during Coronavirus-19 pandemic. Neurological sciences, 41(5), pp.1003-1005.
- Barnes, T.R., MacCabe, J.H., Kane, J.M., Delgado, O. and Paton, C., 2020. The physical health and side-effect monitoring of patients prescribed clozapine: data from a clinical audit conducted in UK mental health services. Therapeutic Advances in Psychopharmacology, 10, p.2045125320937908.
- Bhatt, N.R., Frankel, M.R., Nogueira, R.G., Fleming, C., Bianchi, N.A., Morgan, O., Chester, K., English, S.W., Janocko, N., Navalkele, D. and Haussen, D.C., 2021. Reliability of Field Assessment Stroke Triage for Emergency Destination Scale Use by Paramedics: Mobile Stroke Unit First-Year Experience. Stroke, 52(8), pp.2530-2536.
- bniresearchgroup.com 2021, BNI database, Available at: https://bniresearchgroup.com/health.html [Accessed on: 24 January 2022]
- Boden-Albala, B., Goldmann, E., Parikh, N.S., Carman, H., Roberts, E.T., Lord, A.S., Torrico, V., Appleton, N., Birkemeier, J., Parides, M. and Quarles, L., 2019. Efficacy of a discharge educational strategy vs standard discharge care on reduction of vascular risk in patients with stroke and transient ischemic attack: the DESERVE randomized clinical trial. JAMA neurology, 76(1), pp.20-27.
- Bourne, E., Short, K., McAllister, L. and Nagarajan, S., 2019. The quantitative impact of placements on allied health time use and productivity in healthcare facilities: a systematic review with meta-analysis. Focus on Health Professional Education: A Multi-disciplinary Journal, 20(2), pp.8-40.
- Boyle, A. and Keep, J., 2018. Clinical audit does not work, is quality improvement any better?. British Journal of Hospital Medicine, 79(9), pp.508-510.
- Büchter, R.B., Weise, A. and Pieper, D., 2020. Development, testing and use of data extraction forms in systematic reviews: a review of methodological guidance. BMC medical research methodology, 20(1), pp.1-14.
- Burgess, R., 2020. Introduction: Foundations, tradition and new directions—the future of clinical audit in a new decade. In NEW principles of best practice in clinical Audit (pp. 1-21). CRC Press.
- Burkle, F.M., 2019. Character disorders among autocratic world leaders and the impact on health security, human rights, and humanitarian care. Prehospital and disaster medicine, 34(1), pp.2-7.
- Campbell, B.C., De Silva, D.A., Macleod, M.R., Coutts, S.B., Schwamm, L.H., Davis, S.M. and Donnan, G.A., 2019. Ischaemic stroke. Nature Reviews Disease Primers, 5(1), pp.1-22.
- Canfield, C. and Galvin, S., 2018. Bedside nurse acceptance of intensive care unit telemedicine presence. Critical Care Nurse, 38(6), pp.e1-e4.
- Chen, J., Li, S., Zheng, K., Wang, H., Xie, Y., Xu, P., Dai, Z., Gu, M., Xia, Y., Zhao, M. and Liu, X., 2019. Impact of smoking status on stroke recurrence. Journal of the American Heart Association, 8(8), p.e011696.
- Chen, J.J. and Xu, G.L., 2020. Smoking and stroke. Journal of Medical Postgraduates, pp.454-459.
- Chichirez, C.M. and Purcărea, V.L., 2018. Interpersonal communication in healthcare. Journal of medicine and life, 11(2), p.119.
- Chilingerian, J., 2021. The discipline of strategic thinking in healthcare. In Managing and leading in the allied health professions (pp. 191-226). Routledge.
- cochrane.org 2021, Cochrane Library, Available at: https://www.cochrane.org/ [Accessed on: 24 January 2022]
- Cumming, T.B., Churilov, L., Collier, J., Donnan, G., Ellery, F., Dewey, H., Langhorne, P., Lindley, R.I., Moodie, M., Thrift, A.G. and Bernhardt, J., 2019. Early mobilization and quality of life after stroke: findings from AVERT. Neurology, 93(7), pp.e717-e728.
- Davis, M.B. and Walsh, M.N., 2019. Cardio-obstetrics: Team-based care to improve maternal outcomes. Circulation: Cardiovascular Quality and Outcomes, 12(2), p.e005417.
- dmu.ac.uk 2022, Research requiring ethical approval, Available at: https://www.dmu.ac.uk/research/ethics-and-governance/research-requiring-ethical-approval.aspx [Accessed on: 28 February 2022]
- Douiri, A., Muruet, W., Bhalla, A., James, M., Paley, L., Stanley, K., Rudd, A.G., Wolfe, C.D., Bray, B.D. and SSNAP Collaboration, 2021. Stroke care in the United Kingdom during the COVID-19 pandemic. Stroke, 52(6), pp.2125-2133.
- ebsco 2021, CINHAL, Available at: https://connect.ebsco.com/s/article/CINAHL-Databases-Basic-Searching-Tutorial?language=en_US [Accessed on: 24 January 2022]
- Farghaly, A., 2018. Comparing and Contrasting Quantitative and Qualitative Research Approaches in Education: The Peculiar Situation of Medical Education. Education in Medicine Journal, 10(1).pp.45-90.
- Fast, O., Dosani, A., Uzoka, F.M., Cuncannon, A. and Cheav, S., 2020. Improving sterile processing practices in Cambodian healthcare facilities. Infection prevention in practice, 2(4), p.100101.
- Fatima, N., Saqqur, M., Hussain, M.S. and Shuaib, A., 2020. Mobile stroke unit versus standard medical care in the management of patients with acute stroke: A systematic review and meta-analysis. International Journal of Stroke, 15(6), pp.595-608.
- Fekadu, G., Chelkeba, L. and Kebede, A., 2019. Burden, clinical outcomes and predictors of time to in hospital mortality among adult patients admitted to stroke unit of Jimma university medical center: a prospective cohort study. BMC neurology, 19(1), pp.1-10.
- Flach, C., Muruet, W., Wolfe, C.D., Bhalla, A. and Douiri, A., 2020. Risk and secondary prevention of stroke recurrence: a population-base cohort study. Stroke, 51(8), pp.2435-2444.
- Fuller, B., 2019. Applying change theory to the flight model. Rethinking Your Unit Council Structure, p.97.
- Gallacher, K.I., May, C.R., Langhorne, P. and Mair, F.S., 2018. A conceptual model of treatment burden and patient capacity in stroke. BMC family practice, 19(1), pp.1-15.
- Gao, F., Thiebes, S. and Sunyaev, A., 2018. Rethinking the meaning of cloud computing for health care: a taxonomic perspective and future research directions. Journal of medical Internet research, 20(7), p.e10041.
- Gibbons, C., Porter, I., Gonçalves-Bradley, D.C., Stoilov, S., Ricci-Cabello, I., Tsangaris, E., Gangannagaripalli, J., Davey, A., Gibbons, E.J., Kotzeva, A. and Evans, J., 2021. Routine provision of feedback from patient‐reported outcome measurements to healthcare providers and patients in clinical practice. Cochrane Database of Systematic Reviews, (10).pp.70-123.
- Gittins, M., Vail, A., Bowen, A., Lugo-Palacios, D., Paley, L., Bray, B., Gannon, B. and Tyson, S., 2020. Factors influencing the amount of therapy received during inpatient stroke care: an analysis of data from the UK Sentinel Stroke National Audit Programme. Clinical rehabilitation, 34(7), pp.981-991.
- Gordon, A. and Pollack, J., 2018. Managing healthcare integration: Adapting project management to the needs of organizational change. Project Management Journal, 49(5), pp.5-21.
- Gottwald, M. and Lansdown, G.E., 2021. 4 Change management and implementing quality improvement programmes. Ebook: Clinical Governance: Improving the quality of healthcare for patients and service users, p.84.
- Grzesik, K. and Piwowar-Sulej, K., 2018. Project Managers’ Competencies and Leadership Styles from the Perspective of Organizations Functioning in Poland. Journal of Entrepreneurship, Management and Innovation, 14(3), pp.35-60.
- Habibzadeh, H., Dinesh, K., Shishvan, O.R., Boggio-Dandry, A., Sharma, G. and Soyata, T., 2019. A survey of healthcare Internet of Things (HIoT): A clinical perspective. IEEE Internet of Things Journal, 7(1), pp.53-71.
- Häyry, M., 2021. The COVID-19 pandemic: Healthcare crisis leadership as ethics communication. Cambridge Quarterly of Healthcare Ethics, 30(1), pp.42-50.
- Hollingsworth, A. and Reynolds, M., 2020. The ED nurse manager’s guide to utilizing SWOT analysis for performance improvement. Journal of Emergency Nursing, 46(3), pp.368-372.
- Horntvedt, M.E.T., Nordsteien, A., Fermann, T. and Severinsson, E., 2018. Strategies for teaching evidence-based practice in nursing education: a thematic literature review. BMC medical education, 18(1), pp.1-11.
- Idelji-Tehrani, S. and Al-Jawad, M., 2019. Exploring gendered leadership stereotypes in a shared leadership model in healthcare: a case study. Medical Humanities, 45(4), pp.388-398.
- Jones, F., Gombert-, K., Honey, S., Cloud, G., Harris, R., Macdonald, A., McKevitt, C., Robert, G. and Clarke, D., 2021. Addressing inactivity after stroke: the Collaborative rehabilitation in acute stroke (create) study. International Journal of Stroke, 16(6), pp.669-682.
- Kable, A., Baker, A., Pond, D., Southgate, E., Turner, A. and Levi, C., 2019. Health professionals’ perspectives on the discharge process and continuity of care for stroke survivors discharged home in regional Australia: A qualitative, descriptive study. Nursing & health sciences, 21(2), pp.253-261.
- King, D., Wittenberg, R., Patel, A., Quayyum, Z., Berdunov, V. and Knapp, M., 2020. The future incidence, prevalence and costs of stroke in the UK. Age and ageing, 49(2), pp.277-282.
- Kuriakose, D. and Xiao, Z., 2020. Pathophysiology and treatment of stroke: present status and future perspectives. International journal of molecular sciences, 21(20), p.7609.
- Lehane, E., Leahy-Warren, P., O’Riordan, C., Savage, E., Drennan, J., O’Tuathaigh, C., O’Connor, M., Corrigan, M., Burke, F., Hayes, M. and Lynch, H., 2019. Evidence-based practice education for healthcare professions: an expert view. BMJ evidence-based medicine, 24(3), pp.103-108.
- Lumbers, M., 2018. Approaches to leadership and managing change in the NHS. British Journal of Nursing, 27(10), pp.554-558.
- Mach, F., Ray, K.K., Wiklund, O., Corsini, A., Catapano, A.L., Bruckert, E., De Backer, G., Hegele, R.A., Hovingh, G.K., Jacobson, T.A. and Krauss, R.M., 2018. Adverse effects of statin therapy: perception vs. the evidence–focus on glucose homeostasis, cognitive, renal and hepatic function, haemorrhagic stroke and cataract. European Heart Journal, 39(27), pp.2526-2539.
- Machin, A. and Hamdan, M., 2018. Factors associated with onset to hospital delay among stroke patients in the emergency department. Indian Journal of Public Health Research & Development, 9(11), pp.1782-1786.
- Markidan, J., Cole, J.W., Cronin, C.A., Merino, J.G., Phipps, M.S., Wozniak, M.A. and Kittner, S.J., 2018. Smoking and risk of ischemic stroke in young men. Stroke, 49(5), pp.1276-1278.
- McAleavey, A.A., Nordberg, S.S. and Moltu, C., 2021. Initial quantitative development of the Norse Feedback system: a novel clinical feedback system for routine mental healthcare. Quality of Life Research, 30(11), pp.3097-3115.
- McCarthy, B., Bessell, N., Murphy, S. and Hartigan, I., 2021. Nursing and speech and language students’ perspectives of reflection as a clinical learning strategy in undergraduate healthcare education: A qualitative study. Nurse Education in Practice, 57, p.103251.
- medline.com 2021, MEDLINE, Available at: https://www.medline.com/ [Accessed on: 24 January 2022]
- Melnychuk, M., Morris, S., Black, G., Ramsay, A.I., Eng, J., Rudd, A., Baim-Lance, A., Brown, M.M., Fulop, N.J. and Simister, R., 2019. Variation in quality of acute stroke care by day and time of admission: prospective cohort study of weekday and weekend centralised hyperacute stroke unit care and non-centralised services. BMJ open, 9(11), p.e025366.
- Oesch, L., Tatlisumak, T., Arnold, M. and Sarikaya, H., 2017. Obesity paradox in stroke–Myth or reality? A systematic review. PloS one, 12(3), p.e0171334.
- Ofei, A.M.A. and Paarima, Y., 2022. Nurse managers leadership styles and intention to stay among nurses at the unit in Ghana. The International Journal of Health Planning and Management.pp.67-90.
- Ohlwein, S., Kappeler, R., Joss, M.K., Künzli, N. and Hoffmann, B., 2019. Health effects of ultrafine particles: a systematic literature review update of epidemiological evidence. International journal of public health, 64(4), pp.547-559.
- Pan, B., Jin, X., Jun, L., Qiu, S., Zheng, Q. and Pan, M., 2019. The relationship between smoking and stroke: a meta-analysis. Medicine, 98(12).pp.45-67.
- Patel, A., Berdunov, V., Quayyum, Z., King, D., Knapp, M. and Wittenberg, R., 2020. Estimated societal costs of stroke in the UK based on a discrete event simulation. Age and Ageing, 49(2), pp.270-276.
- Paton, C., Cookson, J., Ferrier, I.N., Bhatti, S., Fagan, E. and Barnes, T.R., 2018. A UK clinical audit addressing the quality of prescribing of sodium valproate for bipolar disorder in women of childbearing age. BMJ open, 8(4), p.e020450.
- Perry, S.E., Miles, A., Fink, J.N. and Huckabee, M.L., 2019. The dysphagia in stroke protocol reduces aspiration pneumonia in patients with dysphagia following acute stroke: a clinical audit. Translational stroke research, 10(1), pp.36-43.
- Price, A.J., Wright, F.L., Green, J., Balkwill, A., Kan, S.W., Yang, T.O., Floud, S., Kroll, M.E., Simpson, R., Sudlow, C.L. and Beral, V., 2018. Differences in risk factors for 3 types of stroke: UK prospective study and meta-analyses. Neurology, 90(4), pp.e298-e306.
- Pype, P., Mertens, F., Helewaut, F. and Krystallidou, D., 2018. Healthcare teams as complex adaptive systems: understanding team behaviour through team members’ perception of interpersonal interaction. BMC health services research, 18(1), pp.1-13.
- Rutten-Jacobs, L.C., Larsson, S.C., Malik, R., Rannikmäe, K., Sudlow, C.L., Dichgans, M., Markus, H.S., Traylor, M. and International Stroke Genetics Consortium, 2018. Genetic risk, incident stroke, and the benefits of adhering to a healthy lifestyle: cohort study of 306 473 UK Biobank participants. bmj, 363.pp.1-23.
- Schot, E., Tummers, L. and Noordegraaf, M., 2020. Working on working together. A systematic review on how healthcare professionals contribute to interprofessional collaboration. Journal of interprofessional care, 34(3), pp.332-342.
- Shalaby, R.A.H. and Agyapong, V.I., 2020. Peer support in mental health: literature review. JMIR Mental Health, 7(6), p.e15572.
- Singh, A.K., Anand, A., Lv, Z., Ko, H. and Mohan, A., 2021. A survey on healthcare data: a security perspective. ACM Transactions on Multimidia Computing Communications and Applications, 17(2s), pp.1-26.
- Souliotis, K., Golna, C., Mantzana, V., Papaspyropoulos, S., Koutsovasilis, A. and Sotiropoulos, A., 2019. Clinical audit as a tool to optimize contracted private healthcare provision: Testing the waters in resource-deprived Greece. SAGE Open Medicine, 7, p.2050312119838736.
- Stanley, D., 2019. Values-based leadership in healthcare: Congruent leadership explored. Sage.
- strokeaudit.org 2022, National Results: Stroke, Available at https://www.strokeaudit.org/results/Clinical-audit/National-Results.aspx [Accessed on: 28 February 2022]
- strokeaudit.org 2022, Stroke care in England, Wales and Northern Ireland, Available at: https://www.strokeaudit.org/Documents/National/Clinical/JulSep2021/JulSep2021-EAV.aspx [Accessed on: 28 February 2022]
- Szeto, E., 2021. How do principals’ practices reflect democratic leadership for inclusion in diverse school settings? A Hong Kong case study. Educational Management Administration & Leadership, 49(3), pp.471-492.
- Tang, C.J., Zhou, W.T., Chan, S.W.C. and Liaw, S.Y., 2018. Interprofessional collaboration between junior doctors and nurses in the general ward setting: A qualitative exploratory study. Journal of Nursing Management, 26(1), pp.11-18.
- Ten Have, S., Rijsman, J., ten Have, W. and Westhof, J., 2018. The Social Psychology of Change Management: Theories and an Evidence-based Perspective on Social and Organizational Beings. Routledge.
- Thakor, K., Major, V. and Ramlaul, A., 2020. Clinical Audit. In Medical Imaging and Radiotherapy Research: Skills and Strategies (pp. 255-269). Springer, Cham.
- Vecchi, V., Casalini, F., Cusumano, N. and Leone, V.M., 2020. PPP in Health Care—Trending Toward a Light Model: Evidence From Italy. Public Works Management & Policy, 25(3), pp.244-258.
- Wade, D.T., 2020. What is rehabilitation? An empirical investigation leading to an evidence-based description. Clinical rehabilitation, 34(5), pp.571-583.
- Wang, M., Xie, Y., Zhao, S., Wang, Y., Cui, J. and Chang, S., 2021. Association of alcohol consumption with prognosis of ischemic stroke by subtype in different follow-up periods: a hospital-based study in China. Postgraduate Medicine, 133(2), pp.154-159.
- Wang, Y., McKee, M., Torbica, A. and Stuckler, D., 2019. Systematic literature review on the spread of health-related misinformation on social media. Social science & medicine, 240, p.112552.
- Wang, Y., Wang, L., Rastegar-Mojarad, M., Moon, S., Shen, F., Afzal, N., Liu, S., Zeng, Y., Mehrabi, S., Sohn, S. and Liu, H., 2018. Clinical information extraction applications: a literature review. Journal of biomedical informatics, 77, pp.34-49.
- Whitehead, S. and Baalbergen, E., 2019. Post-stroke rehabilitation. South African Medical Journal, 109(2), pp.81-83.
- Wong, Q., Lacombe, M., Keller, R., Joyce, T. and O'Malley, K., 2019. Leading change with ADKAR. Nursing management, 50(4), pp.28-35.
- WSO 2019, Global Stroke Fact Sheet 2019, Available at: https://www.world-stroke.org/assets/downloads/WSO_Fact-sheet_15.01.2020.pdf [Accessed on: 24 January 2022]
- Xia, X., Yue, W., Chao, B., Li, M., Cao, L., Wang, L., Shen, Y. and Li, X., 2019. Prevalence and risk factors of stroke in the elderly in Northern China: data from the National Stroke Screening Survey. Journal of neurology, 266(6), pp.1449-1458.
Looking for further insights on Enhancing Retail Efficiency? Click here.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



