Exploring Well-being in End-of-Life Care
Chapter 1
1.0 Introduction
Researchers are increasingly gaining interest on the well-being and experiences of health and social workers involved in providing critical services to patients, so that their experiences, as well as the experiences of their patients, can be improved (Maben et al., 2012). Moreover, Maben et al. (2012) comments that staffs providing end of life care are more predisposed to high levels of emotional exhaustion, and therefore, they require much attention. Fundamentally, end-of-life care is defined as a component of palliative care concerned with patients facing life-threatening illnesses and has a life expectancy of six to twelve months (Worldwide Palliative Care Alliance, WPCA, 2014; The Gold Standards Network, 2011). According to WPCA (2014), end-of-life care enables the patients to die in dignity, peace, and comfort. The main aim of this study is to explore existing evidence on the experiences of nurses providing end of life care to patients in community settings. The study will explore existing qualitative and quantitative evidence on this topic, using the extended literature review methodology to achieve its objectives. The entire research report is organized in chapters. Chapter one will give background information on the study topic, as well as a rationale for the study. Chapter two will highlight the research methodology, techniques, and tools used to complete the study, while chapter three will present the main findings of the study. The penultimate chapter four will present a discussion of the study findings. Chapter five, the last chapter, will give a conclusion as well as the strengths and limitation of the study.
1.1 Background and Rationale
Global statistics by Edkind et al. (2017) indicate that in the next 20 years, at least 75% of patients with end-of-life stage illnesses should benefit from palliative care; meaning that the global society is still expecting quality care services delivered by community care nurses handling such patients. Furthermore, the speculated increase in end-of-life care in the near future calls for countries to put in place various essential elements of care for such patients. Besides a range of physical discomfort that people with end-of-life illnesses face (Button et al. 2016 & Ekstra et al., 2016), their lives are marred with a variety of spiritual and psychosocial issues (Ben et al. 2010, Reyneirs et al., 2016). Hence, as their diseases progress to the end of their lives, they require more health services (Abarshi et al. 2010, Teno et al. 2013). Consequently, as statistics by Bekelman et al. (2016), Cohen et al. (2008) indicate, a significantly large number of patients with chronic illnesses die in acute care hospitals, instead of, or before being transferred to palliative care. Ideally, palliative care settings are the most appropriate for patients with end-of-life illnesses because acute care settings may not have specialized equipment or wards to deliver such care. Department of Health (2013) & William (2014) found that with the increasing number of patients developing end-of-life stage illnesses, the mortality rates of patients in palliative care settings or hospices are lower than those in non-palliative care settings. Furthermore, the results a study by Office for National Statistics (2015), drawing participants in the whole of United Kingdom (UK) revealed that only 6% of patients with end-of-life stage illnesses who dies were from hospices. These findings reveal the crucial role of palliative care pathways on the health and well-being of patients with end-of-life stage illnesses. Existing research evidence shows mixed results regarding the experiences of staffs caring for patients with end-of-life stage illnesses. For example, McCloskey & Taggart (2010) reported that nurses providing end of life care to children do have positive experiences, including good relationships and positive experiences with them and their families. Similar observations were made by Reid (2013) who also observed that such experiences contribute to the improved psychosocial and physical well-being of the patients. Conversely, Papadatou et al. (2009) found various challenges that impact on the staffs' well-being at the workplace, including poor and frustrating service coordination, staff shortage, and stressful work environments. Moreover, according to Bartholdson et al. (2015), the staffs particularly face significant challenges with regards to making end-of-life decisions, end of life care communication and symptom management. Papadatou et al. (2009) also observed reports by many staffs that they find it a challenge to express their misgivings in public because they fear that it may impact on their professional reputation, as well as on patients’ family. According to Korzeniewska et al. (2010), an experience of these challenges directly correlates with the well-being of the staff as well as patient experience. Therefore, it is vital to have a regular evaluation of staff well-being, to ensure that solutions are consistently offered to the challenging experiences they encounter. Similarly, an assessment of staff experience would be critical in improving the positive experiences they encounter that patients can have better care.
Although the vital role of staffs’ experience evaluation towards quality patient care and caregivers’ well-being (Papadatou & Bellali, 2002), the current study deems that there are conflicting pieces of evidence on the nature of these experiences. Moreover, much of the existing research (i.e. McCloskey & Taggart 2010, Papadatou et al 2001, Papadatou & Bellali 2002) concentrate on the impact of quality care to the well-being of patients with end-of-life stage illnesses, leaving a research gap on the nature of experiences faced by caregivers especially within the palliative care setting (McConnell et al, 2016). The current study seeks to bridge this gap by conducting a review of evidence on these experiences, and how the staffs cope with the experiences they encounter. Whereas the end of life care is usually considered synonymous with palliative care Maben et al. (2012), this study finds an end of life care as both palliative care and the point when the patient is actively dying.

1.2 Research Aim
The main of this study is to explore evidence on the experiences of a nurse in caring for palliative patients in community care settings
1.3 Research question
What are the experiences of nurses at the end of life care in community settings?
1.4 Research objectives
i. To explore the experiences of nurses when caring for patients with end-of-life stage illnesses in community care settings
ii. To identify the impact end-of-life care nurses’ experiences on the quality of care
iii. To explore the coping strategies of palliative care nurses in community settings
Chapter 2
2.0 Research Methodology
The main focus of the current study is to identify, critique, and evaluate existing evidence on the experiences of nurses delivering care to end of life patent in community palliative care. Palliative care has remained to be an exciting topic in healthcare research, especially considering the vital role that such care contributes to the lives and well-being of the patients involved. Therefore it is of great importance to evaluate the existing evidence on the experiences and coping strategies of nursing staffs dealing with patients in such settings, especially patients who are on the end of life stages of their illnesses. In the spirit of evidence-based practice, the researcher has used systematic approaches and search strategies in identifying the relevant literature sources for review. Furthermore, literary sources have been retrieved from various online databases that will be described shortly. This study adopted the ‘extended literature review’ methodology to conduct a critical review of existing empirical research evidence on palliative care and nurses’ experiences while providing this care to patients at the end of life stages of their illnesses. Similar to other types of reviews such as systematic reviews, extended literature reviews adopt predetermined research objectives achieved through a systematic search and analysis of literature. However, the process of search and selection of literary sources in extended literature reviews are more straightforward and less involving as in the systematic reviews (Hoffmann et al., 2009). Nonetheless, the researcher was motivated towards extensive literature review because of its reliance on high-quality evidence. Hence, the reasons above, and rationales provided herein, justified the selection of extended literature review methodology to achieve the objectives of the current study.
2.1 The Research Question
Baumeister (2013) argues that the development of the research question in clinical research should be based on a robust theoretical framework for purposes of developing a strong base of evidence. Hence, the current study relied on the PEO (Population, Exposure, and Outcome) framework that consists of various variables related to the research topic. The following table illustrates how PEO was used to develop the current research question:
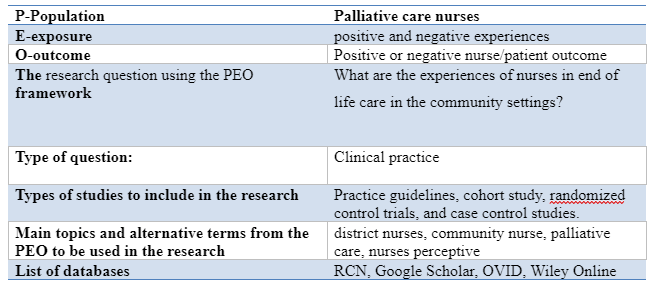
The research question’s primary focus is on the evaluation of evidence regarding the experiences of palliative nurses’ experience with patients facing the end of life stage illnesses.
2.2 Search Terms
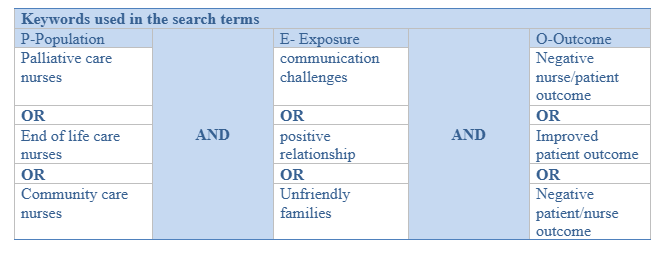
According to Bernard (2011), effective retrieval of literary materials from online databases requires a systematic approach towards the search process. Ideally, this process begins with the identification keywords usable in the search process – which also represent the key components of the research question. For instance, the current research question can be divided into five key variables, namely: Experiences, nurses, end of life, palliative care, and community setting. An alternative term is then developed for each of these variables to derive the search terms. Therefore, the keywords represented the critical elements of the research question. For an effective search process, the researcher relied on Boolean operators (i.e., AND and OR) to broaden or narrow the search process. Furthermore, the Boolean operators were useful in combining the search terms, to include specificity, precision, and sensitivity in the search process. For instance, ‘OR’ was used to narrow the search by combining alternative words, while ‘AND’ was used to broaden the search by combining unrelated words. The following table illustrates the use of Boolean operators in the search process:
2.3 Inclusion/Exclusion Criteria
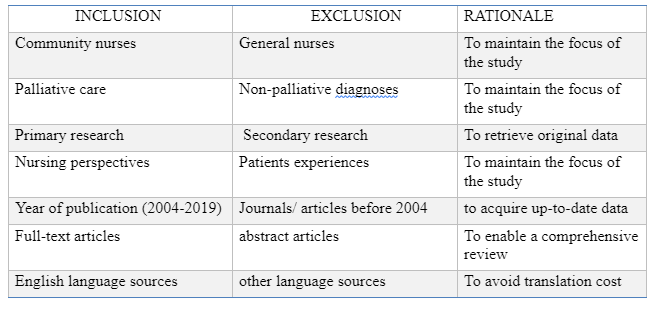
For credibility purposes, the researcher relied on predetermined inclusion/exclusion criteria to select the relevant literary materials for further review. Furthermore, the criteria were selected based on the reason that the search process could likely unveil an overwhelming number of literary materials, thus the need to eliminate some. For instance, because palliative care practice has undergone rapid change in terms of evidence-based practice, the study was limited to sources published between 2004 and now. This was to ensure that the most current sources were included for review. Likewise, a rigorous literature review requires an evaluation of the full literary material, thus the need for sources retrievable in full text (Hoffmann et al., 2009). Consequently, the search process was limited to studies that could be retrieved in full text. Language is an essential element of communication, especially when the handling evidence that could inform practice (Hoffmann et al., 2009). Therefore, the researcher limited the search to sources that were published in the English language to make it easier to understand the content. Furthermore, the researcher excluded causes published in other languages to avoid incurring translation costs. Other types of sources excluded from the study included: studies on community nurses, studies focusing on palliative care, primary research, and studies on nurses’ experiences. The following table illustrates the inclusion/exclusion criteria with their respective justification:
2.4 Search Strategy
Developing a firm search strategy is an essential part of a literature review process because it helps in the identification of relevant literary sources for the development of evidence (Bernard, 2011). Hence, in the current study, the researcher developed the search strategy based on the underlying keywords, as well as the inclusion/exclusion criteria. The initial literature search was conducted in various online databases, including the Royal College of Nursing database, the Willey Library, Google Scholar, and Ovid. The search process involved the use of keywords combined with Boolean operators, as illustrated in figure 2 above. Ideally, the researcher chose to use online databases based on various fundamental reasons. First online databases could enable the use of specific words (keywords) to retrieve relevant literature, thereby making the search process more uncomplicated than it would be if the searches were conducted manually in a physical library (Hoffmann et al., 2009). Secondly, according to Baumeister (2013), the process of a literature search on online databases is replicable and more comfortable to follow. Last but not least, these databases contain abundant and relevant literature material in nursing and medicine, making a good source of literary evidence (Hoffmann et al., 2009).
2.5 Study Selection
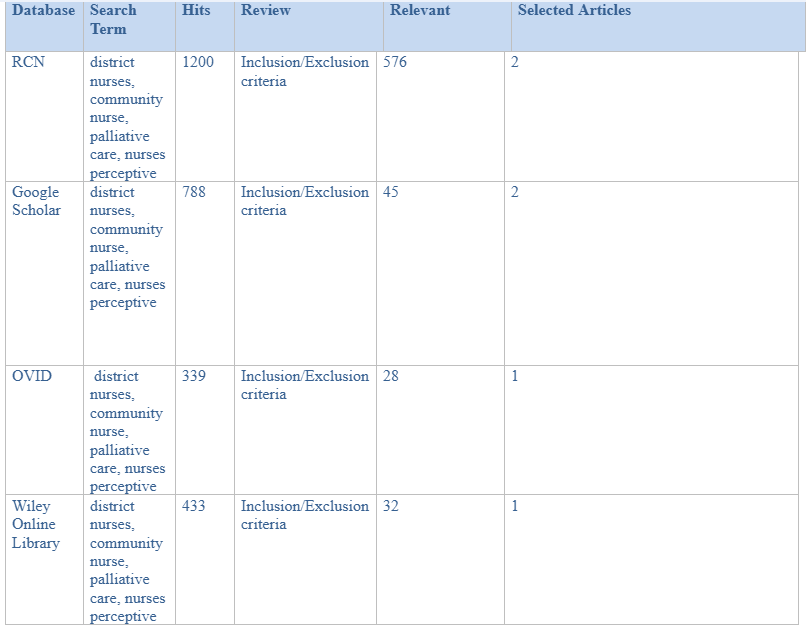
The initial search process in the RCN database yielded a total of 8543 citations. However, when the sources were subjected to inclusion/exclusion criteria, 567 relevant literary materials remained. The researcher selected two articles from this database. The second search activity was conducted in Google Scholar, and 788 sources emerged in the first instance. However, when these sources were subjected to the inclusion/exclusion criteria, only 45 sources appeared to be relevant. The researcher picked two sources from this database. The next search process was conducted on OVID, where 339 literary materials emerged in the first instance, while 28 remained to be relevant after being subjected to the inclusion/exclusion criteria. One source was selected for inclusion in the review. The search was then conducted on Willey Online Library, where 433 were retrieved in the first instance while 32 sources remained after being subjected to the inclusion/exclusion criteria. The author selected one source from this database. Ultimately, a total of 6 journal articles were selected for inclusion in the review. The following table illustrates the search process:

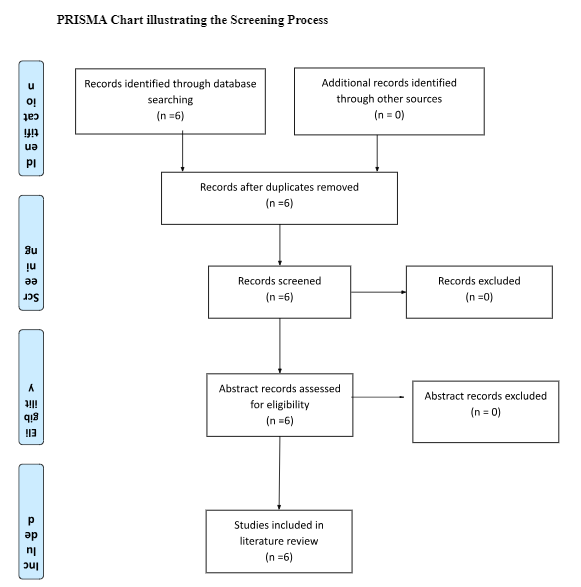
There was a thorough screening on all the retrieved journal articles to ensure that they met the inclusion/exclusion criteria. During the screening process, the author was keen of the materials’ abstracts, title, and the full-texts for the identification of any fault that could affect the relevancy and suitability of the study. The following PRISMA flowchart illustrates how the screening process was conducted:
2.6 Critical Appraisal
According to Baumeister (2013), developing quality evidence in literature review for purposes of evidence-based practice requires the use of high-quality sources of data. Hence, researchers rely on critical appraisal techniques to appraise the quality and reliability of selected literary sources before actually using them as sources of data (Hoffmann et al., 2009). Furthermore, critical appraisal enables researchers to identify the relevance of the selected process to the underlying research question a well as to healthcare practice. Fundamentally, the process of a literary-critical appraisal involves an evaluation of the strengths and weaknesses of the literary sources to identify whether the sources are relevant to the study. Various tools can be used to appraise the sources critically, but the most common one, according to Baumeister (2013) is the Critical Appraisal Skills Program (CASP). CASP evaluates the credibility, relevance, and rigour of evidence in each literary material to determine their suitability for review (Bernard, 2011). It is based on a checklist of 10 questions categorised into three sections, namely: section A; what are the results? Section B; Aare the results valid? And Section C; are the results locally applicable? Hence, the author selected the CASP tool to evaluate the methodological quality of the study in a process that involved a second researcher for purposes of eliminating bias. The CASP table presented in Appendix 1 outlines the CASP scores of each journal article subjected to the critique. The author adopted an elaborate scoring system illustrated below to ensure that all the selected journal articles were relevant.
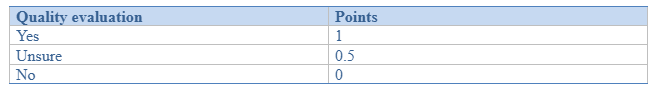
Based on the above-illustrated scoring system, the articles were awarded the scores as follows:
High quality sources -9 &10 points
Moderate quality sources-7.5 & 9 points
Low quality sources-less than 7.5 points
Ultimately, all the six included papers were of moderate quality.
2.7 Data synthesis
The researcher relied on the data extraction tool illustrated in Appendix 2 to extract vital information about each study included in the review. The key focus of the tool was: name of the author(s), study methodology (i.e., study sample, data collection, and data analysis) results of the study, conclusion, and implication of the findings to practice. The researcher then used the grounded theory approach to synthesise the extracted data. According to Hoffmann et al. (2009), the grounded theory enables a systematic approach to data synthesis and allows the researcher to relate the findings to the phenomenon under investigation. Ultimately, because the selected sources were based on different study methodologies, thematic analysis was used to identify relevant themes emerging from the data and using them to answer the research questions.
Chapter 3
3.0 Findings
Non-palliative care settings have shown more mortality rates compared to palliative care settings. However, there is a shortage of knowledge on how care is delivered within the palliative care settings, especially with regards to patients with end-of-life stage illnesses. Against this backdrop, McConnell & Porter (2017) conducted a study to explore the nurses’ experiences of providing care to children with end-of-life stage illnesses in a hospice setting. The researchers adopted a qualitative research design involving interviews and focus group discussions as the main methods of data collection. The study targeted 40 nurse participants using the purposive sampling method. Furthermore, participant nurses were those offering either palliatives or specialist care services such as symptom management, family support, and general end-of-life care to the children in Northern Ireland. The study found mixed (i.e., rewarding and challenging) results regarding the experiences of nurses offering palliative care to patients with end-of-life illnesses. With regards to rewarding experiences, McConnell & Porter (2017) found that in the course of executing their duties, the nurses find it rewarding to make a difference in the lives of the patients and their families. Based on the acknowledgment that end of life stage illness present the patients and their families with hard times, the nurses reported that they find it fulfilling to make a difference in the lives of the patients and their families through emotional, physical, and spiritual support, tailored to meet their needs. Conversely, some of the challenging experiences reported in the study by McConnell & Porter (2017), included identifying the most appropriate medications to enhance end-of-life care, and maintaining effective communication with the patient and their families due to fear of communicating the wrong message. Ultimately, it emerged from the study by McConnell & Porter (2017) that despite the challenging experiences faced by nurses caring for this particular group of patients, hospices provide the best setting and models for mitigating or coping with the challenging experiences. Some of the models and coping strategies include regular training and organizational support for quality palliative care. Moreover, it emerged from the study that some of the critical strategies for improving the experiences include advanced training on communication skills and knowledge sharing among the nurses to enhance the quality of care. The study also recommended policy initiatives towards formal and open organizational support, especially with regards to communication and symptom management in patients with end of life stage illness. Adequate development of skills and expertise also emerged as an essential aspect of palliative care.
In Europe, the increase in older people with chronic disease has led to an increasing need for palliative care (WHO, 2011). Based on the argument that assistant nurses play an essential role in the care delivery within the palliative care setting, Udo et al. (2018) conducted a study to explore the experiences of assistant nurses who deliver palliative care to patients with end of life stage illnesses within residential care settings. The explorative qualitative study used semi-structured interviews to collect data from participants who were selected from two residential care settings in Sweden. Eight participants were selected through purposeful sampling methodology based on three criteria, including assistant nurses with at least one year experience in residential care and be available for the study when called upon to participate. After undertaking 20-50 minute interviews with all the participants, the researchers found impressive results with regards to the experiences of assistant nurses delivering end of life palliative care that could be categorised into three main themes, namely experiences related to being part of a team experiences pertaining to delivery of psychological support, and experiences related to care environment. With regards to teamwork, the researcher found that assistant nurses in palliative care settings caring for end of life stage patients experience successful coordination with both the patients and their families, as well as between themselves. Furthermore, a smooth running of the care process was perceived by the participants as the provision of quality, safe and dignified care service to the patients. Conversely, Udo et al. (2018) also found that sometimes assistant nurses have negative experiences such as poor inter-professional coordination and lack of effective plans on teamwork coordination. With regards to the provision of psychological support, Udo et al. (2018) found that assistant nurse had positive experiences when they can offer to conform to patients and their families, especially when families are invited to stay with the dying patients until they die. Whereas some of the participants in Udo et al.’s (2018) viewed that staying with the patients until they die was challenging to the families, they considered it an essential aspect of care and either way, fund it challenging to offer psychosocial support at that particular time. With regards to the care environment, Udo et al. (2018) found that assistant nurses have positive experiences when they realise how different environmental factors such as photography, ornaments, and paintings could help in enhancing patients’ memory and opening them up for more dialogue. Conversely, Udo et al. (2018) found negative experiences related to the care environment, such as excessive noise, which contributed to a lack of peace and worries among the patients. Ultimately, the study concluded by highlighting the vital role that collaborative and consultative care play in enhancing positive experiences of care and consequently promoting the delivery of quality care to patients with end of life stage illness.
Provision of palliative care in rural communities is an essential way of ensuring accessibility of care regardless of the underlying health inequalities. Based on the evidenced challenges experienced by nurses delivering palliative care in rural communities, Kaasalainen et al. (2014) launched a study to investigate the experience of nurses who provide palliative care to individuals with end- of life stage illnesses in rural settings as a follow up to an earlier study by the same authors conducted in 2012. The study employed qualitative research methodologies to gather data from 21 community nurses through telephone interviews. Results by Kaasalainen et al. (2014) revealed various experiences encountered by nurses working in rural communities, as well as how these experiences influence the nurses’ ability to play their roles of delivering quality care to the cities. Kaasalainen et al. (2014) also revealed how nurses in these settings play vital roles in providing a variety of care and support services including mental, physical, spiritual and emotional care regardless of the challenges associated with transitioning from one role to the other and coordinating with other care professionals. Moreover, Kaasalainen et al. (2014) highlighted the challenges associated with the remoteness and rurality of their areas of practice which affects their ability to swiftly move in to assist patients who may be in critical health conditions. Specifically, the study found that delivering palliative care in the rural setting was characterized by inaccessible roads and lack of adequate transport facilities to enable them to reach the patients or transport vital materials for delivery of care. The critical role that nurses play in coordinating and delivering palliative care to patients at the end of life stage illness can never be overemphasized. Consequently, Kaasalainen et al. (2012) initiated a study to explore the nurses’ experiences of barriers and enables of palliative care to patients with end of life stage illness to patients living in rural areas. The study was based on a qualitative descriptive methodology to gather qualitative data from nurse participants. Based on substantial ethical grounds (i.e., based on gaining ethical approval from an ethics committee), the researchers partnered with a prominent nursing organization in Canada that offers various palliative services and other community development services. Kaasalainen et al. (2012) relied on purposeful sampling methodology to select a diverse group of 21 nurse participants who had the following characteristics: had participated in various levels of palliative care, had taken part in multidisciplinary palliative care activities, had varied educational backgrounds and had different levels of job satisfaction. While purposive sampling may have exposed the study outcomes level of bias, the diversity of participants selected through this methodology would have contributed to a rich data (Apan et al., 2012). The results revealed a variety of insights on the experiences of the nurses that could enhance or hinder the delivery of effective palliative care. For instance, the study found that nurses experienced challenges related to the nature of rural communities, whereby they had to travel long distances into remote areas to provide care especially during adverse weather conditions such as the winter times. The long distances led to delays in delivering care, especially in cases where care was urgently needed. The study also found that nurses experience challenges related to coping up with the cultural beliefs of patients and their family members, poor attitude towards car and the caregivers, as well as an emergence of conflicts among the care teams Moreover, Kaasalainen et al. (2012), found that sometimes the nurses had to play a generalist role, providing all types of care to the patients regardless of their specialties. A reported by the respondents, the need to provide generalist care contributed to difficulties in handling individual nurse’s caseload and thereby affecting the optimal delivery of palliative care. Kaasalainen et al. (2012) found that apart from the challenges mentioned above, the nurses also experienced system-related challenges including working in underserviced environments and shortage of nurses which not only affects the quality of care but also affects the quality of dying experience of patients with end of life stage illnesses. However, the generalizability of these findings are limited to the fact that the study was only conducted in one province in Canada, and only concentrated on responses from nurses only without considering perceptions of other support staffs such as physicians. Moreover, the respondents were sampled from only one community nursing organization, and therefore, the findings related work environment may not apply to those from other community nursing organizations.
People with dementia may also require end of life care at some stage of their illness. However, existing research reveals that sometimes carers my not be able to provide quality end of life care for these patients due to various experiences they encounter in their work environment. Against this backdrop, Dening et al. (2012) investigated to explore the challenges experienced by nurses providing end of life care to patients with dementia, and how these challenges affect the delivery of quality care to their patients. The study targeted recently bereaved dementia care professionals involved in caring for dementia patients at the end of life stage of the illness. Whereas the researchers sought ethical approval from the ethics committee, the study was later considered by the committee as a service evaluation, and therefore, no ethical consent was deemed to be necessary. However, this did not disapprove the researcher’s intent to base the study on ethical grounds (Given, 2008). Nonetheless, the study included a wide range of cares, including family cares and social cares that were recruited from mental healthcare institutions and local authority day-care organizations through purposive sampling. Whereas purposive sampling exposed the study to a considerable level of selection bias, the researchers selected participants with a variety of social, economic, cultural background to represent the local population. This diversity would enhance the generalizability of the study, considering its focus in perception and experiences of the respondents (Gisselle & Lotte, 2018). However, the researchers employed a different sampling strategy, i.e., snowballing sampling strategy to select the health and social care professionals, including nurses. While snowball sampling exposed the study to the impossibility of making inferences about the target population Hendersthot et al. (2014), the researcher again ensured that the samples emerged from a variety of care services including ambulance care, home care, hospice staff, and admiral nurses. According to Given (2008), this enhances the generalizability of the study findings. Ultimately, Dening et al. (2012) found various experiences from the nurses that acted as barriers to care. For instance, with regards to care pathways, it was reported that patients with end of life stage dementia have complex social and medical needs that are difficult to meet in the realm of poor coordination. Dening et al. (2012) also reported challenges regarding out-of-hours care experienced by admiral nurses who sometimes were not aware of the severity of the patient condition. Poor coordination was also reported in instances where ambulance response calls were made in the absence of other support services, leading to hospital admissions due to limited alternatives. Hospital admission was associated with adverse outcomes for patients with end of life stage dementia, emphasizing the negative impacts of poor care pathway coordination. Dening et al. (2012) also reported experiences related to staffs skills and training. Notably, it was observed that in the hospice setting, the nurses admitted to not having adequate skills and knowledge on how to effectively communicate with the patients and their families, as well as skills for managing the behavioural problems within the care setting. As highlighted by Dening et al. (2012), a lack of communication and behaviour management skills contributed to several negative experiences including violence and attacks on nurses by the patients due to the use of poor restraining techniques.
Nonetheless, the study by Dening et al. (2012) has several strengths and limitations that are noteworthy. For instance, the study used a relatively large sample of participants with different specialities and offering care at various capacities (i.e., a whole systems approach), which enhanced the generalizability of its findings. However, the study participants were predominantly female carers and nurses, and this may affect the generalizability of the results to male carers. The final reviewed (Bainbridge & Seow, 2018) study was focused on the experiences of care nurses offering care to patients in their last three months of life. The main aim of Bainbridge & Seow (2018) was to explore the experiences of delivering an end of life palliative care to bereaved patients in a hospice setting. A selected group of bereaved caregivers was selected to participate in a survey evaluating various aspects of their perceptions and experiences if care delivery to patients in their last three months of life. The inclusion criterion for participants was the ability to read and write in the English language, while ethical approval was sought from the university’s ethical committee. Ultimately, Bainbridge & Seow (2018) found that hospices provide the best experience of care for end of life stage patients (as proposed by 80% of the respondents) compared to other settings such as home and hospitals. Moreover, the respondents reported that hospices allow for the best experience of caring for end of life stage patients because it provides enough help, material, and equipment to meet the patients’ needs. Moreover, Bainbridge & Seow (2018) reported positive nurse experience emanating from the availability of a good bed area surrounding environment and adequate privacy.
Chapter 4
4.0 Discussion and Analysis of Findings
The reviewed studies provide essential aspects of palliative care with regards to nurses’ experience in community care settings. Based on thematic analysis, the study results offer a wide variety of data regarding palliative care delivered to children and adults, addressing the lack of research evidence on the setting of child and adult palliative care. While the themes will not be discussed in both adult and children care separately, there will be an exploration of such experiences in two main categories of themes (i.e. positive and negative experiences) while highlighting their implications to practice.
4.1 Positive Experiences
4.1.1 Emotional Relationships with the patients
The reviewed literature indicated that nursing staffs feel a rewarding experience when they can create meaningful and emotional relationships with the patients and their families. These findings corroborate with the results of Korzeniewska-Eksteowicz et al. (2010) who also found that the creation of a meaningful relationship with patients with end of stage illnesses are emotionally rewarding to most carers. Nonetheless, a rewarding experience that was unique to the hospice setting was the ability to have a one-on-one interaction with the patient, which gave the nursing staffs an experience of both job and emotional satisfaction. Furthermore, the reviewed studies revealed that various memory-making activities with the patients allowed the nurses to make a difference to the patients’ lives, and this was emotionally rewarding to them.
4.1.2 Teamwork
Being part of a team was found to be associated with the assistant nurses’ positive experience in the reviewed studies. Teamwork was depicted to produce good palliative care because through collaboration, the assistant nurses could deliver quality palliative care to the patient and their families, even in the lack of formal care training. The assistant nurses’ ability to provide psychosocial support to the patients was among the most rewarding experiences, as reported in the reviewed studies. These findings corroborate the results by Ahsberg & Carlsson (2014) that the role of assistant nurses in palliative care settings is not only to deliver practical palliative care but also to provide psychosocial care by engaging with the patients and discussing various existential issues they face.
4.1.3 Care Environment
Care environment also emerged as a significant factor influencing the experiences of assistant nurses in the palliative care setting. For instance, a positive care environment enabled the assistant nurses to apply the person-centred approach to care and to engage in supportive dialogue with the patients easily. Notably, several examples of positive care environment were reviewed, including sharing happy moments and taking photos with the families. These findings corroborate with the results by McCormack & McCance (2006) that a positive care environment plays an important role in the development and practice of person-centred care because, from a theoretical standpoint, the models of person-centred care can easily be achieved by matching the individual’s capabilities with their environment.
4.1.4 Community Nursing Experience
The reviewed literature was rich enough to compare the experience of nurses across the various end of life care settings based on qualitative data. The review literature showed a significant difference in the perceived quality of care delivered in community nursing setting (i.e. hospice) settings compared to other end of life care settings, with nurses from community nursing settings reporting highly favourable experiences of care compared to nurses providing end of life care in different settings such as the hospitals and cancer centres. Notably, relief of physical pain emerged to be the most highly regarded experience across the care settings, even though some nurses were not comfortable with the provision of spiritual and emotional care. Compared to other care settings, it emerged from the reviewed literature that community nursing setting provides the best experience with regards to the last week of life care because nurses could easily engage with patients at their final moments.
4.2 Negative Experiences
4.2.1 Symptom Management
The reviewed literature revealed that nurses faced a challenge with symptom management especially in the hospice setting where they had to cope with various end of life care situations, especially when handling children whereby they had to balance between providing end of life care and the children’s special needs. Similar results were found by Price et al. (2013) who concluded that in the hospice setting, nurses experience challenges of delivering care to children with complex care needs while also addressing their end of life care needs. However, it emerged from the current review that some paediatric palliative care settings have a supportive working environment that enables the nurses to mitigate most of the challenges. The present study findings generally corroborate with the results of earlier studies (e.g., Woolley et al. 1989) that the hospice setting provides the gold standard of a supportive environment required by nursing staff offering care to patients with end of life stage illness. A possible implication for these findings is that end of life stage patients are likely to experience quality care when nurses experience a supportive hospice environment (Maben et al. 2012 McConnell et al. 2016, Pearson, 2013). Hence, this study recommends that palliative community care nurses should receive both organizational and peer support to improve the quality of care they deliver.
4.2.2 Lack of Support
Findings from reviewed qualitative studies also indicate the negative experiences of nurses providing palliative care to patients with end of life stage illnesses with regards to lack of support from other practitioners. The lack of support means that they have to take extreme measures to provide care beyond their job descriptions, so that the individuals under their care can receive quality end of life care despite the physical constraints of residential care setting. According to Verderber & Refuerzo (2006), delivery of palliative care is akin to revalidation of an already invalid human being by providing holistic care and support ranging from emotional support to medical and spiritual care. Among the identified challenges include shifting the patient from hospital to residential care, especially when the patient lives in a geographically remote area in the absence of ambulatory care support. Furthermore, according to the reviewed evidence, the remoteness is associated with the patient’s inability to maintain personal hygiene, to keep off dangers like fire hazards, poor accessibility and consequently a reduced frequency of nurses’ visits. These findings corroborate with the results of Jacob (1961), who compared the delivery of palliative care in rural areas and cities and concluded that patients in city hospitals benefit from frequent visits, continuous monitoring by nurses, and a generally closer proximity to care providers, as opposed to patients from rural residential care facilities that have the comprehensive support from practitioners with various specialities. Nurses providing palliative care to patients with end of life stage illnesses in residential settings also experience challenges related to logistics and design of the residential environment. For instance, respondents on of the reviewed studies (i.e., Kaasalainen et al., 2014) indicated that they sometimes experience difficulty with navigating through the distant rooms with narrow corridors, which also pose as injury hazards to patients who live alone. Similar results were found by Evans (2005), who concluded that the architecture of some residential care facilities poses a danger to weak patients who are not able to navigate through the rooms, and this means that the nurses must constantly monitor even when they are off their formal duties. Furthermore, poorly designed residential care facilities pose a challenge to visiting nurses who have to move equipment around.
These findings indicate the underserviced nature of residential care facilities in rural areas compared to urban areas, and their impact on the quality of palliative care given to patients with end of life illness. Moreover, it depicts the lack of support from the construction authorities who are responsible for ensuring that the buildings are accommodative to all populations. Similar observations are made by Crooks et al. (2011) who asserted that although the delivery of palliative care among patients with end of life stage illnesses has received much attention nowadays, there is a lack of focus on the consequences of varying service availability and quality of care between rural and urban areas. A practical solution this variation is the creation of a palliative care hub where caregivers from both urban and rural regions collaborate through interdisciplinary teamwork to fill the care gaps experienced in rural areas. This would primarily harmonize any existing imbalance of care delivery between rural and urban care settings, and harness support from other specialities and departments to deliver quality care in community palliative settings. The reviewed literature also revealed lack of support as a negative experience by assistant nurses, especially when they were left alone with the patients. For instance, the assistant nurses sometimes have to assess the complex needs before figuring out when to call the ‘experts.’ The duty of assessing the patient’s complex needs is beyond their qualifications, meaning they conduct them under uncertainty. The literature also shows that the assistant nurses received suboptimal support from registered nurses, which is less than they expected. The assistant nurses expected that registered nurses would step in anytime the patient’s situation worsened or became complicated. Other studies have highlighted the experience of isolation and lack of professional collaboration among nurses and assistant nurses in palliative care settings. For instance, Fryer et al. (2016) & Philips et al. (2008) also found a lack of collaboration and coordination among assistant nurses and registered nurses, and this phenomenon hurt the patients’ well-being.
Emphasis is primarily put on teamwork between registered nurses and assistant nurses not only because it provides a supportive environment where every professional is working towards the single goal of improving the patient’s well-being, but also because it provides an opportunity for multi-professional learning. Furthermore, the essential nature of teamwork between registered nurses and assistant nurses in a palliative care setting is advocated for by many other studies including Finucane et al. (2013) & Fryer et al. (2016). However, a possible implication of these findings is that the structure of a consultant organization should be designed in a way that enhances and promotes inter-professional collaboration and teamwork.
4.2.3 Personal Involvement with the Dying Patients
The current literature review showed that the assistant nurses also experience complex and demanding situations when the patients shared stories of themselves because they felt a sense of pity after personally identified with the dying patient. Becoming emotionally and personally involved with the patient while providing psychosocial support made it difficult to maintain contact with the dying patient. These findings corroborate with the results by Beck et al. (2014), Udo et al. (2013), and Jakobsson et al. (2006) that complex situations in palliative care settings affect the professionals both existentially and emotionally, especially when they are handling patients with end of life stage illnesses. Besides, the review revealed that when such complex situations arise, patients and their families ask unplanned questions, which makes it difficult for the assistant nurse to determine when to engage the registered nurse. Reviewed literature also reviled insight into the end of life care for dementia patients and the experience of nurse professionals that create a barrier to the delivery of quality care. For instance, whereas better service coordination has mostly been emphasized as vital for the delivery of quality care end of life dementia patients (Department of Health 2001, Banerjee & Owen, 2009), reviewed literature show that professionals providing end of life care to dementia patients practice in environments of poor coordination and lack of knowledge of each other’s roles. Furthermore, the results show that some staffs involved in the care of such patients such as the ambulatory care nurses are perceived to be not part of the dementia care teams despite being frequently required at times of emergency. The home care nurses in the reviewed literature also reported difficulties with managing the unpredictable nature of dementia care needs as well as identifying the point at which the patient was entering the end of life-stage of dementia. As reported in some of the reviewed studies, such challenges made it difficult for nurses to decide the most appropriate care. Furthermore, the uncertainties made it difficult for the nurses to conduct an advanced care planning, despite several studies (e.g., Department of Health, 2008) advocating for the importance of advance care planning and its role in improving quality of care for patients with end of life stage illness.
4.2.4 Drop Back in Management
Nonetheless, other negative experiences associated with barriers to end of life care include a drop back in management, leading to inadequate resources and lack of time for the staffs to engage in essential care discussions, nurses’ inability to adhere to set care plans, and fear of close monitoring but regulatory authorities. The reviewed literature clearly revealed that some nurses felt a sense of futility and lack of confidence in caring for patients at the end of life stage and this hindered the self-drive and motivation to deliver quality care. Specifically, the lack of confidence was reported by nurses working in rural communities and care homes with frail patients. A possible implication of these findings is that nurse handling end of life stage patients require more management support through training and sensitization. This observation is supported by Banerjee & Owen (2009), who noted the efforts made by the UK’s National Dementia Strategy to advocate for education and training of dementia care nurses. Similarly, Scott & Pace (2009) argued that there needs to be on-going support for community nurses delivering both residential and home care to end of life stage dementia patients.
4.2.5 Rurality and Remoteness of Care Settings
The literature review also revealed a variety of challenging experiences related to the delivery of palliative care in rural areas, as well as how these challenging experiences act as barriers to delivery of quality care to end of life stage patients. Some of the prominent challenging experiences highlighted in the reviewed studies include conflict among healthcare workers, as well as challenges associated with working with the patient families. A possible implication of these findings is that the development of interventions to address the difficulties experienced by rural area nurses should be comprehensive enough to address both the staffs-related challenges and family-related challenges. Because families act as the primary caregivers for end of life stage patients, community nurses need to work in close collaboration with the families to optimize the care given to such patients. Similar conclusions were made by Novik & MacLean (2012) who observed that an effective communication between the patient, the nurses and the family caregivers is an essential element of quality care. Conversely, poor communication will harm the coordination of care, especially for those with a terminal illness.

Chapter 5
5.0 Conclusion and Recommendations
In conclusion, the findings of this study address the scarcity of knowledge on the experiences of palliative care nurses delivering care to patients with end of life stage illnesses in community settings. The study has explored the experiences and discussed them in two major themes of negative and positive experiences, whereby the positive experiences enhance the quality of care while the negative experiences act as barriers to delivery of quality care. The reviewed studies have highlighted the several roles of palliative care nurses and how the roles are affected or enhanced by negative or positive experiences, respectively. These findings are especially important because nurses, as well as assistant nurses delivering care to patients with end of life stage illness, have a role to play in caring for community-residing patients who are dying. Hence these results should be used as a source of information when making decisions regarding palliative care practices and strategies to support nurses working in the palliative care settings.
5.1 Strengths and Limitations
However, there are several limitations associated with this study that might affect the generalizability and application of its results. For instance, whereas all the reviewed pieces of literature were from primary sources, most of the findings were based on a small sample of populations; hence, their results could not be widely generalized. Moreover, being secondary research, the current study findings are subject to researcher bias inherent in the various primary studies reviewed. However, a significant strength of the present study is that it draws evidence from high-quality peer-reviewed journal articles to make conclusions on the experiences of palliative care nurses delivering care to patients with end of life stage illnesses at the community setting.
References
- Abarshi, E., Echteld, M., Van Den Block, L., Donker, G., Deliens, L. and Onwuteaka-Philipsen, B. (2010). Transitions between care settings at the end of life in the Netherlands: results from a nationwide study. Palliat Med, 24(2), pp.166–174.
- Apan, D., Quartaroli, T., & Riemer, F. (2012). Qualitative research: an introduction to methods and designs. San Francisco, Jossey-Bass.
- Bartholdson, C., Lützén, K., Blomgren K et al. (2015) Experiences of ethical issues when caring for children with cancer. Cancer Nurs;38:125–32.
- Baumeister, R. F. (2013). Writing a literature review. In M. J. Prinstein & M. D. Patterson (Eds.), The portable mentor: Expert guide to a successful career in psychology (pp. 119-132; 2nd ed.). New York: Springer Science+ Business Media.
- Banerjee S, & Owen J. (2009) Living well with dementia: A National Dementia Strategy.
- Cohen, J., Bilsen, J., Addington-hall, J., Löfmark, R., Miccinesi, G., Kaasa, S., et al. (2008) Population-based study of dying in hospital in six European countries. Palliat Med;22(6):702–710.
- Crooks, V., Schurrman, N., Cinnamon, J., Castleden, H., Johnston R. (2011) Refining a location analysis using a mixed methods approach: community readiness as a key factor in siting rural palliative care services. Journal of Mixed Methods Research; 5(1): 77-95.
- Department of Health (2001). National Service Framework for Older People. London:
- Ekstrã, M., Allingham, S., Eagar, K., Yates, P., Johnson, C. and Currow, D. (2016). Breathlessness during the last week of life in palliative care: an Australian prospective, longitudinal study. J Pain Symptom Manag, 51(5), pp.816–823.
- Etkind, S., Bone, A., Gomes, B., Lovell, N. and Higginson, I. (2017). How many people will need palliative care in 2040? Past trends, future projections and implications for services. BMC Med, 15(1), pp.E178–E187.
- Given, M. (2008). The Sage encyclopedia of qualitative research methods. Los Angeles, Calif, Sage Publications.
- Gisselle G. and Lotte Stig N. (2018) ‘Qualitative Methods in Pharmacy Research’, Pharmacy, Vol 6, Iss 3, p 79 (2018), (3), p. 79.
- Hendershot, A., Dixon, M., Kono, A., Dong, M. And Pentz, D. (2014) Patients’ perceptions of Complementary and Alternative Medicine in head and neck cancer: A qualitative, pilot study with clinical implications. Complementary Therapies in Clinical Practice. Vol.20, pp. 213-218.
- Hoffmann, T., Bennett, S., & Del Mar, C. (2009). Evidence-based practice across the health professions. Chatswood, N.S.W., Elsevier Australia.
- Korzeniewska-Eksterowicz, A., Przyslo, L., Grzelewski, T., Stolarska, M., Mlynarski, W., Stelmach, I., et al. Job satisfaction among health professionals of home hospice for children of Lodz region. Adv Pall Med. 2010;3:67–72.
- Jakobsson, E., Johnsson, T., Persson, L. O., & Gaston-Johansson, F. (2006). End-of- life in a Swedish population: Demographics, social conditions and characteristics of places of death. Scandinavian Journal of Caring Sciences, 20, 10–17.
- Korzeniewska-Eksterowicz, A., Przyslo, L., Grzelewski, T., Stolarska, M., Mlynarski, W., Stelmach, I., et al. (2010). Job satisfaction among health professionals of home hospice for children of Lodz region. Adv Pall Med;3:67–72.
- Novik, N., & MacLean, M. (2012). Pain and palliative care with seniors in Canada’s northern territories. In J. Kulig & A. Williams (Eds.), Health in Rural Canada (pp. 334-351). Toronto, ON: UBC Press.
- McConnell, T., Scott, D., Porter, S. (2016) Healthcare staff experience of providing end of life care to children: a mixed method review. Pall Med.
- McCloskey, S., and Taggart L. (2010). How much compassion have I left? An exploration of occupational stress among children‟s palliative care nurses. Int J Palliat Nurs;16:233–40.
- Maben, J., Peccei, R., Adams, M., Robert, G., Richardson, A., Murrells T., et al. (2012). Patients’ experiences of care and the influence of staff motivation, affect and wellbeing. Final Report. NIHR Service Delivery and Organisation Programme.
- Price, J., Jordan, J., Prior L. (2013). A consensus for change: parent and professional perspectives on care for children at the end-of-life. Issues Compr Pediatr Nurs;36:70–87.
- McConnell, T., Scott, D., Porter, S. (2016). Healthcare staff experience of providing end of life care to children: a mixed method review. Pall Med.
- Pearson N. (2013). “You’ve only got one chance to get it right”: children’s cancer nurses’ experiences of providing palliative care in the acute hospital setting. Issues Compr Pediatr Nurs;36:188–211. doi: 10.3109/01460862.2013.797520.
- Plante, J. and Claude D. (2011) Health care professionals’ grief after the death of a child. Paediatr Child Health;16:213–6.
- Scott S, & Pace V. (2009) The first 50 patients: a brief report on the initial fi ndings from the Palliative Care in Dementia Project. Dementia;8:435–41.
- Teno, E., Gozalo, P., Leland, N., Miller, S., Morden, N. and et al (2013). Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA, 315(3), pp.272–283.
- Verderber S., & Refuerzo B. (2006). Innovations in hospice architecture. Abingdon, Oxon: Taylor & Francis Group.
- William L. (2014). Non-palliative care staff need to deliver generalist end of life care. BMJ;348:3426.
- Woolley, H., Stein, A., Forrest, C., et al. (1989). Staff stress and job satisfaction at a children’s hospice. Arch Dis Child;64:114–8.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



