Improving Patient Safety with SBAR
Introduction of HBPM
1.1 Brief Introduction
Blood pressure is defined as the force required by the blood to flow through the arteries in the human body. When a heart beats, blood is pushed through the arteries and is carried from the heart to the rest of the body. The blood pressure can also be defined as the pressure put on the artery walls as the blood is flowing (England Public Health, 2017). High blood pressure (also known as hypertension) occurs when blood flows through the arteries at a higher pressure than normal (Slark, et al., 2014). There are many causes of hypertension; such as an individual’s diet, lifestyle, medication, age and genetics. If an individual’s high blood pressure gets too high and remains high for a long time, it can lead to many health complications. Individuals are put at a high risk for stroke, heart attack, heart disease and kidney failure (England Public Health, 2017). Blood pressure is measured in mmHg (millimetres of mercury) and is normally recorded as two numbers, where one is written above the other. The top number is referred to as the systolic blood pressure (the highest pressure in the blood vessels), whereas the bottom number is referred to as the diastolic blood pressure (the lowest pressure in blood vessels) (England Public Health, 2017). The National Institute for Health and Care Excellence (NICE) defines high blood pressure as a clinic blood pressure of 140/90 mmHg or higher and as either the home blood pressure average or the succeeding ambulatory blood pressure monitoring daytime average of 135/85 mmHg or higher (England Public Health, 2017). It is estimated that over 2.1 million people below the age of 45 had high blood pressure in England in 2015.

1.2 Problem Statement
One of the ways to improve the detection and management of blood pressure is through self-monitoring. Research has shown that self-monitoring of blood pressure is associated with reasonable reductions in both the systolic and diastolic blood pressure (England Public Health, 2017). Studies have shown that a large number of the home blood pressure monitoring devices were inaccurate. Also, that patients didn’t have the techniques required to use them. Thus, this study aims to examine the accuracy and reliability of home blood pressure monitoring for patients with hypertension.
1.3 Objectives
The research seeks to achieve the following objectives:
To determine the use and reliability of home blood pressure monitoring
To evaluate the challenges associated with the self- monitoring device and its relationship with the self- monitoring patient
CHAPTER 2
Literature Review
2.1 Background of HBPM
Historically, ambulatory blood pressure monitoring (ABPM) has been considered the gold standard for the diagnostic confirmation of resistant hypertension (RH). However, home blood pressure monitoring (HBPM) has now become an option for many patients because of aspects such as lower costs and the comfort the patients get from doing it in their own homes (Marui, et al., 2010). ABPM was established before HBPM and it requires little effort from the patient. The only requirement is for the patient should to try not to disturb the measurement. Even though ABPM is the gold standard for assessing whether a patient needs to be put on antihypertensive management, when it comes to monitoring the time-course of any response to the treatment given it is less feasible (Hodgkinson, et al., 2011). The most common preventable cause of cardiovascular (CV) disease is hypertension. It increases the chances of an individual having a stroke, heart attack, kidney disease and heart failure (George & MacDonald, 2015). HBPM is a system that is usually incorporated into the treatment recommended for patients with hypertension. Studies have shown that office-based monitoring has less benefits as compared to HBPM. Patients who used Oscillometric BP devices at home as opposed to assessment by mercury sphygmomanometer benefited a lot. To begin with, there was an overall reduction in the white coat and masked effect in analysis and management of hypertension. Second, the overall BP load, which is obtained by the BP readings taken at different times of the day, is improved in accuracy. Lastly, since the patient is involved in the management of their high blood pressure, there is an increased devotion to ensuring that they effectively manage their hypertension (George & MacDonald, 2015). HBPM also allows for detection of BP variability, this again enables the patient to understand their hypertension management better and the tele monitoring aspect allows healthcare professional to remotely monitor their patients BP (Hodgkinson, et al., 2011). Table 1 summaries some of the advantages and limitations of HBPM. In both primary care settings and clinical trials, it has been found that there are significant discrepancies in office BP readings (Sebo, et al., 2014). Furthermore, when predicting long-term CV outcomes, office-based BP measurements are inferior to the blood pressures measured using the HBPM system (Cohen & Cohen, 2017).
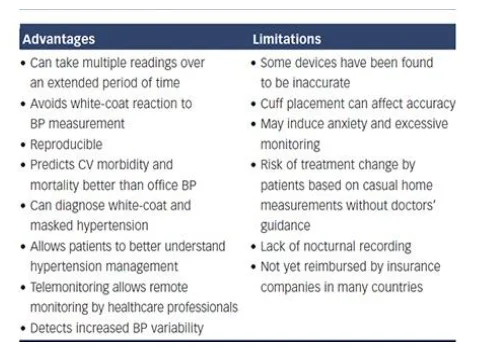
There are some limitations attributed to the HBPM, when it comes to the management of certain diseases. In patients with chronic kidney disease (CKD), when predicting the progression to end stage renal disease or death, it was found that HBPM outperformed the office-based BP monitoring (Sanghavi & Vassalotti, 2014). In addition, when the HBPM results are combined with additional support such as medication titration or behavioural therapy and tele monitoring, there is an overall improvement in the BP control (Sanghavi & Vassalotti, 2014). Nonetheless, nocturnal readings cannot be obtained from HBPM, thus information on diurnal patterns in BP cannot be observed, and these tend to be more widespread in the CKD population and are also important when assessing the CV risk factors (Sanghavi & Vassalotti, 2014). Another limitation associated with HBPM is the accuracy of devices. A study was carried out in 2009 to determine the accuracy of 554 automated HBPM devices. It was found that only 30% of the devices were accurate while the other 70% of the automated machines were inaccurate. Also, the frequency of accuracy was observed to be higher in validated devices as compared to non-validated devices (Akpolat, et al., 2009). A study conducted in 2012, showed that 30% of the 382 devices studied had been acceptably validated and only 24% of the devices were inaccurate. Moreover, it was found that wrist devices were less accurate as compared to upper hand devices (Akpolat, et al., 2011). A feature that is essential to the HBPM monitors is the link observed between upper arm circumference and cuff size. It has been observed that inappropriate cuff size can lead to inaccuracy in the recordings; researchers have suggested that depending on patient (child, adult or obese) different cuffs should be used to measure the BP (Bur, et al., 2003). As earlier stated, 70% of the readings from HBPM devices are undesirably inaccurate. Inaccuracy of the results from these devices may cause serious implications to people, especially those who rely on these readings in the making of informed significant health decisions. Most of these devices have been found to be inaccurate within 5 mmHg; these devices, according to Ringrose et al (2017), were off the right mark by 10 mmHg or more around 30% of the time. In a certain case, 30% of 210 clinic patients recorded a 5 mmHg difference in systolic pressure, comparing the HBPM device and the standard office reference (Pendick, 2019). Depending on the accuracy threshold, 5-15% of patients record inaccurate measurements in their HBPM devices. The accuracy of these HBPM devices is an important factor basically because both over- and under- treatment of hypertension may have adverse consequences ranging from symptomatic hypotension, hypo perfusion, fall- related injuries to hypertension, heart failure, myocardial infarction and left ventricular hypertrophy. There should be 80-100% coverage of the patients arm circumference by the inflatable bladder of the cuff. Observations made showed that the use of cuffs which were too small led to the overestimation of the BP, while a large cuff caused an underestimation of the BP (Bur, et al., 2003). Even though the use of standard cuffs are appropriate for majority of patients, it is recommended that those with small (<24 cm) or large (>32 cm) arm circumference only the devices that is equipped with that particular sized cuffs should be used (Bur, et al., 2003).
The UK has a lot of options when it comes to HBPM current devices. Monitoring an individual’s blood pressure regularly is an important way in which the individual may prevent health conditions; these include heart related diseases or attacks. Some of the most used devices include the Omron M7 Intelli IT Upper Arm Blood Pressure Monitor, which is an innovated monitor with extended functionality, large black lit display and enables use for several people; the Duronic BPM150 Upper Arm Blood Pressure monitor is another which is easy to store and comfortably used universally. There are other common HBPM devices such as the Braun iCheck 7 Wrist Blood Pressure Monitor, Omron M3 Comfort Upper Arm monitor and the Omron M2 basic Upper Arm monitor.
2.2 Intervention
For accurate measurements of the BP, the individual must ensure that the cuff is wrapped around the arm correctly and that the individual should have proper posture during the measurement. Inexperienced users may find it difficult to wrap the cuff in the correct position, thus leading to inaccurate results. Additionally, patients that exhibit arrhythmias (irregular pulses) will have inaccurate results. Advancements in technology have ensured that home monitoring devices are equipped with automated cuff wrapping and a display that indicates where the correct position of the cuff should be (Takahashi, et al., 2015). These types of devices are equipped with systems that can detect irregular pulses that can lead to inaccurate BP readings. Furthermore, they detect noises and wave pulses within the cuff that are caused by arm movements thus leading to more accurate results (Takahashi, et al., 2015). The Intelli wrap cuff technology is the newest development in the HBPM technology. It has a longer inflatable area within the cuff that wraps enables the patient to wrap it all the way round their arm. Therefore reducing the pressure lost on the brachial artery, while increasing the ‘acceptable range’ of placement and thus reducing the impact of cuff placement on accuracy (see Figure 1). It can be easily fitted with one due to its pre-formed, feature (George & MacDonald, 2015).

A study evaluated the Omron M6-Comfort; HEM-7321-E (which is a validated oscillometric device) fixed with the Intelli wrap cuff in subjects (planned n=50) aged 50.7 ± 16.0 years who had an arm circumference 33.3 ± 4.4cm, body mass index of 32.8 ± 7.9 kg/m2 and in stable clinical condition. Results from the data showed that incorrect positioning of a conventional cuff significantly affects BP measurement results. The greatest overestimation of BP was observed when the bladder centre is displaced by an angle of 90° laterally or by an angle of 180° compared (Bilo, et al., 2017). However, when the Intelli Wrap cuff was used, there was no substantial outcome caused by the particular cuff position. When using the oscillometric device the BP values obtained were lower as compared to those obtained by reference method. This was attributed to undercuffing that resulted from the mercury device equipped with standard size cuff in patients who had a large arm circumference (Bilo, et al., 2017).
2.3 Change
Studies show that patients generally view HBPM as a positive strategy and tend to be more motivated, empowered, and assured (Rickerby, 2002). Models such as Social Learning Theory (Bandura, 1986), the Health Belief Model (Clark, et al., 1992) and Theory of Planned Behaviour (Ajzen, 2011), identify the significance of the factors and processes that predict and prompt behaviour change. It is observed that diverse precursors to behaviour adoption, change, and maintenance can be attributed to the different theoretical views. In a study conducted by Cacioppo & Rogers (1983), it observed that patients readily adopted HBPM because of the consequences of hypertension. The HBPM enabled them to take more control of their BP management, thus mitigating the consequences of hypertension. HBPM provides various readings in the everyday environment of an individual. Through this, it is possible to detect the immediate phenotypes of hypertension; masked hypertension and white coat. Compared to the conventional and standard office BP measurements, HBPM seems to have superior prognostic values (Stergiou et al, 2018). In addition, HBPM enables control of hypertension rates on a long term basis. Furthermore, HBPM provides a forum that is widely available, acceptable and relatively inexpensive to many patients. In the United States, Europe, Japan and many other countries, various guidelines for the management of hypertension the use of the 24- hour ambulatory BP monitoring (ABPM), as well as the self- monitoring by patients at their homes, is an essential way in which patients may be able to manage and confirm hypertension on a long term basis (Parati et al, 2010; Whelton et al, 2018). There is a misconception that HBPM is performed to aid in the delay of seeking treatment from healthcare providers. Therefore, it has been noted that there are problems when it comes to transferring data obtained from HBPM to healthcare providers (Grant, et al., 2015). A Canadian study of older adults should evidence of falsified reassurance, heart attacks or strokes could prevented by simply using the HBPM (Viverais-Dresler & Baker, 2004). Moreover, current studies suggest that patients don’t necessary understand the benefits of HBPM (Grant, et al., 2015).
2.4 Diffusion of innovation theory
This is a classical theory of change. Classical theories of change are sometimes referred to as normative or descriptive theories. Most of these theories simply explain or describe the natural process by which change occurs. The most prominent theory that can be illustrated is the Diffusion of innovation theory (Rogers, 1983). There are five major stages in which Rogers explains the innovation decision process. First, people are made aware of the innovation or change; second, through leadership and advocacy or agent change, people are persuaded towards the change (this basically entails development of positive attitudes toward innovation); third, people decide whether or not they accept the change. After acceptance, implementation is done. The last stage involves confirmation; this basically means that people decide on whether or not the change is beneficial or sustainable; they decide on whether they continue with the change or abandon the change (McDonald et al, 2004).
CHAPTER 3
Design
3.1 Method
This report ultimately adopts a quantitative method of research. Quantitative research from reliable study sources is substantially disseminated in the report and analysed to give a practical understanding of HBPM devices, their use and efficiency. In addition, this study report also analyses other reports, health guidelines and procedural provisions regarding HBPM. In a bid to evaluate the impact of HBPM, the report also presents statistical data on the use and practices related to the self- monitoring devices, among other elements affecting the devices. It is necessary to adopt a quantitative research method because this type of research enables the analysis of statistical data gathered from various reliable sources, which is primarily how the impact of this intervention may be acknowledged.
3.2 Prevalence of HBPM
According to Baral- Grant et al (2011), the primary care survey conducted aimed to determine the prevalence of HBPM devices amongst individuals with hypertension. 31% of 955 people in the UK reported to self-monitor their blood pressure at home. The survey targeted 1815 patients with hypertension in the West Midlands, and registered with four general practices. 955 surveys were analysable and the data collected from these results were used in the assessment of HBPM prevalence in the UK. A current analysis depicted 293 participants self- monitoring their blood pressure (CI 27.8-33.7% and crude prevalence 30.7%). 24.1% of the participants from various parts of the UK had concurrent diabetes. From this number, 32.6% monitored blood pressure while 67.4% monitored blood sugar levels. The characteristics presented in this primary study also showed that younger people were more likely to measure their own blood pressure compared to older people (young= aged between 18-60; older years= above 60). From the prevalence it can be deduced that the 70% inaccuracy results presented by various studies may lead to a number of misinformed consequences.
3.3 Inaccuracy of HBPM devices
Statistical data collection was based on a few UK- based study reports. Vasileiou et al (2013) conducted a qualitative study which included participants from various areas in England. Data analysed from the study was thematically analysed. The participants’ and devices’ characteristics were presented as below:
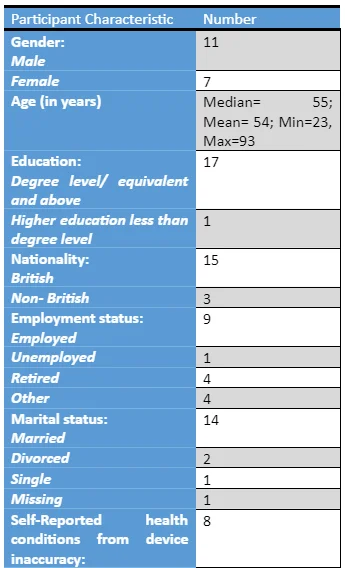
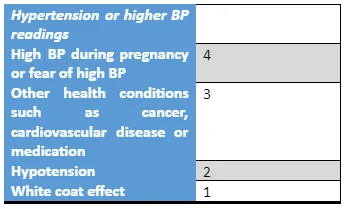
In addition to the inaccuracies in readings by these monitors, Hodgkinson et al (2016) also associated the precision of these readings with the time in service from data collected with the UK, shown below:
The limiting factor associated with HBPM remains to be the accuracy of the devices. A study to determine accuracy in 2009 found only 30% of 554 automated HBPM devices had acceptable validation accuracies, whereas 72% were generally inaccurate (George & MacDonald, 2015). While comparing validated devices and non- validated devices, the frequency of accuracy was lower in non- validated devices. 24% of the devices in 2011 were inaccurate in a study including a total of 382 devices; only 30% of them were acceptably validated. Recent review on data from 210 patients displayed the presented results (Figure 3-1 below); these patients attending hypertension clinics recorded differences in readings; 30% of the HBPM readings displayed differences of more than 5 mmHg, while 8% recorded more than 10 mmHg difference in readings from mercury systolic BP measurements taken from the office clinic.
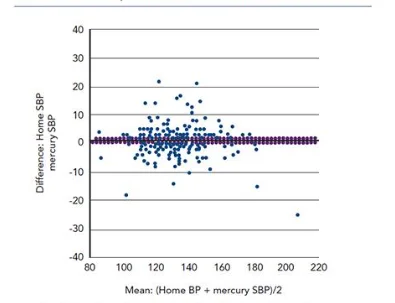
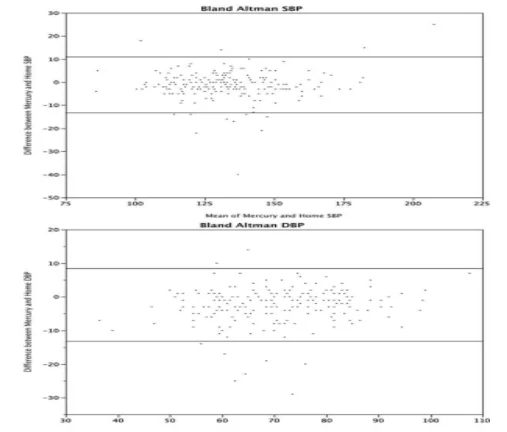
Regardless of the different sets of inaccuracy thresholds, Ruzicka et al (2016) also show that there is inaccuracy when the blood pressure measurements are compared between HBPM devices and the mercury sphygmomanometer. They presented their findings from the Bland- Altman analysis which depicted difference in BP values spread across the entire BP range, showing no trend in inaccuracy with both decreasing and increasing BP. The figure below shows this inaccuracy:
From a positive angle, according to George & MacDonald (2015), most prospective studies have found that HBPM more accurately predicts Stroke and Cardiovascular mortality and morbidity compared to the standard office BP measurements (See appendix I).
CHAPTER 4
Analysis and Conclusion
4.1 Critical Review
Stergiou et al (2018) strongly suggests that HBPM presents a much more superior predictive measurements compared to the office BP monitoring. HBPM is widely accepted by patients in different countries and with different conditions; it is also widely available in many countries. In optimal diagnosis and effective management of hypertensive individuals, it is essential to receive accurate measurements of BP (Stergiou & Bliziotis, 2011). In comparison to the conventional office BP measurements, HBPM enables patient convenience, the detection of masked phenomena and white coat, enhancement of therapeutic compliance and adherence, and superior risk prediction (McManus et al, 2010). HBPM is also strongly endorsed in hypertensive patients by hypertension guidelines. The oscillometric technique is the primary way in which HBPM devices measure BP; an algorithm applied to the envelope of oscillometric wavelengths estimates the BP which is generated in the course of cuff inflation and deflation (Alpert et al, 2014). HBPM is becoming increasingly popular in the UK; the conceptual understanding behind this is, however, little. According to Grant et al (2015), there are three main themes that arise from the psychological processes or factors that result into self-monitoring: Self-medication and behaviour, describing views on self-monitoring, medication adherence and current practice; professional health care provider to patient transaction; and emotional element of living with an asymptomatic condition. While some people engaged in self-monitoring out of curiosity, others who self-monitored used it as a protective and preventive tool against fears of silent but serious conditions. Most of the self- monitoring devices are sold formal validation of accuracy. Furthermore, it is difficult to ascertain whether the study results are generalizable to individual patients even when the monitors are considered valid to contemporary standards (Akpolat et al, 2011). The accuracy of oscillometry is thought to be detrimentally affected by predisposing factors arising from certain characteristics such as widened pulse pressure and arterial stiffness. The general accuracy of self- monitoring devices is never a verified aspect in HBPM and as a result, across all studies, this has been identified as a key limitation in terms of current validation standards (Babbs, 2012). Similar to this issue, various studies have purposed to show the inaccuracy of HBPM devices (Ruzicka et al, 2016; Akpolat, 2009; Dilek et al, 2008). However, according to Ruzicka et al (2016), the differences in what is considered inaccurate in different studies arises due to the differences in the methodologies used; number and type of observers assessing the accuracy limit, threshold used to determine inaccuracy and the monitors assessed. In the study conducted by Ruzicka & Hiremath (2017), 7%, 29% and 69% recorded more than 15, 10 and 5 mmHg respectively difference in measurement taken between the patient’s own automated oscillometric home BP device and the auscultatory reference standard (mercury sphygmomanometer); these were recordings of the diastolic or systolic BP taken simultaneously with a 2- observer auscultatory reference standard BP measurement.
4.2 Agent Change
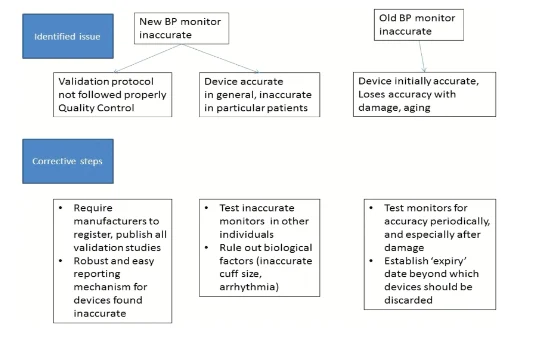
The BI report in methodology design presenting the prevalence, use and accuracy of HBPM devices significantly emphasizes the clinical impact of HBPM in the modern society. Given that various major national organizations (Such as the American Society of Hypertension, Hypertension Canada and NICE) guidelines on the management and diagnosis of hypertension endorse HBPM, the data compiled and depicted creates a major concern. In the same manner, data recorded from these self- monitoring devices play significant roles in making informed decisions for the control and management of hypertension. In addition to this, the market trends depict dramatic expansions of these devices over the last decade (Ruzicka & Hiremath, 2017). Although there are prescriptive measures and standards for validation of HBPM, there is insufficient evidence that proves that these rigorous standards are actually met. For instance, upon a certain review, only 21% of published validation studies complied with the protocols in place regarding examination of validated ABP devices (Hodgkinson et al, 2013). There are several reasons provided by Ruzicka & Hiremath (2017) for this failure of compliance (Shown in the figure 4-1)
A wide range of devices are increasingly offered by medical technology for use at homes. This report essentially emphasises the role of individual responsibility and autonomy. Through such findings, the uncertainties and complexities that characterize the interpretations of home readings are illustrated (Vasileiou et al, 2013). It is clear that greater clinical involvement could aid in the acquisition of accurate and more helpful measurements of BP. Moreover, self- monitoring practices also improves communication between the professional health care giver and the patient.
4.3 Service improvement
With reference to the ABPM, several cross- sectional studies have been undertaken to investigate the diagnostic performance of HBPM. There is considerable agreement in these investigations between the two; HBPM and ABPM; despite the heterogeneity in their designs. Specificity and sensitivity values range from 60-90% depending on the study design used (Stergiou & Bliziotis, 2011; Hodgkinson et al, 2011). In regards to limitations from various clinical studies, there are things that should be reconsidered to enhance efficiency in primary care and clinical settings. First, there are several models of self- monitoring devices, the validation statuses of each and every one of these models may be difficult to report on (Ruzicka et al, 2016). Interpretation of the results from this report should also be cautioned; in that in as much as the results are provocative and applicable in practice, they are obtained from retrospective analyses of various reports and articles. As a concern for further study, it is also crucial to look at the inaccuracy of the results produced by an individual HBPM among different individual patients. Various issues may still arise from the concept of inaccuracy of these HBPM, however, moving forward, for the ongoing review of HBPM, the National Institute for Health Research and the British Hypertension Society has a few significant recommendations. First, it is important to maintain and calibrate these HBPM devices in line with the manufacturers’ instructions. In addition, patients should bring their self- monitoring devices for check-ups so that the appropriate health care practitioner may confirm that the device is being used in the right way, the correct sized cuff is being used and that the device is indeed valid. Ruzicka et al (2016) bring out the significant gap associated with HBPM processes that needs to be investigated further and addressed so that the concept of sustainability may be met. Re- validation in regards to the accuracy and safety of these devices is crucial as a first step. Furthermore, the methods and procedures for validation in place are difficult to implement, essentially due to their time- consuming nature and technicality in routine clinical care settings.

4.4 Sustainability
Across most studies, there was a similar finding in the rate of clinically relevant inaccuracy in certified and non- certified devices. The methodologies of various studies finding this primary limitation of HBPM devices a major concern can be deemed to be highly appropriate and as a result, a number of issues arise (Ruzicka & Hiremath, 2017). This can be deemed as the primary potential barrier to the intervention. For sustainability, it is necessary to understand the concept behind this major barrier. The first issue is whether the certification and validation process actually incorporates assessment of the device’s accuracy. On affirmation, is this process of validation and assessment independent and rigorous? There is one major characteristic which affects this process; HBP monitors differ depending on their respective physical components and electronic algorithms. Consequently, there are various protocols and standards that have been developed in relation to validation of respective devices. Examples of these standards include the British Hypertension Society in 1990 and the European Society of Hypertension (ESH) in 2002. In 2010, the ESH developed simplified procedures for validation of these devices. The standards set in these various regulations are indeed exhaustive, prescriptive and rigorous in a way which includes the criteria for accuracy assessment (Ruzicka & Hiremath, 2017). Appendix II shows some of these salient features that can be seen from the American Medical Instrumentation (AAMI), the British Hypertension Society (BHS) and the European Society for Hypertension (ESH). The second issue is whether the source of error actually originates from the quality control issues in individual devices; this is despite the validation and certification process. The HBPM may be accurate enough for the population, but still fails to produce accurate results when it comes to the individual. As a matter of fact, Ruzicka & Hiremath (2017), state that the individual devices algorithms from diastolic and systolic BPs may suit more or less the individual user and may also vary from one brand to another. The third and final issue according to Ruzicka & Hiremath (2017) is decrease in accuracy of these kinds of devices with the time of usage. Erroneous measurements may be recorded when the mechanical components of the device undergo damage, probably due to wear and tear, this may happen even though the algorithm itself is programmed not to change with time. This may however not be an independent predictor of accuracy (Ringrose et al, 2017).
4.5 Conclusion
In more often than not situations, the decision to HBPM appears to be an individual choice (Grant et al, 2015). The results from such practice, undoubtedly, can be utilized by both parties to make informed health care decisions. Across various studies, it is clear that HBPM improves the accuracy of hypertension diagnosis and effective management of the same. However, the main limitation brought out from various reports remains to offset this overall benefit from HBPM (Ruzicka et al, 2016). There can be serious and adverse impacts in the management of hypertension arising from the magnitude of this inaccuracy. The detection and awareness of this problem is therefore warranted in the continued use of HBPM. HBPM, just like ABPM, provides various BP measurements in the usual environments of the respective individuals, away from the office and artificial setting; this allows for a much more representative and accurate assessment than the office BP measurement. Although self- monitoring is not as prevalent in the UK, compared to the statistics at an international level, this concept is practised by a significant number of people, warranting its greater integration into clinical practice (Baral- Grant et al, 2011).
REFERENCES
- Akpolat, T., 2009. Proposal of a method for the evaluation of inaccuracy of home sphygmomanometers. Blood Press Monit; 14 (5)
- Akpolat, T., Aydogdu, T., Erdem, E. & Karatas, A., 2011. Inaccuarcy of Home Sphygmomanometers: A Perspective From Clinical Practice. Blood Press Monit , 16(4), pp. 168-171.
- Alpert, B., Quinn, D., Gallick, D., 2014. Oscillometric blood pressure: a review for clinicians. J Am Soc Hypertens; 8, pp. 930-938
- Baral- Grant, S., Haque, M., Nouwen, A., Greenfield, M., McManus, R., 2011. Self- Monitoring of Blood Pressure in Hypertension: A UK Primary Care Survey. International Journal of Hypertension
- Bloch, M. and Basile, J. (2008). Analysis of Recent Papers in Hypertension, Jan Basile, MD, Senior Editor. The Journal of Clinical Hypertension, 9(4), pp.297-301.
- Cohen, J. B. & Cohen, L. D., 2017. Intergrating Out-Of-Office Blood Pressure in the Diagnosis and Management of Hypertension. Curr Cardiol Rep, 18(11), p. 112.
- George, J. & MacDonald, T., 2015. Home Blood Pressure Monitoring. European Cariology Review, 10(2), pp. 95-101.
- Grant, S., Greenfield, M. S., Nouwen, A. & McManus, J. R., 2015. Improving management and effectiveness of home blood pressure monitoring a qualitative UK primary care study. British Journal of General Practice, 65(640), pp. 776-783.
- Hodgkinson, J., Mant, J., Martin, U., 2011. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension; systematic review. BMJ, p. 342.
- Hodgkinson, J., Sheppard, J., Henghan, C., Martin, U., Mant, J., Roberts, N., McManus, R., 2013. Accuracy of ambulatory blood pressure monitors: a systematic review of validation studies. J Hypertens; 31, pp. 239-250
- Kallioinen, N., Hill, A., Horswill, M., Ward, H., Watson, M., 2016. Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings: a systematic review. Journal of Hypertension, 35 (3), pp. 421-441
- McDonald, K., Graham, I., Grimshaw., 2004. Closing the Quality gap: A critical analysis of quality improvement strategies. Agency for Healthcare Research and Quality
- McManus, R., Mant, J., Bray, E., Holder, R., Jones, M., Greenfield, S., Kaambwa, B., Banting, M., Bryan, S., Little, P., Williams, B., Hobbs, F., 2010. Telemonitoring and self- management in the control of hypertension (TASMINH2): a randomized controlled trial. Lancet; 376, pp. 163-172
- Rickerby, J., 2002. The role of home blood pressure measurement in managing hypertension: an evidence-based review. J Hum Hypertens, 16(7), pp. 469-472.
- Ringrose, J., Polley, G., McLean, D., Thompson, A., Morales, F., Padwal, R., 2017. An assessment of the Accuracy of Home Blood Pressure Monitors When Used in Device Owners. American Journal of Hypertension, 30 (7), pp. 683-689
- Ruzicka, M., Hiremath, S., 2017. Accuracy- Limiting factor for Home Blood Pressure Monitors? American Journal of Hypertension; 30 (7), pp. 661-664
- Sanghavi, S. & Vassalotti, J. A., 2014. Practical use of home blood pressure monitoring in chronic kidney disease. Cardiooenal Med, Volume 4, pp. 113-122.
- Takahashi, H., Yoshika, M. & Yokoi, T., 2015. Validation of two automatic devices for the self-measurement of blood pressure according to the ANIS/AAMI/ISO81060-2:2000 guidlines:the Omron BP765 (HEM-7311-ZSA) and yje Omron BP760N (HEM- 7320-Z). Vasc Health Risk Manag, Volume 11, pp. 49-53.
- Whelton, P., Carey, R., Aronow, W., 2018. Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a Report of the American College of Cardiology/ American Heart Association Task Force on Clinical Practice Guidelines. Hypertension, 71
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



