CT Scans and Subarachnoid Hemorrhage Diagnosis
INTRODUCTION
When a patient visits any medical facility following a sudden onset of headache or a ‘thunderclap headache, a computed tomography (CT) brain scan will inevitably be conducted as part of the diagnosis of the underlying problem (Martin et al., 2013). A CT brain scan done in the first 12 hours of sudden headache corroborates the diagnosis of subarachnoid hemorrhage (SAH) in 98% of the patients. After 12 hours the sensitivity of the scan is reduced to approximately 90% because the blood undergoes gradual dilution by the constant movement of the CSF (Marcolini & Hine, 2019). Within 3 days, the sensitivity goes down to 80% and 50% after a week. This shows that some of the patients experiencing sudden headaches but with normal CT brain scans could still have had a SAH, especially if there was a delay before the scanning (Williams, 2004). Failure to spot an aneurysmal SAH is life-threatening especially in cases where there is recurrent bleeding. To combat the risk of bleeding out, surgery is done to clip the aneurysm (Goyale et al., 2016).
At the Milton Keynes University Hospital NHS Foundation Trust, patient satisfaction is always prioritized and medical services are offered round the clock. Currently, in accordance with the UKNEQAS (United Kingdom National External Quality Assessment Service) guidelines, laboratory facility offers CSF xanthochromia screening using the gold standard method of bilirubin detection with spectrophotometric scanning (wavelength of 350 nm to 600 nm). This procedure is done between 0900 hours to 1900 hours during the weekdays, i.e. Monday to Friday and 0900 hours to 1200 hours during the weekends. However, there is a delay when it comes to discharging of patients particularly those who are suspected to have SAH. Medical procedures like CT scanning have to be done to diagnose the condition. This is followed by lumbar puncturing if the CT scanning does not provide satisfactory results and SAH is highly suspected. Processing of the CSF samples is usually pushed to the end of the day or the following day in order to attend to emergency cases. This leads to a delay in the production of CSF xanthochromia results and therefore delayed discharge of the patient.
LITERATURE REVIEW
Lumbar puncturing is a medical procedure used to diagnose for SAH especially in cases where the CT scan turned out negative and SAH is highly suspected. This method entails the insertion of a needle at the lower back (Lumbar region) between two vertebrae in order to collect cerebral spinal fluid (O’Glasser & Mansoor, 2015). Up to four tubes of 3 mL of the CSF samples are collected to examine CSF Xanthochromia (Koenig, 2008). Xanthochromia is a Greek word that was coined to mean “Yellow Color” which originates from bilirubin (Williams, 2004). This yellow color in the Cerebral Spinal Fluid (CSF) can be detected in patients experiencing a sudden onset of headaches, jaundice, carotene addiction or those with elevated levels of CSF proteins. If the lumbar puncture results are positive, patients are admitted for a minimum of 2 days, before discharge, to monitor for an aneurysm so that it can be treated on time (Brinjikji & Lazino, 2018).
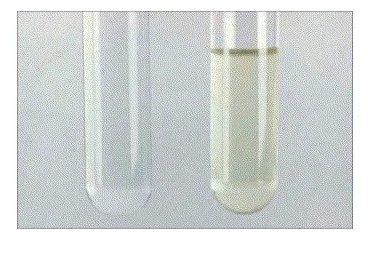
Xanthochromia of the CSF occurs within 6 to 12 hours after subarachnoid hemorrhage (SAH) due to the production of bilirubin (Dugas & Bollu, 2019). To determine CSF xanthochromia, approximately 3 milliliters of the fourth tube of the collected sample undergoes centrifugation at 2000 rpm for five minutes. The fourth tube is used as the first three tubes might contain contamination of red blood cells due to a traumatic tap. The centrifuged sample is then placed in a clear glass tube alongside the same amount of water. The two are then inspected visually against a plain white background in natural lighting. A normal CSF is as colorless as the water but in the case of xanthochromia, the fluid is tainted yellow, bloody or cloudy (Koenig 2008) as shown in figure 1. It is not clear whether the entire process is adhered to, therefore inspection with the naked eye can produce an inaccurate conclusion (Martin et al., 2013)

Another method of determining xanthochromia, apart from visual inspection, is spectrophotometry (Dugas & Bollu, 2019). The use of the spectrophotometer is a more reliable method as it can analyze whether the xanthochromia is due to CSF bilirubin or oxyhemoglobin. A traumatic lumbar puncture causes the introduction of red blood cells into the CSF leading to oxyhemoglobin which is not transformed into bilirubin once sample collection has been done (Goyale et al., 2016). Oxyhemoglobin can be detected in the cerebral spinal fluid between four to ten hours. There are many studies that support detection of bilirubin at six hours after a major hemorrhage. After 3 to 4 days, the xanthochromia can still be detected in the CSF as the heme has now been fully converted into bilirubin. Therefore, the detection of bilirubin in CSF by a spectrophotometer is a distinguishing diagnosis for true subarachnoid blood than oxyhemoglobin (Williams, 2004) as shown in figure 2. This minimizes the chances of a false positive conclusion caused by a traumatic tap.
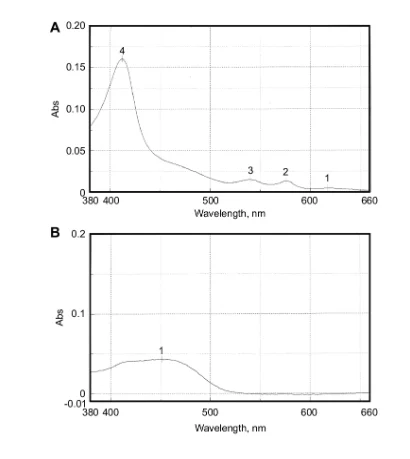
From figure 2, curve A indicates the absorption spectrum of a mixture of oxyhemoglobin at point 4 is 416 nm (greater than 0.15 AU) and bilirubin at point 3 is 540 nm (at 0.020 AU) while curve B displays the absorption spectrum of a normal CSF sample at 450 nm which is 0.048 AU.
A normal cerebral spinal fluid sample is as colorless as water and have a relatively levelled and consistent absorption spectrum under a spectrophotometer (Zhao & Wei, 2017). A medical laboratory technologist should be keen to distinguish even the minute differences in the wavelength produced by the various samples for accurate diagnosis (Nebeker et al., 2020) In the US, a simple visual inspection of CSF xanthochromia is widely utilized, while in the UK spectrophotometry is the adopted method for the detection of CSF xanthochromia (Koenig, 2008).
Williams, (2004) concluded that an incorrect diagnosis of CSF xanthochromia may occur if an analysis of the samples is done too soon after subarachnoid hemorrhage. Pigments from RBCs are produced within the first two hours subsequent to the hemorrhage. In order to ascertain the non-appearance of xanthochromia, CSF sample collection should not be conducted until at least 6 hours have elapsed after the bleeding (Ahmed et al., 2014). This sampling period should be between 6-12 hours after the in vivo transformation of heme to bilirubin (Martin et al., 2013).
In labs where spectrophotometry is used, it is advocated that lumbar puncturing should be delayed up to twelve hours after the incident. However, in labs where a simple visual inspection is the method adopted, particularly in the United States, CT scanning is often done followed by lumbar puncturing for quick diagnosis, given the high influx of patients into the emergency department (Marcolini & Hine, 2019).
There is currently very little work published supporting the delay of lumbar puncture up to 12 hours. Recent works available on the issue of CSF xanthochromia have aimed at examining the superiority of using a spectrophotometer against inspection with the naked eye in detecting whether xanthochromia is present in the CSF (O’Glasser & Mansoor, 2015), (Chu et al., 2014), (Greenberg et al., 2018) and (Ahmed & Gibbons, 2016). It was concluded that spectrophotometry is more accurate at the detection of CSF xanthochromia as compared to a simple visual inspection. Several authors have published numerous pieces of literatures on the timing of surgery for SAH including Yao et al., (2017), Nieuwkamp et al., (2005) and Zhao & Wei, (2017). Ahmed et al., (2014) assessed the correlation of CSF xanthochromia with brain imaging and its importance and Martin et al (2013) conducted a study on the urgency of analyzing CSF xanthochromia samples and possible solutions to reducing the time it takes for results to be out. It was concluded that processing the CSF out of hours did lead to any significant changes and it affected clinical care negatively. Whereas the studies mentioned above are relevant to this research, there was no deep evaluation of what clinical effects the out of hours processing of CSF xanthochromia has, and also the significance it has on the discharge of patients. This is the basis on which this research was conducted. It evaluated whether or not CSF xanthochromia samples are processed out of hours, if not, then what clinical implications they had. It then examined whether incorporating the out of hour processing impacted on the timings of patient discharge. Was there be a reduction of the time spent in the Milton Keynes University Hospital by a patient who was awaiting diagnosis for SAH or any related condition?
Aims and Objectives
This research aims at evaluating the clinical impact of processing CSF xanthochromia out of hours and the significance it has on the timing of discharge of patients at the Milton Keynes University Hospital NHS Foundation Trust
The objectives of the study are:
To understand the processing and significance of CSF xanthochromia.
To examine the clinical impact of processing CSF xanthochromia out of hours at the Milton Keynes University Hospital NHS Foundation Trust
To assess how processing CSF xanthochromia out of hours affects the timings of patient discharge at the Milton Keynes University Hospital NHS Foundation Trust
Significance of the Study
Information obtained from the research will be beneficial to the medical personnel and the entire fraternity of the Milton Keynes University Hospital NHS Foundation Trust. It will also benefit patients who attend the hospital. The general public and future researchers will also benefit from this research.
METHODOLOGY
This study adopted a quantitative approach as the research design. There was the utilization of quantitative data to seek clarification into the ‘what’ of this research (Williman, 2017). For instance: what clinical impacts does out of hours processing of CSF xanthochromia have? What significance does out of hours processing of CSF xanthochromia have on patient discharge? The main purpose of quantitative research is to evaluate the relationship between two variables: the dependent variable, and the independent variables (Holcomb, 2016). The dependent variables in this research are the clinical impacts of out of hour processing of CSF xanthochromia and the significance on patient discharge that out of hour processing of CSF xanthochromia has. The independent variable in the research is the out of hour processing of xanthochromia. This is presented in the conceptual framework below.

The characteristics of data provided by quantitative research methods are that they are numerical and can be computed mathematically. The techniques used in this approach are standardized and not expensive to enforce (Patten & Newhart, 2017). The two types of quantitative methods used are either experimental or descriptive. In an experiment, there is intervention of the current situation to observe the ‘before’ and ‘after’ of the situation. It requires a very small sample and might need patience to obtain the desired results (Walliman, 2017). In a descriptive method, the data of the research is collected as the current situation is. There are no interventions put in place to alter that condition. This requires a tangible sample to gather enough information that will be useful to a research (Holcomb, 2016). The descriptive method was the one utilized in the research as it involved gathering information from the hospital without altering the current situation. In this research, close-ended questionnaires were distributed to both the daytime and out of hour admission, discharge and laboratory staff. A questionnaire is a data collection tool that is designed in the form of questions and/ or prompts for the participants to fill out (Williman, 2017). The questionnaires assessed whether samples of CSF obtained from patients were processed out of hours or not and the impacts thereof of making it a round the clock process. Did this have an effect on the clinical side or not? Did this affect patient discharge or not? Data was also obtained from the laboratory database and the admission and discharge records. This data was for the CSF xanthochromia requests received in the last twelve months. This provided information on the timings of admission, CSF sample collection for xanthochromia detection, timings for production of lab results and discharge time of the patient. Data about the positive and negative results was also obtained from these records. This made it possible for the examination of the negative predictive value of CSF xanthochromia screening. For the positive screens, brain imaging records of the patients were also obtained from the computer database. The sampling technique utilized was stratified sampling of the staff as they were classified into groups: Lab attendants, admission staff and discharging staff, then randomly selected a sample from each group. This ensured that those who answered the questionnaires were a representation of the target population. From the laboratory database, there was use of the keyword ‘xanthochromia’ which displayed a total of the xanthochromia lab procedures performed. The filter applied was period, in that it was narrowed to the previous twelve months to ensure up to date records were captured, and reduced the overload of data. Random selection was applied to obtain samples for the research. This was also replicated in the admission and discharge records. The patient records were then grouped according to age, gender and diagnosis outcome; both positive and negative outcomes.
Data analysis was done using Microsoft excel (a statistical software programme) to obtain descriptive statistics that summarized the data in a meaningful and simple way for easier interpretation (Patten & Newhart, 2017). Presentation of the data was done using graphs, pie charts and tables. The descriptive statistics allowed for the summation of large amounts of data collected during research and provided clarity in understanding the data. They also allowed for the comparison of the relationship between the dependent and independent variables of this research. The limitation of descriptive statistics is that the information collected only applies to the target population and cannot be replicated to other populations (Holcomb, 2016). For instance, the descriptive statistics that will be obtained during this research will be applicable only to the Milton Keynes University Hospital NHS Foundation Trust and might not be applied to other hospitals or medical facilities.
ETHICAL CONSIDERATIONS
Considering ethical issues before conducting any research is of utmost importance. Ethical issues ensure the protection of human and animal subjects in research and that their rights are not violated nor are they exposed to harmful procedures that might lead to fatal consequences or, worst-case scenario, death (Green, 2019). Ethical considerations also ensure the information provided in the research is genuine and not stolen from other people’s work (Drake, 2020). It protects against fabrication and wrong interpretation of information. The work of the researcher is also protected from replication by other future researchers (Nebeker et al., 2020) The public also trusts the work of a genuine researcher and might, therefore, provide funding for the research to be conducted especially if it is of great benefit to the public, environment or animals (Sobocan et al., 2019). Ethical considerations also enhance respect from both sides, the participant and the researcher, and ensures the researcher is held responsible for information generated to the public (Green, 2019). By following ethical considerations, researchers also abide by the rules and regulations put in place by certain institutions (Nebeker et al., 2020) This research put into consideration the ethical issues such as seeking consent from the Milton Keynes University Hospital NHS Foundation Trust before conducting the research. Consent was also sort from the laboratory, admission and discharge staff and communication was made to enable understanding about the research before agreeing to be participants. The questionnaires did not have sections for filling out names or contact details. This ensured anonymity in order to protect the confidentiality of the participants. Relevant departments also had to give approval for the generation of data from the computer databases and book records. Throughout the research, there was strict adherence to the rules and regulations of the Milton Keynes University Hospital NHS Foundation Trust to ensure that the operations and daily activities were not disrupted and the research was conducted smoothly.
RESULTS
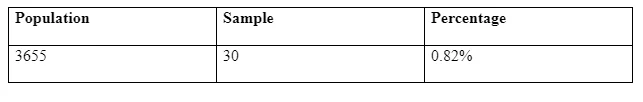
From the laboratory database, a total of 3655 laboratory xanthochromia procedures were obtained on search results after keying in the word ‘xanthochromia’ and after narrowing down the search to the last twelve months. There was then a random selection of the results according to months. For every month in the previous year, a maximum of three results were obtained. This gave a total of n=30 samples for the research. From which 50% (n=15) were male and 50 % (n=15) were female.
Sample representation as a percentage;
The negative and positive outcomes for the xanthochromia procedures were then obtained and calculated. Out of the 15 male patients, 26.6% (n=4) had positive outcomes and 73.3% (n=11) had negative outcomes. Out of the 15 female patients, 46.7% (n= 7) had positive, while 53.3% (n=8) had negative outcomes. This is shown in figure 4 below.

The negative predictive value of the total samples was calculated. The total value of the negative outcomes was (n=19), this was considered the number of patients not having the disease. The value was expressed as a percentage of the total number of patients using the equation shown below. This value was found to be 63.33%. The admission and discharge times were recorded. The time of CSF sample collection and time of production of results were also generated. For admission, 40% (n=12) cases were received in the morning hours, whereby 66.7% (n=8) CSF samples were collected within that period while 33.3% (n=4) were collected in the evening. For admission in the evening hours, 60% (n=180 cases were received all of which samples were collected on the following day in the morning hours. The results of the CSF xanthochromia samples collected in the morning came out in the evening or the following day while the samples collected in the evening hours came out the following day in the evening or even the day after. For the 63.33% (n=19) negative outcomes, 26.3% (n=5) were discharged within the same day, 47.4% (n=9) were discharged on the following day while 26.3% (n=5) were discharged after two days of admission. For the positive outcomes, 36.7% (n=11), discharge within 17 days was done to 63.6% (n=7) patients while 36.4% (n=4) were discharged within 30 days. Out of this, 63.6% (n=7) were readmitted into the hospital and discharged at various times. Questionnaires distributed to the admission, discharge and laboratory staff were 30, out of which 93.3% (n=28) were filled and 6.7% (n=2) were not filled. 43% (n=13) of the staff were comfortable with processing CSF xanthochromia out of hours, while 57% (n=15) deemed the idea not suitable. This is presented in figure 5 below.

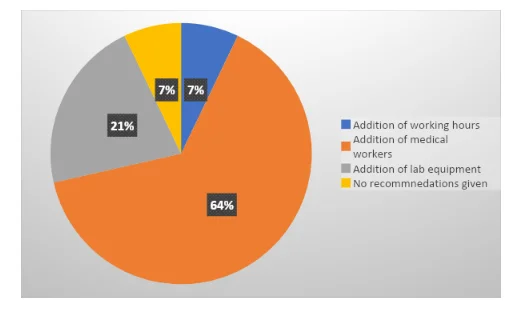
On the recommendations, 64.2% (n=18) saw that it was best to consider adding more medical workers to make it possible for the out of hours processing of CSF to be carried out. 21.4% (N=6) recommended addition of laboratory equipment including the spectrophotometer, and 7.1% (n=2) requested for more working hours.7.1% (N=2) did not recommend anything as they were totally against the out of hour processing of CSF. This is shown in figure 6 below.
DISCUSSION
From the database, there was a 0.82% representation of the population. This is a good representation of a population according to Schraders et al., (2020) study which demonstrated that 0.5% is an adequate percentage sample size. The characteristics of the population: Men and women and the negative and positive outcomes of SAH diagnosis, were also incorporated which minimized bias and sampling errors in the research. According to the results, women were at a higher risk of getting a SAH than men. Eden et al., (2008) studied that the risk of having SAH were related to gender and ethnic differences. Women are at high risks because of external factors such intake of contraceptives, hormonal therapy and internal factors such as reaching menopause (Gaist et al., 2004) and parity. Other predisposing factors include intake of alcohol, smoking cigarette, genetic differences among people (Marcolini & Hine, 2019) For the patients admitted in the morning hours, 40% (n=12), only 66.7% (n=8) of the patients had their CSF samples collected in the morning while 33.3% (n=4) had their samples collected in the evening. According to the questionnaires filled out by the admission, discharge and laboratory staff, it was possible to collect the CSF samples in the morning hours on days that the emergency room was not crowded with cases. This meant that on a busy day, with numerous cases flowing into the emergency room, SAH patients had to be delayed for some time before sample collection could be done. This enabled the medics to attend to the more urgent and fatal cases. The samples were then collected when the emergency cases had reduced. Putting into consideration that a CT scan needs to be done prior to a lumbar puncture, most of the patients who came in the morning were delayed until afternoon hours for the procedure to be performed. A CT scan is a necessary procedure done in the diagnosis of SAH. It has a 98% sensitivity if done promptly after the onset of sudden headache as it will detect the blood in the CSF before it gets diluted and converted into bilirubin. This sensitivity is reduced over time, therefore lumbar puncturing is done in patients who have negative CT scan outcomes (O’Glasser & Mansoor, 2015)
According to Zhao & Wei, (2017), immediately a cerebral aneurysm has burst open, blood leaks into the CSF in various volumes. With time, the blood undergoes degradation by macrophages and is transformed into bilirubin. This process takes 6-12 hours for the heme to be converted into bilirubin and only occurs in vivo. Due to this, it is reasonable to keep a patient waiting for at least 6 hours after they report the onset of sudden headache or a ‘thunderclap’ headache. It means that a potential SAH patient who reports to the Milton Keynes University Hospital in the morning, i.e. 0500 hours might undergo a lumbar puncture from 1100 hours onwards. For a potential SAH patient who visits the hospital at 1100 hours might undergo the lumbar puncture at 1700 hours earliest. From the n=19 negative outcomes, n=5 were discharged within the same day. This was possible if the test was done in the morning hours and results came in on time. Also, if the day was less crowded in the emergency department, it meant that the medics had ample time to work on the SAH cases. Putting into consideration the operating hours of the hospital that is from 0900 hours to 1900 hours on weekdays and 0900 hours to 1200 hours on weekends, most of the cases were pushed to the following day if there was limited time to work on the samples collected. This resulted in patients with negative diagnosis being discharged even after two days. For the positive cases, the discharge took as long as 17 to 30 days due to the treatment and management of SAH. A patient diagnosed with SAH might have to undergo magnetic resonance imaging (MRI) or a computed tomography angiography to detect the aneurysm and explain the cause of the SAH (Greenberg et al., 2018). Alternatively, treatment might begin immediately. Though the surgical treatment of SAH is minimally invasive, post-surgical complications often arise that could be neurological, cardiac, gastrointestinal, hematologic or infectious. When this happens, the patient is readmitted if they had been discharged (Nieuwkamp et al., 2005). In half of the positively diagnosed cases, it was clear from the brain imaging that an aneurysm had ruptured. This was detected because the CT scanning had been done as soon as there was onset of sudden headache. For the other positive samples, CT scans were negative. It was possible that the scan might have been done later after the onset of headache and red blood cell conversion had already occurred in the CSF. According to O’Glasser & Mansoor (2015), the probability of locating a SAH reduces after two hours after the onset of a ‘thunderclap’ headache. For the staff, 43% of the sample had agreed to the idea of CSF xanthochromia being extended to the out of hours to enable quick generation of results hence lead to prompt treatment and management of a SAH if the outcome is positive. The staff claimed it might disrupt the night schedule to some extent, but some activities performed at night could also be performed during the day. This was to be done by not compromising patient care at night. 57% of the sample disagreed to the out of hours processing as they saw that this would mean longer working hours and total disruption of the night schedule. Explanation was given that this would generally affect patient care at night.
According to Ahmed & Gibbons (2014), CSF xanthochromia has a weak positive predictive value of 8.7% while a stronger negative predictive value of 100%. From the results obtained in this research, the negative predictive value was found to be at 63.3%. This shows that the probability of a diagnosis having a negative outcome is higher than it having a positive outcome in the CSF xanthochromia. The questionnaires revealed that the out of hours processing of xanthochromia would have very little impact on patient discharge. This is because the patients would still have to undergo the proper medical procedure of CT scanning before a lumbar puncture, having the lumbar puncture after 6-12 hours after the onset of sudden headache and monitoring the patient for recurrent bleeding in the case of a SAH. Recommendations for the extension of working schedules at night were not well received by the staff at the hospital. It was explained that this would result to burn out and reduced job satisfaction in the medical staff, especially the night team. Addition of CSF xanthochromia processing into the out of hours activities was also viewed as impacting negatively on patient care at night. It meant that the night team would have more work on their hands than they can manage. A study conducted by Hamilton et al (2014) suggested that a fatigued medical worker affects the quality of care given to a patient. This is a risky situation as both the lives are affected. A medical worker experiences fatigue due to longer working hours with numerous cases to attend to. This gives them less working hours and leads to the creation of medical errors that could be avoided. The European Working Time Regulation (EWTR) implemented a reduction in the number of working hours by trainee doctors. The aftermath was that even though they were able to get adequate resting hours, it took longer to learn ‘craft’ specialties and patient care was compromised (Hamilton et al., 2014). In a similar study conducted by Stimpfel et al (2012), it was observed that a night in the hospital made it harder for medical workers to execute complicated responsibilities. The accuracy of decision making was also compromised. With this information, it proves that performing laboratory procedures like CSF xanthochromia at night could lead to making the wrong conclusions on a diagnosis.

It was suggested that the addition of medical workers to the hospital would ease the workload and ensure the working hours are reduced. Also, addition of laboratory medical equipment like the spectrophotometer and centrifuge were also part of the recommendations. This would enable smooth running of lab procedures and ensure activities within the hospital are carried out efficiently including out of hours CSF xanthochromia processing. Even though this is possible, it will take a long period of time for the hospital to implement this as it requires high financial input.
Limitations of the study
The sample representation, though recommended, gave a more room for creation of bias. It was not possible to sufficiently work with a bigger sample percentage due to the limited accessibility to available resources and time.
Future studies
Factors that lead to high negative predictive value in CSF xanthochromia outcomes will be incorporated in future studies. Possible solutions or recommendations to minimize the gap between the positive and negative predictive values will also be assessed. Having a lower negative predictive value will reduce the chances of patients being taken through painful and unnecessary medical procedures. Assessing sustainable solutions to the fatigue of medical workers should be studied in the future to minimize. Implementation of the possible solutions will minimize the negative impacts of fatigue on medical workers such as poor quality healthcare services, dangers or causing traffic accidents and medical job dissatisfaction.
CONCLUSIONS
Having the CSF xanthochromia processing done out of hours would ensure quick generation of lab results. This would ensure that a patient who has a SAH positive outcome would be treated promptly. However, in this study it was observed that the out of hour processing of CSF would not have much significance on reducing the length of stay of a patient at the Milton Keynes University Hospital as they would still have to undergo the required medical procedure. The out of hour processing of xanthochromia would also impact negatively on patient care at night and might even lead to burn out of the medical workers as they already have numerous activities being performed during the out of hours period.
References
- Koenig, M. (2008). Approach to the Patient with Bloody or Pigmented Cerebrospinal Fluid. Cerebrospinal Fluid in Clinical Practice E-Book, 267.
- Goyale, A., O’Shea, J., Marsden, J., Keep, J., & Vincent, R. P. (2016). Analysis of cerebrospinal fluid for xanthochromia versus modern computed tomography scanners in the diagnosis of subarachnoid haemorrhage: experience at a tertiary trauma referral centre. Annals of clinical biochemistry, 53(1), 150-154.
- Sobočan, A. M., Bertotti, T., & Strom-Gottfried, K. (2019). Ethical considerations in social work research. European Journal of Social Work, 22(5), 805-818.
- Greenberg, K., Binning, M. J., & Veznedaroglu, E. (2018). Severe Headache and Diagnosis of Subarachnoid Hemorrhage in the Emergency Department. In Intracranial Aneurysms (pp. 99-113). Academic Press.
- Stimpfel, A. W., Sloane, D. M., & Aiken, L. H. (2012). The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. Health affairs, 31(11), 2501-2509.
- Marcolini, E., & Hine, J. (2019). Approach to the diagnosis and management of subarachnoid hemorrhage. Western Journal of Emergency Medicine, 20(2), 203.
- Martin, S., Page, M., Godber, I., & McGregor, C. (2013). CSF xanthochromia analysis takes longer following centralisation of the laboratories testing samples-how can we improve the time to result? BMJ Open Quality, 2(2), u202450-w1177.
- Yao, Z., Hu, X., Ma, L., You, C., & He, M. (2017). Timing of surgery for aneurysmal subarachnoid hemorrhage: A systematic review and meta-analysis. International Journal of Surgery, 48, 266-274.
- O’Glasser, A. Y., & Mansoor, A. M. (2015). “If You Prick Us, Do We Not Bleed?” An Uncommon Cause of Xanthochromia. Journal of general internal medicine, 30(6), 853-854.
- Nieuwkamp, D. J., De Gans, K., Algra, A., Albrecht, K. W., Boomstra, S., Brouwers, P. J. A. M., & Tulleken, C. A. F. (2005). Timing of aneurysm surgery in subarachnoid haemorrhage–an observational study in The Netherlands. Acta neurochirurgica, 147(8), 815-821.
- Nebeker, C., Leavy, V., Roitmann, E., & Steinhubl, S. (2020). Ethical Considerations When Creating Evidence from Real World Digital Health Data. medRxiv.
- Chu, K., Hann, A., Greenslade, J., Williams, J., & Brown, A. (2014). Spectrophotometry or visual inspection to most reliably detect xanthochromia in subarachnoid hemorrhage: systematic review. Annals of emergency medicine, 64(3), 256-264.
- Salvo, G., Ramirez, P. T., Levenback, C. F., Munsell, M. F., Euscher, E. D., Soliman, P. T., & Frumovitz, M. (2017). Sensitivity and negative predictive value for sentinel lymph node biopsy in women with early-stage cervical cancer. Gynecologic oncology, 145(1), 96-101.
- Eden, S. V., Meurer, W. J., Sanchez, B. N., Lisabeth, L. D., Smith, M. A., Brown, D. L., & Morgenstern, L. B. (2008). Gender and ethnic differences in subarachnoid hemorrhage. Neurology, 71(10), 731-735.
- Gaist, D., Pedersen, L., Cnattingius, S., & Sørensen, H. T. (2004). Parity and risk of subarachnoid hemorrhage in women: a nested case-control study based on national Swedish registries. Stroke, 35(1), 28-32.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



