Exploring Person-Centred Practice in Healthcare
Activity 1
Introduction to person-centred practice
Person-centred practice is a critical aspect that is being devised by most of the care providing businesses with the purpose of addressing to different health care based needs of the patients. It has been observed that the emergence of different health care needs has significantly resulted to the development and growth of the person-centred practice in a health care setting (Santana et al. 2018). Therefore, the discussion would develop a comprehensive view on the person-centred practice approach, activities that might be considered by practitioners for training on person-centred practice and develop a comprehensive understanding on the medical and social models for the application of person-centred practice. Moreover, the discussion would also illustrate the challenges and dilemmas that might be encountered by the practitioners while delivering the person-centred practice to their patients.
Adopting a person-centred approach

Adoption of the person-centred practice requires empathy and understanding among the practitioners which is an integral part towards adhering to the healthcare based requirements of the clients. Håkansson Eklund et al. (2019) opined that empathy of the practitioners supports in developing cognition on the areas of treatment that might be expected by the clients while dealing with diverse range of diseases. Moreover, it has been observed that emotions play a vital role in empowering the capability of the practitioners in diagnosing the concerns while developing interventions for treating the healthcare based concerns that are encountered by different patients. As per the research made by Moore et al. (2019), around 49% of the patients require different treatments based on the their emotional criteria while suffering from a similar disease or ailment. In this connection, it has been observed that the person-centred practice is specifically focused towards empowering the capability of the medical practitioners in addressing the diverse needs of the patients.
The central idea of person-centred practice is based on empowering the practitioners to develop cognition on uniqueness of the patients while delivering treatment to the same as per the requirements. For an instance, a patient with a certain category of neurological disorder would differ from the other having most common nerve attacks, and thereby the treatment differs. Therefore, in this case, it has been observed that the differences in the treatment approach are specifically based on the uniqueness of the healthcare needs of the patient. The adoption of the person-centred practice is thereby based on identifying the emotional and psychological constructs of the patients (Nilsson, Edvardsson and Rushton 2019). The healthcare providers and practitioners must take the initiative of developing empathy towards understanding the psychological constructs and act accordingly on the interventions that might be made with the purpose of addressing to specific priorities and needs of the patient.
Continue your exploration of Saudi Arabia's Demographic Shift and Healthcare with our related content.
On the other hand, it has been observed that the knowledge of the practitioners and the service providers play an important role in empowering the degree of change in the interventions or treatments that are offered to the patients based on the care based needs. Haydon, Browne and van der Riet (2018) opined that the updated knowledge of the healthcare service providers and the practitioners on the different emerging psychological and ailment based concerns would allow the same in addressing the requirements of the person-centred practice. There are different biases and beliefs that are prioritized by the patients as per their psychological constructs. Therefore, a careful study of the psychological and emotional aspects of every patient while developing and delivering the treatments and interventions is a necessary activity that might be considered by the practitioners in order to address the needs of person-centred practice.
A resource that can be used for an activity in training staff and students on how to address different dilemmas typically faced by practitioners in implementing effective person-centred practice.
Resources act as an integral part towards improving the capability of a healthcare practitioner in developing and implementing the person-centred practice. It has been observed that case study reviews act as an inevitable resource towards informing the practitioners on the emerging psychological and emotional contrasts while making the same aware of the different interventions that were undertaken in the past. Arakelian et al. ( 2017) stated that case studies provide the healthcare practitioners with a practical example on the different areas of considerations that might be made by the same while delivering the medical interventions as per the healthcare based needs of the patients. It has been observed that the utilization of case studies support the medical practitioners in developing cognition on the practical concerns and the changing needs and requirements of the clients and the patients related to healthcare. Therefore, the utilization of case study based resources would support in developing cognition on the areas of change in the approach and the manner in which the patients might be attended as per their unique requirements.
Differences in the medical and social models and application to person-centred practice in health, care or support services
The medical models like transpersonal and humanitarian models might be applied in the context of person-centred practice. It has been observed that humanitarian models determine the approach and behavior of the practitioners while identifying the different discourses with the purpose of improving the degree of business operations. The different models are focused towards increasing the efficiency of the medical practitioners and providing the patients with a distinguished experience. Wallström and Ekman (2018) observed that the utilization of the medical models in the person-centred practice supports the practitioners in developing coherent understanding on the different areas of operations and the manner in which the same might be maintained. On the other hand, the social model of care is specifically focused towards developing a social structure with the purpose of accommodating the people with impairments. Ballard et al. (2018) opined that the social model of care is supportive towards developing a clear cognition on the changing areas of healthcare requirements among the people while addressing their expectations as per the needs. It supports the medical practitioners in developing capability on person-centred practice while delivering the treatments or the interventions to resolve the health concerns.
The challenges with applying person-centred care in the workplace setting
The major challenges that might be encountered by the practitioners while applying the concept of person-centred practice is specifically based on their inadequacy of knowledge on the changing healthcare based needs of the patients. The suitable application of person-centred practice is reliant on identifying the areas of psychological and emotional constructs among the people and thereby developing interventions or delivering treatments towards improving the aspects of operations. Naldemirci et al. (2017) opined that the insufficiency of empathy among the practitioners by their so called professionalism has limited their scope on implementing person-centred practice. The people or the patients mostly expect the practitioners to develop sufficient research on their mental and psychological aspects before entreating them with any interventions. However, the incapability of the practitioners, in this connection, is specifically based on their insufficiency of empathy towards understanding the psychological aspects that drives the expectations of the people. On the other hand, Naldemirci et al. (2018) opined that the inadequacy of knowledge among the practitioners on the emerging modern treatment resources or the diseases and ailments might incapacitate their efforts towards implementing a person-centred practice. Identification of the unique concerns of the patients and thereby developing interventions require a steady and continuous learning approach on the psychological aspects and the psychological or emotional constructs of the patient. Failing to gather adequate knowledge on the different areas has been acting as a restrictive aspect towards implementing the person-centred practice by the practitioners.
Dilemmas in workplace setting can affect an implementation of person-centred practice
Dilemmas might create a delusionary effect on the successful implementation of person-centred practice in a health care setting. Ekman et al. (2020) opined that dilemmas in the health care setting acts as a provocative aspect towards reducing the capability of a practitioner in deploying the person-centred practice. Dilemmas like refusal of care by a single patient are integral that affects the capability of a practitioner in implementing person-centred practice. Refusal of care is a kind of dilemma that specifically arises when the subject or the patient refuses to be cared when the same is in death bed or critical condition. The application of the person-centred practice would thereby contradict with the traditional stereotype of the practitioners. The aspect might create a situation where the practitioner might encounter a significant challenge in implementing the person-centred practice while adhering to their own professional responsibility towards the patient.
Conclusion
Therefore, it might be stated that the person-centred practice is an approach that is based on identifying the emotional and psychological constructs of the patients, uniquely, while developing and delivering treatment based interventions on the basis of their needs. Most of the healthcare providers and the practitioners have developed competence on the person-centred practice with the purpose of addressing to the emerging healthcare needs of the patients. However, the inability of a healthcare provider in developing sufficient understanding on the areas of health care attention that is required by the client or the patient might limit the scope of person-centred practice. However, through the research it was found that there are several dilemmas and challenges that might be encountered by a practitioner while implementing the person-centred practice in a healthcare setting.
Activity 2
Legislation in person-centred practice
The Regulation 9 of Health and Social Care Act 2008 aims at identifying the essence of the person-centred practice and the manner in which the personalized care must be catered to the people or the patients. The legislation and regulation specifically focuses towards understanding the type of practice that might be considered by the practitioners in order to adhere to the changing needs of the patients. The regulation suggests the practitioners to closely partner or collaborate with the patients in order to identify their concerns and thereby devise unique interventions on treatments with the purpose of addressing the specific healthcare based needs of a patient. The approach of person-centred practice is widely reflected through the positioning of the regulation while guiding the activities of the practitioners towards developing a collaborative function with that of the patients. Gondek et al. (2017) opined that the Health and Social Care Act 2008 is specifically focused towards improving the degree of person-centred care among the practitioners while developing sufficient capabilities towards improving their understanding on the changing or unique needs of the patients. Therefore, it might be stated that the implementation of the legislation or the regulation has significantly sup[ported the practitioners in developing a clear cognition on the person-centred practice and the manner in which the different needs and healthcare requirements of the patients might be addressed through close association and partnering.
Challenges in interpreting legislations
The interpretation of the legislations require empathetic attitude while identifying the uniqueness of the situation and designing interventions as per the guidelines of a law. The incapability of the practitioners in developing a clear cognition on the situation might affect their capability of interpreting the legislative requirements effectively. Burton et al. (2017) stated that the person-centred practice is specifically guided through the knowledge, cognition and empathy of the practitioners while identifying and interpreting the legislative requirements while undertaking any action. The different areas of change in the approach of person-centred practice are based on the imposition of legislative requirements and the interpretation of the same while devising intervention procedures. In this connection, the incapability of the practitioners in developing clear cognition or interpretive skills on the legislative requirements in diverse situations might affect the scope of the person-centred practice.
Effectiveness of health and safety and safeguarding systems in own workplace setting in meeting legislative requirements
The health and safety systems in a healthcare setting act as a means of developing capability on the various areas of operations while addressing the aspects of the person-centred practice. It has been observed that the health and safety systems provide a systematic outlook on the different concerns that might be encountered by the patients and the practitioners. Öhlén et al. (2017) opined that the health and safety systems provide a systematic background to the operations that are conducted by the practitioners while addressing the personalized needs and requirements of the patients. In this connection, the development of efficient health and safety systems support a healthcare practitioner in developing capability on the interventions while meeting the legislative requirements and addressing the personalized care related needs of the clients or the patients.
Solutions to different concerns in addressing different legislations in a health and care setting
The major aspects that might be considered by the practitioners in order to address different legislations without meeting any challenges is through the identification of the requirements and continuously learning different aspects. It has been observed that the identification of the concerns and mitigation through the utilization of different legislative interventions would allow the practitioners in developing coherent systems while addressing to the specific needs and requirements of the patients. In this connection, it has been observed that the practitioners must ensure continuous learning with the purpose of ensuring sufficient knowledge on the different changing legislative requirements. van der Meer et al. (2018) opined that a clear understanding of the legislative requirements and continuous learning attributes support a practitioner in developing capability on the efficiency of person-centred practice. Several concerns based on the lack of knowledge on the changing legislative requirements might affect the capability of the practitioners in delivering the person-centred practice. Therefore, the person-centred practice of the practitioners might be developed through a clear understanding on the legislative requirements and continuous learning attributes in order to stay updated on the recent changes in the legislations.
Activity 3
Comparative reflective account of person-centred care
Person-centred care involves the critical understanding on the healthcare based needs of the patients and the clients while delivering suitable interventions as per their emotional and psychological constructs. Cederwall et al. (2018) opined that the person-centred care is specifically reliant on developing a clear cognition on the driving motives and the emotional constructs of the people while devising efficient medical intervention techniques. In this connection, I believe that close partnership or collaboration with the patient is a necessity with the purpose of improving knowledge and capability of a practitioner while providing person-centred care. Knowledge on the emerging healthcare concerns and the different areas of emotional constructs that guides or motivates the clients is integral towards developing efficient person-centred care activities. Summer Meranius et al. (2020) stated that communication with the clients and consistent collaboration are the chief aspects in the person-centred care setting while providing healthcare services. Therefore, I believe that the identification of the concerns and the mental constructs of the people or the analysis of their needs is possible through efficient communication with the patient while taking the same into confidence.

Managing workload as a part of the team while offering person-centred care
Managing workload is integral towards improving the performance of a practitioner. It has been witnessed that different changes in the organizational operations are reliant on the efficient functioning of the systems while addressing the strategic needs and requirements of the people. On the other hand, it has been observed that the collaborative functioning is an integral part while operating through a team of experts. In this connection, the management of workload enables a practitioner in developing capability of finishing the tasks within the deadlines and contributes towards improving the performance of the teams. Pirhonen et al. (2017) opined that managing workloads and delivering the tasks within deadlines supports a team in increasing their performance while aligning with the organizational objectives. Therefore, every individual in a team must contribute towards ensuring an effective management of their work load with the purpose of developing their capability on delivering person-centred care.
Evaluation of practices in enabling a consistent approach to high-quality care in different health and care settings
The medical practitioners take on the sole responsibility of communicating with the patients and the clients while identifying their concerns and priorities. The identification of the priorities, interests and concerns of the patients and resolving the concerns through the implementation of standard interventions has been one of the major aspects of person-centred care. In this connection, Dellenborg, Wikström and Erichsen (2019) opined that the practitioners collaborate with the patients while developing clear insights on their healthcare based needs and treating the same separately. The personalized treatment of the practitioners is based on the idea of providing extensive range of care treatments and medical interventions as per the diverse medical needs of the patients. In this connection, a close collaboration or partnering with the patient is an integral part of person-centred care. The high quality person-centred care is based on the quality of understanding on the changing priorities and needs of the patients while treating them uniquely and negating all stereotypes and biases from the side of the practitioner (Bhattacharyya et al. 2019). Therefore, the person-centred care is reliant on the quality understanding on the needs of the patients while developing unique medical interventions that are suitable towards the priorities and needs of the patient.
Short, medium and long-term plan for improving skills in providing person-centred care
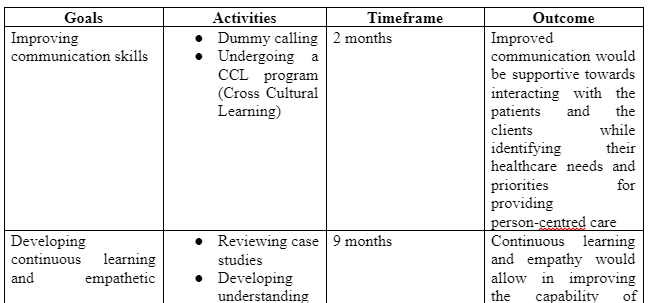
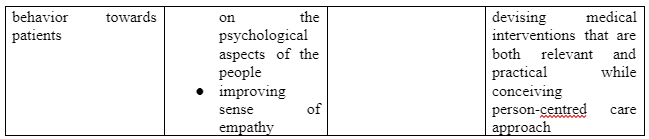
The short term plan for improving the skills in providing person-centred care is specifically based on improving my performance while communicating with the patients
The long term plan for improving my skills on person-centred care would be related to building on empathy and continuously learn the new health care based trends and requirements of the clients and the patients
Practicality of the plans
The practicality of the plans is specifically based on improving the degree of professional and personal capabilities towards instilling a better prospect in terms of person-centred care. In this connection, the short term plan 0of improving communicability with the clients or the patients would be helping me to understand their concerns and act accordingly on the medical interventions while treating the same with a better personalized experience. On the other hand, the long term plan of continuous learning and improving my empathy would allow me in developing skills on increasing effectiveness and growth while instilling the values and idea of person-centred care.
Reflective action plan for personal and professional development
References
Arakelian, E., Swenne, C.L., Lindberg, S., Rudolfsson, G. and von Vogelsang, A.C., 2017. The meaning of person‐centred care in the perioperative nursing context from the patient's perspective–an integrative review. Journal of clinical nursing, 26(17-18), pp.2527-2544.
Ballard, C., Corbett, A., Orrell, M., Williams, G., Moniz-Cook, E., Romeo, R., Woods, B., Garrod, L., Testad, I., Woodward-Carlton, B. and Wenborn, J., 2018. Impact of person-centred care training and person-centred activities on quality of life, agitation, and antipsychotic use in people with dementia living in nursing homes: A cluster-randomised controlled trial. PLoS medicine, 15(2), p.e1002500.
Bhattacharyya, O., Blumenthal, D., Stoddard, R., Mansell, L., Mossman, K. and Schneider, E.C., 2019. Redesigning care: adapting new improvement methods to achieve person-centred care. BMJ quality & safety, 28(3), pp.242-248.
Burton, C.D., Entwistle, V.A., Elliott, A.M., Krucien, N., Porteous, T. and Ryan, M., 2017. The value of different aspects of person-centred care: a series of discrete choice experiments in people with long-term conditions. BMJ open, 7(4), p.e015689.
Cederwall, C.J., Olausson, S., Rose, L., Naredi, S. and Ringdal, M., 2018. Person-centred care during prolonged weaning from mechanical ventilation, nurses’ views: an interview study. Intensive and Critical Care Nursing, 46, pp.32-37.
Dellenborg, L., Wikström, E. and Erichsen, A.A., 2019. Factors that may promote the learning of person-centred care: an ethnographic study of an implementation programme for healthcare professionals in a medical emergency ward in Sweden. Advances in Health Sciences Education, 24(2), pp.353-381.
Ekman, N., Taft, C., Moons, P., Mäkitalo, Å., Boström, E. and Fors, A., 2020. A state-of-the-art review of direct observation tools for assessing competency in person-centred care. International Journal of Nursing Studies, p.103634.
Gondek, D., Edbrooke‐Childs, J., Velikonja, T., Chapman, L., Saunders, F., Hayes, D. and Wolpert, M., 2017. Facilitators and barriers to person‐centred care in child and young people mental health services: A systematic review. Clinical psychology & psychotherapy, 24(4), pp.870-886.
Håkansson Eklund, J., Holmström, I.K., Kumlin, T., Kaminsky, E., Skoglund, K., Höglander, J., Sundler, A.J., Condén, E. and Summer Merenius, M., 2019. Same same or different? A review of reviews of person-centred and patient-centred care. Patient education and counseling, (1), pp.3-11.
Haydon, G., Browne, G. and van der Riet, P., 2018. Narrative inquiry as a research methodology exploring person centred care in nursing. Collegian, 25(1), pp.125-129.
Moore, L., Britten, N., Lydahl, D., Naldemirci, Ö., Elam, M. and Wolf, A., 2017. Barriers and facilitators to the implementation of person‐centred care in different healthcare contexts. Scandinavian journal of caring sciences, 31(4), pp.662-673.
Naldemirci, Ö., Lydahl, D., Britten, N., Elam, M., Moore, L. and Wolf, A., 2018. Tenacious assumptions of person-centred care? Exploring tensions and variations in practice. Health, 22(1), pp.54-71.
Naldemirci, Ö., Wolf, A., Elam, M., Lydahl, D., Moore, L. and Britten, N., 2017. Deliberate and emergent strategies for implementing person-centred care: a qualitative interview study with researchers, professionals and patients. BMC health services research, 17(1), pp.1-10.
Nilsson, A., Edvardsson, D. and Rushton, C., 2019. Nurses’ descriptions of person‐centred care for older people in an acute medical ward—On the individual, team and organisational levels’. Journal of clinical nursing, 28(7-8), pp.1251-1259.
Öhlén, J., Reimer‐Kirkham, S., Astle, B., Håkanson, C., Lee, J., Eriksson, M. and Sawatzky, R., 2017. Person‐centred care dialectics—Inquired in the context of palliative care. Nursing Philosophy, 18(4), p.e12177.
Pirhonen, L., Olofsson, E.H., Fors, A., Ekman, I. and Bolin, K., 2017. Effects of person-centred care on health outcomes—a randomized controlled trial in patients with acute coronary syndrome. Health Policy, 121(2), pp.169-179.
Santana, M.J., Manalili, K., Jolley, R.J., Zelinsky, S., Quan, H. and Lu, M., 2018. How to practice person‐centred care: A conceptual framework. Health Expectations, 21(2), pp.429-440.
Summer Meranius, M., Holmström, I.K., Håkansson, J., Breitholtz, A., Moniri, F., Skogevall, S., Skoglund, K. and Rasoal, D., 2020. Paradoxes of person‐centred care: A discussion paper. Nursing Open, 7(5), pp.1321-1329.
van der Meer, L., Nieboer, A.P., Finkenflügel, H. and Cramm, J.M., 2018. The importance of person‐centred care and co‐creation of care for the well‐being and job satisfaction of professionals working with people with intellectual disabilities. Scandinavian journal of caring sciences, 32(1), pp.76-81.
Wallström, S. and Ekman, I., 2018. Person-centred care in clinical assessment.
Dig deeper into Exploring Mental Health Challenges Among University Students with our selection of articles.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



