Shadowing and Collaborative Clinical Learning
A completed reflection/worksheet to evaluate and articulate learning from shadowing another professional
It is important for me to articulate learning from shadowing another professionals, present in the workplace, so that I is beneficial for me to gather vast knowledge and understanding about clinical skill and practice to treat the patient strategically. In this regard, I try to learn how to work cooperatively in the workplace so that the health and social care professionals can collaborate with each other and maximise the values for the patients. As the physiotherapist, I need to work with other working professionals and health and social care service providers, nurses and staff at the workplace so that I can manage proper time to treat the patients well and give them proper therapy and treatment for improving their health condition. At the workplace, there are many patients, who cannot move from one place to another due to stroke where some patients are suffering of paralysis (Ambrose-Miller and Ashcroft, 2016). In this case, I need to take active part and cooperate with other health and social care professionals in order to treat the stroke patient proficiently so that the individual can do effective movement and improve their heath condition. In this context, I try to cooperate with other care professionals, doctors and other nurses to understand the actual health needs and acknowledge the treatment process that the patients are going through. This is important to cooperate with all of the health and social care professionals to manage the patients proficiently with proper treatment and therapy. I try to improve communication where I share my feeling and capabilities professionals for shadowing the skill and clinical knowledge. Respecting all of them at the workplace and positive attitude further help me to enhance internal communication with the working professionals where I try to work as a partnership basis. In this regard, I also aim at improving time management during the treatment so that I can get proper time to treat the patient and help them to move from one place to another. In addition to this, continuous message of the paralysed areas of the body as well as radiation treatment for physiotherapy are important for me and in this regard, I try to gather more knowledge and clinical experience through treating a vast range of people with different needs. This in turn helps me to communicate with doctors and nurses and gather ideas to treat the patients with quality care and effective treatment. On the other hand, I also try to improve team working skill to treat the patients, where I need to cooperate with the nurses so that the staff and nurses can help me to move the patients and cooperate with them for better movement through messaging and exercise. These are important technique, which I am focusing during my professional field to treat the patient with quality care and proper treatment. Good physical health and time management are also necessary where I try to follow the physical fitness of other doctors and health care professionals as well as improve my knowledge to treat the patients with quality care. in this regard, my communication skill and interactive power further help me to interact with the patients and build strong relationship with them, so that the patients can feel free to communicate with me and share their experience and health needs. The ability to build rapport with the patients as well as strong relationship with other health care professionals further provide me an opportunity to improve my knowledge and understanding to treat the patients with quality care and effective treatment, messaging, radio therapy and exercise so that I can ensure patient’s movement after such effective physiotherapy. In this context, I try to ensure better care and lifting through daily exercise and messaging, where there many stroke patients who are suffering from paralysis. They cannot move properly due to paralysis of some body parts and in this situation, I try to gain experience through working with other professionals and improve my problem solving and interpersonal skill to develop proper care plan for the patients and manage time to cooperate with others and enhance team working activities at the organisation so that all the health and social care professionals, nurses and doctors can collaborate to deliver high quality care and support to the stroke patients, and in this regard, I also try to cooperate with all of them to help the patients to get proper treatment, message, exercise so that the patients can move properly.

A case study that analyses/evaluates how an inter-professional team worked together to implement a NICE guideline
As per the NICE guidelines, it is necessary to improve rehabilitation for the people, who have had a stroke where the multidisciplinary stroke team aims to enhance the quality of life of the patients with continuing impairment, activity limitation and participation restriction. As a physiotherapist, it is the responsibility to develop proper care plan for the patients to deliver high quality care and support to the patients where they can overcome theory barriers and can make effective movement (Sims, Hewitt and Harris, 2015). The multidisciplinary stroke team in this regard plays a crucial role in treating the patients with quality care, support and continuous treatment and medication. There is a serious case of the stroke patient, where the patients have had a serious stroke for which the left side of the patients had paralysed. It is the role of the multidisciplinary stroke team to treat the patient with quality care and support as well as proper therapy, medication for providing support to the patient so that they can move from one place to another. As per the case study, the multidisciplinary stroke team aim to work cooperatively with the pat nets and his or her family members in order to work proficiently and develop professional culture to treat the patients with proper medication and therapeutic assessment. Due to paralysis during stroke, the patients are not able to move from one place to another and they are also unable to participate in daily activities properly. Hereby, the team members need to be concerned about the progress of the patients and ensure continuous progress of the patient through medication, therapy and exercise. In this regard, all the nurses and health and social care professionals need to cooperate and coordinate to treat the patient with quality treatment and support (O’Carroll, McSwiggan and Campbell, 2016). In order to provide proper treatment and quality care and support to the patients, it is necessary for the doctors, professionals and nurses to follow the NICE guideline so that the patients can improve their condition and move from one place to another. In this regard, the health and social care professionals develop proper care plan in order to treat the patients and empower the patient in the care plan to acknowledge the personal perspective, experimentation and health needs of the individual. In this regard, the proper empowerment of the patient in the care plan is beneficial for the health and social care professionals to develop effective treatment and therapeutic assessment so that the patient can get proper medication, physiotherapy and exercise and message from the physiotherapist (Green, and Johnson, 2015). Hereby, in order to implement the NICE guidelines in the organisation, it is necessary to have proper empowerment of the patients in developing the care plan for getting high quality treatment and acre. In addition to this, as per the NICE guidelines, it is necessary to develop patient centred care, where the physiotherapy try to communicate with the patients and interact positively to create suitable and friendly atmosphere, where the patients can share their experience and personal preferences towards getting proper treatment and support from the physiotherapist (Glaser and Suter, 2016).

In this context, the physiotherapist also focuses on explaining the benefits of treatment, medication and physiotherapy for the patient so that the individual can understand the advantages of getting the care and support from the physiotherapist and other health care professional so that the individual can improve their participation and get back to normal life (Arnold and Boggs, 2019). Moreover, during patient’s involvement, it is necessary as per the NICE guidelines, to have proper cooperation and communication with the family member of the patients so that it is possible to acknowledge the patient’s personal behaviour, preferences as well as coordinate with them for better care. This is important to improve satisfaction level of the patient where the patient becomes interested to cooperate with the physiotherapist to get proper treatment and care for them in order to get stretch and move properly (Mangan, Miller and Ward, 2015). Hereby, in order to implement the NICE guidelines, it is the responsibility of the physiotherapist, doctors, health care professional, general physicians and nurses to cooperate with each other and develop inter professional team work so that they can treat the patients with proper treatment, therapy, medication and exercise. In this situation, for stroke patient, the individual needs all the health care professional such as general physicians, physiotherapist and nurses as well as other doctors, for diagnosing their health condition on a daily basis and give them continuous support and care according to their health needs and personal preferences (King et al., 2015). Hereby, the activities for developing patient centred care are effective to treat the stroke patients with proper treatment, therapy and medication as well as give them quality care and proper support for their successful movement.
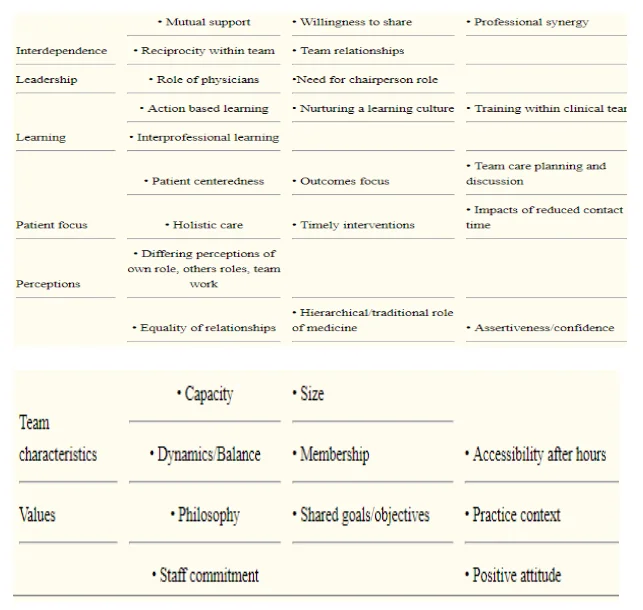
In addition to this, the organisational culture is one of the crucial factors for developing inter professionals team working for implementing NICE guidelines, where the personal qualities, trust and loyalty to each other as well as team culture and inter-professional atmosphere provide a scope to all the team members to work proficiently (Bookey‐Bassett et al., 2017). In this regard, the communication plays a curial role in developing the inter professional team working practice, where the intra team communication, positive interaction with others at the workplace as well as respect others are effective for the health care professionals to develop inter professional working practice where it is possible for the health care professionals to develop clear planning for the patient who is suffering for stroke, and in this regard, there is an important role of the physician to treat the stroke patient for their better movement and participation in daily activities (Glasby, 2017). Hereby, the practice of communication with each other, as well as the organisational atmosphere with respect, mutual benefits trust and loyalty to each professional is effective for better performance and implementing the NICE guidelines efficiently at the organisation in order to deliver quality care and high standard of treatment to the patients (Surr et al., 2017). Interdependence to each other as well as the team relationship is other important factors for contributing team building activities and developing inter professionals working practice at the organisation. It is hereby, the roles and responsibility for the doctors, physiotherapist and nurses and general physicians to cooperate with each other and develop proper team to support the patients and treat them with quality care. The leadership style of the health care organisation is another important factor, where the leaders provide proper training and development program to the health care professional as well as encourage the members to be cooperative and communicative for sharing their knowledge and skill successfully. This in turn helps to share their experience to each other and gave each others to enhance their clinical skill to treat the stroke patient efficiently with proper treatment, medication, therapy and exercise (Gradinger et al., 2015). Maintaining quality at the organisation, respecting each other and building strong relationship with all the health care professionals are effective to implement the NICE guidelines for delivering quality care and standard treatment to the stroke patients so that they can overcome their health condition. Professional commitment in this regard is also necessary for developing inter professionals working practice, where the staff members, nurses and health care professionals can cooperate and communicate for better performance (Coughlan and Cronin, 2016). Hereby, the leadership style as well as organisational atmosphere to work collaboratively and share each other’s experience for better performance.
Core professional skill and capabilities of the team members need to be enhanced through training and development program, where the care professionals need to be professional and develop proper practice to treat the patient efficiently (Barbaglia et al., 2017). In this regard, for the stroke patient, it is necessary to give them proper treatment and care according to their health condition. They need proper medication for continuous improvement of their health condition. On the other hand, the patient needs proper therapy such as radio therapy for overcoming the problem of paralysis as well as they need exercise and messages from the physicians for better movement and participation. Hereby, all the doctors, general physicians, physiotherapist ad nurses need to be cooperative and work as a team in order to treat the stroke patient. In this situation, the nurses, physiotherapist and general physician need to diagnose the patient continuously and provide proper medication and exercise and message to them so that they can move from one place to another. In addition to these, it is necessary for the health care professionals to develop proper understanding and manage own roles and responsibility, which is necessary for them to collaborate and coordinate with other professionals and develop inter professional team working practice in the workplace to treat the stroke patients with high standard treatment and maintaining the NICE guidelines (Cederwall et al., 2018). Staff commitment is another factor, where it is necessary for all the professionals top manage own responsibility and fulfil own commitment at the workplace so that they can be cooperative and respect each other for working together. The training and development program in this regard plays an important role where all the members can share each other’s knowledge and experience as well as build strong relationship among the staff members and care professionals to improve their understanding and enhancing cooperation in the team, so that they can work collaboratively and develop inter professionals team working practice to treat the stroke patients (Vasquez et al., 2019). Shared gaol is other important aspects of developing inter professionals working practice, where the team member tries to share their activities and improve communication for better performance. Additionally, positive attitude towards each other as well as creating values for each other are also improve mutual trust and respect which in turn helps to motivate the team members to be coordinate and maximise the quality of care in the workplace. Openness and trust to each other as well as maintaining organisational hierarchy are effective for implementing the partnership working practice, where each member respect other’s decision and develop the best possible care plan for the patients. Hereby, the actions and practice of treating the stroke patient are effective to develop inter professionals team working practice where the health and social care professionals ensure that it is possible to implement the NICE guidelines to maximise the values of the patients and treat the patients with quality care, continuous support, physiotherapy, exercise, medication and message for improving the patient’s movement and participation (Nieuwenhuis et al., 2019).

A reflection (using Borton’s model) about inter-professional working and person-centred practice following discussions at an in-service training session on the NHS Plan
As per the Borton’s model, it is possible for me to share my experience and knowledge and reflect about own understanding about the inter-professional working and person-centred practice following discussions at an in-service training session on the NHS Plan. Through reflecting and reviewing my own experience and understanding, it is possible to explain the practice of inter professional working practice and developing patient centred care as well as discuss future actions to improve collaborative working practice so that I would be able to deliver high quality care to the stroke patients in near future, where I would be efficient enough to treat all the patient and give them proper physiotherapy for improving their movement. As per the Borton’s reflective model, there are three stages such as what, so what and now what through which it is possible for me to hare my experience and feelings about the incident or event taken place in the workplace while treating the stroke patient to ensure patient centred care by ensuring inter professionals working practice.
What: Describing the event or actions taken place in the workplace
In order to enhance the team cooperation and collaboration among the other staff members it is necessary for the organisation to develop inter professionals working practice, so that every health and social care professionals and nurses and doctors can cooperate with each other for better performance. In this context, the action of providing training and development program to all the health care professionals is one of the events which provide an opportunity to the members to gain in depth knowledge and clinical skill or treating the patient with quality care and support. During the training program, all the professionals are cooperating and sharing their experience while working with the stroke patients and this is effective for me to gain more knowledge successfully.
In addition to these, the action of supporting each other with proper knowledge and skill is also important in the NHS plan to enhance the inter professionals working practice where all the professionals are collaborating and developing team working practice for working as partnership basis. Sharing views, experience and clinical skill is possible under this action, where all the professionals are respecting each other and manage internal environment to work cooperatively with freedom and integrity. The actions of working as a team is possible in this organisational culture, where openness, trust, building strong relationship with all the health care service providers as well as collaboration, cooperation and coordination further enhance communication and team working activities at the workplace, which in turn helps to ensure patient centred care in the organisation (Papadimitriou and Cott, 2015). Proper empowerment of each team members as well as empowering the patients in the care plan are another action as per the NHS plan, which is also effective for me to enhance my abilities to improve engagement with the patients and provide a chance to them to share their personal preferences to develop effective care plan.
So what: Explaining why that action or event was significant
The actions for inter-professional working and person-centred practice at an in-service training session on the NHS Plan are effective for motivating all the health and social care professionals to work collaboratively and share each other’s knowledge, clinical skill and experience for better performance as per my overview, the actions and events taken place for improving the inter professionals working practice and patient centred care are effective for me as a physiotherapist as it provides a scope to empower the patient in the care plan and effective care by maintaining high quality standard of care. It further effective to reduce the significant communication gap as well as enhance the international interaction, where all the members start work with each other through improving cooperation and coordination. The actions and strategies to develop inter professional team working and developing patient centred care are effective for me to enhance my knowledge and capabilities by working cooperatively, where I can gather knowledge from other professionals and ensure to deliver patient centred care according to the patient’s preferences and health needs as a physiotherapist so that the patients can feel valued. Building trust and strong relationship with the patients as well as with other professionals at the workplace are the significant benefits for developing the tactics of inter professional team working practice.

Now What: Explaining how you will use that information to inform future practice
The mentioned actions and planning for inter professional working practice and developing patient centred care will be effective for me where I can improve my capabilities and knowledge as well as gather clinical experience while working with other professionals. It will give me a scope to treat the patient with quality care and acknowledge their health need and personal preferences to give the stroke patients proper physiotherapy, treatment and support for better movement of their body. In addition to these, the tactics of sharing each other’s experience as well as the training and development program at the organisation will also be beneficial for me to improve my performance where I aim to support the stroke patients with proper experience, messages and physiotherapy treatment through giving radio therapy so that the patients can move from one place to another. Moreover, the support from the team members and cooperation and internal communication further will motivate me and improve my experience to work collaboratively as partnership basis. It is necessary to acknowledge the health condition and medical observation of the patient and for this; I need to communicate with all the team members and health care professionals for handling the patients successfully with proficient care and support.
Reference List
Ambrose-Miller, W. and Ashcroft, R., 2016. Challenges faced by social workers as members of interprofessional collaborative health care teams. Health & social work, 41(2), pp.101-109.
Barbaglia, G., Reynolds, J., Arcas, M., Domingo, L., Espallargues, M., Espaulella, J., Ramon, I., Segales, M., Serrarols, M., Molist, I. and Viña, N., 2017. Inter-professional coordination: first step towards a more person-centred approach. Improvement projects in Catalonia within the framework of the SUSTAIN project. International Journal of Integrated Care, 17(5).
Bookey‐Bassett, S., Markle‐Reid, M., Mckey, C.A. and Akhtar‐Danesh, N., 2017. Understanding interprofessional collaboration in the context of chronic disease management for older adults living in communities: a concept analysis. Journal of advanced nursing, 73(1), pp.71-84.
Cederwall, C.J., Olausson, S., Rose, L., Naredi, S. and Ringdal, M., 2018. Person-centred care during prolonged weaning from mechanical ventilation, nurses’ views: an interview study. Intensive and Critical Care Nursing, 46, pp.32-37.
Glaser, B. and Suter, E., 2016. Interprofessional collaboration and integration as experienced by social workers in health care. Social work in health care, 55(5), pp.395-408.
Gradinger, F., Britten, N., Wyatt, K., Froggatt, K., Gibson, A., Jacoby, A., Lobban, F., Mayes, D., Snape, D., Rawcliffe, T. and Popay, J., 2015. Values associated with public involvement in health and social care research: a narrative review. Health Expectations, 18(5), pp.661-675.
Green, B.N. and Johnson, C.D., 2015. Interprofessional collaboration in research, education, and clinical practice: working together for a better future. Journal of Chiropractic Education, 29(1), pp.1-10.
King, O., Nancarrow, S.A., Borthwick, A.M. and Grace, S., 2015. Contested professional role boundaries in health care: a systematic review of the literature. Journal of foot and ankle research, 8(1), p.2.
Mangan, C., Miller, R. and Ward, C., 2015. Knowing me, knowing you: inter-professional working between general practice and social care. Journal of Integrated Care, 23(2), pp.62-73.
Nieuwenhuis, L., Hoeve, A., Kuijer, W. and Peeters, A., 2019. Innovation and Practice-based Research. The Case of Dutch Vocational and Professional Education. Work-based Learning as a Pathway to Competence-based Education, p.273.
O’Carroll, V., McSwiggan, L. and Campbell, M., 2016. Health and social care professionals’ attitudes to interprofessional working and interprofessional education: A literature review. Journal of Interprofessional Care, 30(1), pp.42-49.
Reeves, S., Pelone, F., Harrison, R., Goldman, J. and Zwarenstein, M., 2017. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews, (6).
Sims, S., Hewitt, G. and Harris, R., 2015. Evidence of a shared purpose, critical reflection, innovation and leadership in interprofessional healthcare teams: a realist synthesis. Journal of Interprofessional Care, 29(3), pp.209-215.
Surr, C.A., Gates, C., Irving, D., Oyebode, J., Smith, S.J., Parveen, S., Drury, M. and Dennison, A., 2017. Effective dementia education and training for the health and social care workforce: a systematic review of the literature. Review of educational research, 87(5), pp.966-1002.
Vasquez, D., Deland, L., Spears, K., Metcalfe, L., Frost, S. and Christensen, M., 2019. Time is Precious: person-centred end of life care in an emergency department. A quality improvement project. Emergency Nurse, 27(4).
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



