Addressing the Global Health Challenge of Tuberculosis
Introduction
The global health has the focus on human health problems to understand the type of care needed in the international as well as interdisciplinary context as it has the priority to improve as well as achieve better health and equality healthcare for all the people present worldwide. However, in the current world, the global health challenge is seen to develop a holistic health and well-being platform which provides effective healthcare services for helping the global population lead a healthy as well as an active lifestyle. The most common concerns of health faced globally are the spreading of infectious illness such as HIV, malaria, influenza, tuberculosis and others. In this essay, the global health challenge related to tuberculosis is to be discussed. The prevalence of tuberculosis along with the policies developed to control the illness in Nigeria and in the UK is to be discussed with focus on their statistical health data. A comparison is to be made to identify the reason behind the presence of increased prevalence of tuberculosis in the UK and Nigeria. The partnership approach and the role of the nurses to control tuberculosis in the UK as well as in Nigeria are also to be discussed, with an emphasis on how healthcare dissertation help can provide insights and solutions.

Overview of Tuberculosis
Tuberculosis (TB) is referred as one the serious infectious illness which occurs due to presence of bacteria known as Mycobacterium tuberculosis that damages the lungs of the individuals (Nyang'wa, B.T., Berry et al. 2019). Tuberculosis mainly spreads through the tiny droplets released while coughing and sneezing by the person already affected by the illness. The symptoms of tuberculosis (TB) includes chest pain, high fever, coughing of blood sputum, feeling fatigued, loss of appetite, chills and night sweats (Shete et al. 2015). The presence of HIV makes people prone to get affected by the illness. This is because HIV which is Human Immunodeficiency Virus acts to weaken the immune system of the body making it difficult for the person to resists and fight bacteria which causes TB leading the individual to suffer from the illness (Claassens et al. 2017). The risk factors which lead individuals to be prone to get affected by TB are cancer treatment, travelling to TB infected areas without protection, improper medical care, tobacco use and others (LaCourse et al. 2016). The presence of tuberculosis is found worldwide and the leading countries where it is found are India, China and Nigeria (WHO, 2018).
Tuberculosis in Nigeria
Nigeria is regarded as the third prominent country only after India and China where increased cases of tuberculosis are reported (WHO, 2018). In 2013, nearly 590,000 new cases of the illness are reported in the country and among them 140,000 cases were found to be related with people who already have developed HIV (Omisore et al. 2019). Thus, it indicates that presence of HIV acts as a potential risk factor towards raising the number of people affected by tuberculosis in Nigeria. The reports of 2017 published by WHO informs that 27,000 female within 0-14 years of age and 123,000 females above 14 years of age in Nigeria are affected by tuberculosis (WHO, 2018). The reports also inform that 30,000 males between 0-14 years and 238,000 males who are above the 14 years of age are affected by tuberculosis in Nigeria. It indicates that total of 150,000 females and 268,000 males are affected by tuberculosis in Nigeria (WHO, 2018). This informs that men in Nigeria show greater prevalence compared to females to get affected by tuberculosis. The statistics also informs that 57,000 people within the age of 0-14 years are affected by tuberculosis compared to 361,000 people who are above the age of 14 years (tbfacts.org, 2019; WHO, 2018). This informs that people who are older than 14 years are more prone to get affected by tuberculosis in Nigeria compared to the children.
In 2017, the total cases of tuberculosis notified are 104,904 and out of it, total of 102,387 new cases was reported in the year (WHO, 2018; Avert, 2019). In Nigeria, each year nearly 245,000 people are reported to die from tuberculosis and this figure indicates that 10% of the deaths occurring in the country are due to the presence of the illness. It is also estimated that each hour nearly 30 people in Nigeria die from tuberculosis instead of proper treatment and healthcare services (WHO, 2018). Thus it indicates the prevalence of tuberculosis is at an increased level in the country creating a concerning health situation. The proper and timely diagnosis of tuberculosis is complex because many of the symptoms expressed in the illness are similar to other common illness. Thus, in Nigeria, it is reported that only 16% of the cases of tuberculosis are properly detected and notified to the National Tuberculosis and Leprosy Control Programme (NTBLCP) (WHO, 2019).
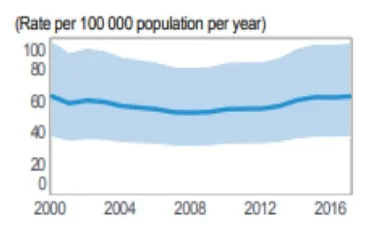
Figure: Prevalence of Tuberculosis

Figure: Mortality rate due to TB

Figure: TB cases as per age and sexual orientation
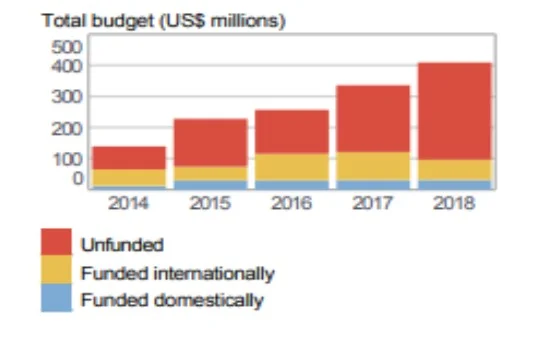
Figure: Funding for TB treatment
The National Tuberculosis and Leprosy Control Program (NTBLCP) was established to coordinate healthcare activities for managing tuberculosis and leprosy in different states within Nigeria so that the prevalence and burden of the illness can be controlled (ntblcp, 2019). The administrative control measure or the workplace policy set by the NTBLCP mentions that a written control and prevention plan for Tuberculosis infection is to be developed at the all Tuberculosis and HIV centres for its proper management (WHO, 2010). This is because written information is able to be properly circulated to all individuals at the workplace and the written data acts as evidential support which can be referred at any time to determine the activities to be executed to prevent and control spread of TB among individuals while working at the centres (Velayutham et al. 2018). The policy also mentions that administrative supports are to be included in processing the plan and quality assurance is to be ensured. Further, the policy mentions that trained staffs are to be allocated to implement the plan successfully within the workplace (Ogbuabor and Onwujekwe, 2019). The DOTS and ART services are to be made available in the facility in true manner so that it can be available by required individuals at the right time to control and prevent the relapse of TB (Ogbuabor and Onwujekwe, 2019; WHO, 2010). The workplace policy set by the NTBLCP mentions the new TB as well as HIV centres to consider different control measures before setting up for providing services to the need (Otu, 2013). This is because without proper prevention initiative to control spread of TB the centres would be unable to act efficiently in controlling the prevalence of the illness.
The environment policy by NTBLCP in Nigeria mentions that to manage spreading and prevention of Tuberculosis all nature of natural ventilation is to be installed as compulsory measures within the rooms and service centres (WHO, 2010). This is because it is regarded as the cheapest way of reducing risk of spreading tuberculosis bacteria. In addition, NTBLCP has mentioned that UGVI is asked to be installed in new healthcare centres where convenient as it acts to kill or inactive the bacteria which causes TB (Singh et al. 2018). The environmental policy also mentions that since UV lights are harmful they are to be installed in the upper part of rooms or exhaust events. Further, the policy mentions that the exhaust and fans are to be cleaned regularly and checked to ensure they are working properly to maintain ventilation so that the illness causes germs are removed from rooms and confined places (WHO, 2010; Mphaphlele et al. 2015).
The personal protection policy is developed by the NTBLCP for managing spread of TB through air or contact with droplets. The policy mentions that procedural masks or surgical masks are to be worn by individuals to prevent the spread of infectious agent of TB (WHO, 2010; Ekuma and Oridota, 2016). This is because the masks allow capturing most of the wet particles and limit droplets to be expelled to the environment during sneezing, coughing or talking (Waheed et al. 2017). Thus, the mask would limit the patients to stop spreading droplets through which new individuals can be infected with TB, in turn, acting to control the spread of the illness. In addition, masks allow the wearer to have proper protection from coming in contact with infectious droplets in the environment which may lead them to develop TB (WHO, 2010). In order to protect the healthcare workers from getting infected by TB, the respirators which are manufactured with 94-95% filter efficiency for 0.3-.04mm participles are to be provided (WHO, 2010). Thus, through effective personal protective measures, the service providers can be protected from getting infected by M.tuberculosis as well as patients would be able to avoid spreading of the illness by releasing droplets in the surroundings (Nardell, 2016).
Continue your exploration of A Three Step Approach to Effective Study Planning with our related content.
In Nigeria, the government has introduced free treatment policy for Tuberculosis in all public facilities and they are based on direct observation treatment, short-course (DOTS) strategy. In this strategy, the patients are required to take medicine under the direct supervision and in front of healthcare workers (copenhagenconsensus, 2015). This strategic policy is useful in controlling TB in Nigeria as the patients take medicine at the proper time without skipping any dose ensuring proper recovery of health. In order to control and prevent TB, National Tuberculosis and Leprosy Control Program (NTBLCP) has developed policy to create awareness regarding the illness among the population through use of television, social media, print media, health promotion and others (stoptb.org, 2019). On World TB Day, the National Tuberculosis and Leprosy Control Program (NTBLCP) hosted awareness program on TB to educate the significance of early diagnosis of the illness and sticking to the care regime suggested by the health practitioners (hfgproject, 2015). In addition, NTBLCP hosts various health promotion campaigns in all areas around Nigeria to aware people regarding the way they can prevent from getting affected by TB and the way care services are to be received to recover from the illness (hfgproject, 2015).
Tuberculosis in the UK
In UK, the data currently published by the Public Health England (PHE) mentions that from 2011 to 2018 a 44% reduction in the new diagnosis of TB was seen and 8.4% fall in diagnosis of TB in the previously affected individual was seen from 2017 to 2018 only. In 2018, 4,655 Tuberculosis cases were reported in England, UK which is 8.3 affected people per 100,000 people (GOC, 2019; tbalert, 2018; Kirby, 2018). The prevalence of TB among the most deprived population in the UK is six times higher compared to the least deprived people. It is also reported that 13% of the individuals affected by TB in England, UK have at least one social factor such as homelessness, substance abuse history or time in prison leading them to suffer from the illness. Nearly, 36% of cases of TB are reported in major cities such as London and 30% of individuals with pulmonary TB in England, UK experiences minimum 4 months delay (tbalert, 2018).
In England, the treatment for Tuberculosis and Latent TB infection is free for all individuals at any level as well as irrespective of immigration status (BLF, 2019). Thus, it provides opportunity to all individuals in the UK to easily access care regarding TB. The NHS England supports raising awareness regarding TB by working with the underserved people with the help of trained professionals. The PHE TB Fingertips tool is being developed by the government in England to help effective monitoring, tracking over time and comparing TB prevention and control performance in different localities. It would be effective to develop actions plans in localities where lower control of TB cases are seen to achieve the goal of effectively lowering TB among people (PHE, 2015). Moreover, in England, UK different Clinical Commissioning Groups (CCGs) are present who commission and plan health services required to control and prevent TB in local areas. They invite and test people for TB as well as encourage the population who have latent TB to take proper treatment facility which is provided free of cost to ensure the illness is resolved (PHE, 2015). The significance of the CCGs is that they provide direct care or arrange proper treatment for individuals suffering TB by personally identifying them from the locality.
Continue your journey with our comprehensive guide to Skills For Interdisciplinary Study.
In the UK, the Tuberculosis Control Boards are developed as a policy to act in preventing TB prevalence in England by the government. The Board acts to support and improve the TB clinical frameworks, execute gap-analysis for local services, support underserved population and work with local laboratories to improve diagnosis of TB (NHS, 2015; assets.publishing.service.gov.uk, 2019). They are effective to provide effective support to the local individuals in the areas to be aware and avail proper services to act in controlling TB. In the UK, TB Clinical Teams are recruited as a policy to increase awareness regarding the illness among healthcare providers to make them more focussed on providing improved services to ensure better health condition of individuals. The Clinical Teams also discuss all forms of multi-drug resistant TB cases with the British Thoracic Society to develop arrangements and plans to control them (NICE, 2019). In the UK, the vaccination policy is used for preventing spread of Tuberculosis (TB). The BCG vaccine which is manufactured in Denmark by the AJ Vaccines is used to vaccinate children who are living in highly affected TB infested areas, had family history of TB and/or in close contact with TB patients to protect them from getting affected by the illness (NHS, 2019a). It is informed that the BCG vaccine is effective in 70-80% of cases of TB to prevent the person from getting affected by the illness. However, the vaccine is mentioned by the UK government not to be taken by people who are already affected by TB as it would create negative impact on their health (vk.ovg.ox.ac.uk, 2019).
Analysing presence of increased Tuberculosis in Nigeria compared to the UK
The statistical comparison regarding the prevalence of Tuberculosis (TB) between Nigeria and the UK mentions that there are more people in Nigeria who are affected by TB compared to the UK. There are different reason behind increased prevalence of TB in Nigeria compared to the UK one of which is the presence of myths and misconceptions regarding the illness among the population in Nigeria. In Nigeria, the population believe that TB is caused due to ingestion of cat hair, cold air, eating together, witchcraft and it is heredity which makes the illness unable to be cured through medical treatment. It requires use of ashes, brunt garlic and oils along with other common ingredients that are infested with magic to resolve the illness (Balogun et al. 2015; Obembe et al. 2017; Anochie et al. 2013). However, in England, UK Tuberculosis is regarded as medical condition by the individuals and they try to seek proper healthcare and medicine to ensure recovery from the illness (Abbara et al. 2017). Thus, the presence of the misconceptions among the Nigerian people makes them avoid to access proper healthcare to resolve the illness, in turn, raising the prevalence of the TB in the country.
Take a deeper dive into The Healthy Settings Approach with our additional resources.
In Nigeria, it is seen that TB is regarded as a shame as individuals with the illness are seen to be isolated and avoided to be interacted socially (Bieh et al. 2017). Thus, the perception of considering TB as a shameful illness in the society of Nigeria is increasing its prevalence at a massive rate in the country. This is because many individuals out of shame and fear of isolation avoid receiving proper healthcare as it would expose them in society. However, in the UK no such isolation or shame in the society is faced by individuals suffering from Tuberculosis as it is regarded as a disease which can be cured through proper intervention. The acceptance is brought through effective awareness campaigns by healthcare organisations in the UK (thetruthabouttb, 2019). The presence of increased number of defaulters who have stopped taking medicine midway has resulted increased presence of TB in Nigeria compared to the UK.
The increased number of defaulters in TB treatment in Nigeria is seen because of lack of proper access to care centres, increased treatment duration and hindrance in taking medicine (Ukwaja et al. 2013; Adejumo et al. 2017). However, in the UK it is seen that the NHS England along with the government has developed various CCGs in local areas, Clinical teams who monitor and provide health care to TB affected individuals in locality and increased number of health centres in rural areas of the country (GOV, 2016). It has led them to develop well-maintained systems which ensure no defaulters of TB treatment are present in any area ensuring better control of the illness in the country. In Nigeria, there is no proper Board or team of health professionals to detect cases of Tuberculosis in different areas. This is evident from the study of Ahmad et al. (2018) where it is mentioned that poor case detection along with poor notification regarding tuberculosis among the population in Nigeria is raising the incidence and mortality related to the illness. However, in England, a separate Tuberculosis Control Boards are seen to be established who are provided the task to detect cases of TB along with arrange services for the individuals to properly control the prevalence of the illness in any area (GOV, 2016).

The increased household cost to be borne by members due to treatment regarding TB is leading many individuals in Nigeria to avoid accessing care for TB. This is evident as even though medical care is provided free of cost yet the families in Nigeria report that the cost of the overall care of the patient at the home is quite high which often makes them borrow money by selling their assets (Ukwaja et al. 2013). According to international economic condition, it is seen that Nigeria is poor country where many of the people live in low socio-economic condition compared to the UK. Thus, the lower economic status of the Nigerian people which makes them face hindrance to bear cost of entire care of people affected by TB is leading the country to experience increased presence of TB. In addition, in the UK there are many advanced healthcare services as well as treatment available for resolving TB compared to Nigeria (assets.publishing.service.gov.uk, 2019). Thus, the presence of better facility of healthcare services for controlling TB in the UK is leading the illness to be remained in control in the country in a better way compared to Nigeria.
Evaluating collaborative partnership to tackle Tuberculosis inequalities across people of different culture and beliefs as well as age
The collaborative partnership is referred to the agreements which are developed between consenting organisations for sharing resources such as finances, human resource and knowledge for accomplishing a common goal (Zumla et al. 2015). The presence of collaborative partnership is beneficial because it allows improved teamwork as various professionals with wide experiences from different organisation works together to develop effective ideas in resolving healthcare problems (Lienhardt et al. 2018). This indicates that collaborative partnership is essential to tackle TB inequalities across people because it is going to allow the inclusion of wide amount of ideas and assistance from various experienced professionals of different organisations who belong from different culture. The professionals would act together to resolve inequalities related to TB across different ages and cultures of people as they have the idea which way communication is to be made among different age groups and culture to make the people access proper treatment for TB. The collaborative partnership helps in reducing communication gaps as professionals from different areas of various organisation works together (Surette et al. 2017). Thus, collaborative partnership is essential for tackling TB inequalities as it would include different organisation from various parts of the society to act together for understanding the inequalities they are to resolve to improve communication and awareness regarding the illness among the population.
Analysing role of nurses to manage people with Tuberculosis in the UK and Nigeria
The key role of the nurse in managing people with Tuberculosis in UK and Nigeria is to monitor health and activities of the patients, provide patient care, offer health education, collect sputum, screen patients, identify any side-effects of medicine and others. The regular monitoring of the patient’s health progress and their activities in Tuberculosis treatment is to be made by the nurses so that they can assess the progress of health condition of the individual and if the person is following proper rules and taking medication as suggested (de Vries et al. 2017). Thus, the continuous monitoring would help the nurses to understand the health progress of the patients as well as the further actions to be taken to resolve the illness in the patient.
The offering of health education regarding TB is role of nurses where they inform regarding the cause of TB, way to prevent its transmission, usefulness of medicines provided and consequences of not following treatment to the patient (Coelho et al. 2016). This is required to make the patients remain aware regarding the way they are to act to resolve the raised health issues and avoid spread of the infectious disease to others. The nurses are to collect sputum of patients with TB to send it for diagnosis to identify and report the health condition of the patient to the health professional who would suggest proper treatment for the patients (Nathavitharana et al. 2017). The nurses also have the role in Tuberculosis management to pay home visits to the people affected by TB (Daftary and Padayatchi, 2016). This is because it would make them understand whether the care procedure suggested is properly followed by the patient or not as well as the health condition of the patient or any hindrances faced by the patient which is causing the individual to discontinue treatment.
Conclusion
The above discussion mentions that Tuberculosis is one of the global health challenges being faced by many people. Tuberculosis (TB) is an infectious disease which is spread through Mycobacterium tuberculosis. Nigeria is third after India and China with high prevalence of TB where each hour 30 individuals die due to the illness. In England, UK the prevalence of TB is low which is evident as in 2018 only 4,655 cases were reported. However, in Nigeria, 57,000 people within the age of 0-14 years are affected by tuberculosis compared to 361,000 people who are above the age of 14 years as per reports in 2017. The environment, workplace and personal safety policies are set by the National Tuberculosis and Leprosy Control Program (NTBLCP) in Nigeria to control TB. In England, UK policies for management of TB include arrangement of CCGs, development of TB Control Bora and Teams and others. The prevalence of TB is more in Nigeria compared to UK because there are many misconceptions regarding TB as well as many people avoid accessing full course of care for TB. The role of nurses in Nigeria and the UK to tackle TB include providing patient care, monitoring health and activities of the patients, offering health education and others.
References
Abbara, A., Chitty, S., Roe, J.K., Ghani, R., Collin, S.M., Ritchie, A., Kon, O.M., Dzvova, J., Davidson, H., Edwards, T.E. and Hateley, C., 2017. Drug-induced liver injury from antituberculous treatment: a retrospective study from a large TB centre in the UK. BMC infectious diseases, 17(1), p.231.
Adejumo, O.A., Daniel, O.J., Otesanya, A.F., Salisu-Olatunj, S.O. and Abdur-Razzaq, H.A., 2017. Evaluation of outcomes of tuberculosis management in private for profit and private-not-for profit directly observed treatment short course facilities in Lagos State, Nigeria. Nigerian medical journal: journal of the Nigeria Medical Association, 58(1), p.44.
Ahmad, N.M., Montañola-Sales, C., Prats, C., Musa, M., López, D. and Casanovas-Garcia, J., 2018. Analyzing policymaking for tuberculosis control in Nigeria. Complexity, 2018. pp.19-29.
Anochie, P.I., Onyeneke, E.C., Onyeozirila, A.C., Igbolekwu, L.C., Onyeneke, B.C. and Ogu, A.C., 2013. Evaluation of public awareness and attitude to pulmonary tuberculosis in a Nigerian rural community. Germs, 3(2), p.52.
assets.publishing.service.gov.uk 2019, Tackling Tuberculosis in Under-Served Populations, Available
Balogun, M., Sekoni, A., Meloni, S.T., Odukoya, O., Onajole, A., Longe-Peters, O., Ogunsola, F. and Kanki, P.J., 2015. Trained community volunteers improve tuberculosis knowledge and attitudes among adults in a periurban community in southwest Nigeria. The American journal of tropical medicine and hygiene, 92(3), pp.625-632.
Bieh, K.L., Weigel, R. and Smith, H., 2017. Hospitalized care for MDR-TB in Port Harcourt, Nigeria: a qualitative study. BMC infectious diseases, 17(1), p.50.
BLF 2019, How is TB treated?, Available at:
Claassens, M.M., Van Schalkwyk, C., Floyd, S., Ayles, H. and Beyers, N., 2017. Symptom screening rules to identify active pulmonary tuberculosis: Findings from the Zambian South African Tuberculosis and HIV/AIDS Reduction (ZAMSTAR) trial prevalence surveys. PloS one, 12(3), p.e0172881.
Coelho, A.P.C., Larocca, L.M., Chaves, M.M.N., Felix, J.V.C., Bernardino, E. and Alessi, S.M., 2016. Healthcare management of tuberculosis: integrating a teaching hospital into Primary Health Care. Texto & Contexto-Enfermagem, 25(2). pp.78-90.
Daftary, A. and Padayatchi, N., 2016. Provider perspectives on drug-resistant tuberculosis and human immunodeficiency virus care in South Africa: a qualitative case study. The International Journal of Tuberculosis and Lung Disease, 20(11), pp.1483-1488.
Ekuma, A.E. and Oridota, E.S., 2016. Knowledge, attitude and tuberculosis infection control practice among healthcare workers in DOTS centres in Lagos, Nigeria. Int J Inf Con, 12(4), pp.1-9.
Kirby, T., 2018. Tuberculosis incidence in England hits 30-year low. The Lancet Respiratory Medicine, 6(10), p.744.
Lienhardt, C., Zumla, A., Gebreselassie, N., Frick, M., Gray, G., Kasaeva, T. and Raviglione, M., 2018. Tuberculosis research and development: seeding the future. The Lancet Respiratory Medicine, 6(4), pp.242-244.
Merker, M., Blin, C., Mona, S., Duforet-Frebourg, N., Lecher, S., Willery, E., Blum, M.G., Rüsch-Gerdes, S., Mokrousov, I., Aleksic, E. and Allix-Béguec, C., 2015. Evolutionary history and global spread of the Mycobacterium tuberculosis Beijing lineage. Nature genetics, 47(3), p.242.
Mphaphlele, M., Dharmadhikari, A.S., Jensen, P.A., Rudnick, S.N., Van Reenen, T.H., Pagano, M.A., Leuschner, W., Sears, T.A., Milonova, S.P., van der Walt, M. and Stoltz, A.C., 2015. Institutional Tuberculosis Transmission. Controlled trial of upper room ultraviolet air disinfection: a basis for new dosing guidelines. American journal of respiratory and critical care medicine, 192(4), pp.477-484.
Nardell, E.A., 2016. Transmission and institutional infection control of tuberculosis. Cold Spring Harbor perspectives in medicine, 6(2), p.a018192.
Singh, T., Ngcobo, Z., Kgasha, O., Leuschner, W., Matuka, O., van Reenen, T. and De Jager, P., 2018. Efficacy assessment of ultraviolet germicidal irradiation (UVGI) devices for inactivating airborne Mycobacterium tuberculosis. Occupational Health Southern Africa, 24(4), pp.92-100.
stoptb.org 2015, NIGERIA STOP TB PARTNERSHIP STRATEGIC PLAN 2013-2015, Available
The infection mainly initiates when the mycobacteria reach the alveolar sacs of the lungs where they are found to invade as well as replicate endosomes of alveolar macrophages. The bacterium is identified as foreign body by the macrophages and they try to eliminate them through the process of phagocytosis in which the bacteria is temporarily stored within the macrophage bounded by a vesicle known as phagosome (Orgeur and Brosch, 2018). In the phagolysosome, the cell by trying to use reactive oxygen species intends to kill the bacteria. However, in M.tuberculosis it is seen that they are covered by a thick membrane with the waxy mycolic acid capsule which protects it from getting destroyed. The M.tuvberculosis in the protection of its thick capsule then tries to reproduce through binary fission inside the macrophage to eventually kill immune cells of the body (Merker et al. 2015).
Continue your journey with our comprehensive guide to Addressing Public Nuisances.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



