Tackling the Growing Epidemic
Introduction
Obesity is the medical condition in which excessive fat accumulates in the body that adversely impacts on the health of the individuals (Kyle et al. 2017). In 2017, the government of Scotland informed that 29% of adults are obese along with 13% of children of 2-15 years of age are obese (gov.scot, 2017, gov.scot, 2017a). According to world statistics, it is reported that 30% of the total population worldwide are suffering from obesity (WHO, 2020). These statistics revealed that quite high number of people in Scotland and in the world is affected by obesity making it one of the key contemporary health issues to be analysed. For students tackling such health issues in their research, seeking healthcare dissertation help can provide valuable guidance. According to prediction, by 2030, 40% adults are to be affected by obesity in Scotland (gov.scot, 2018). This indicates that in coming years the health issue of obesity for population in Scotland is going to be grave due to which effective discussion regarding the contemporary health topic is needed.

Dimension of Health
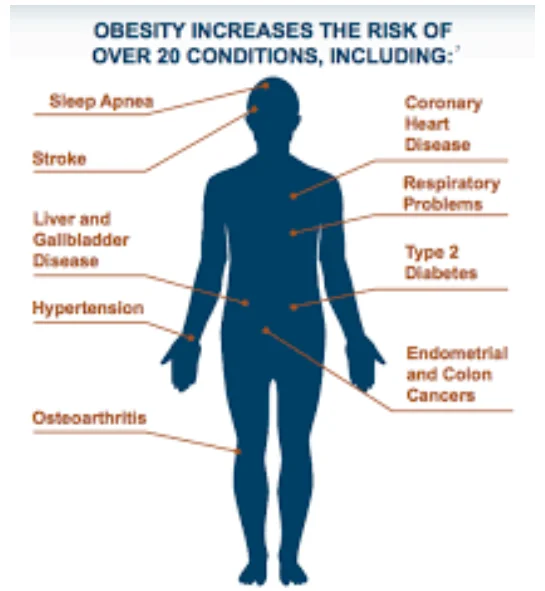
The five dimensions of health are emotional, physical, spiritual, social and intellectual well-being that are interrelated to influence the health of individuals (Shiloh and Nudelman, 2020). Each of the five dimensions of health is important to ensure holistic care as their consideration by health professionals and individuals makes them aware of the aspects to be followed for maintaining overall improvement and management of optimal health to lead a healthy life (Linton et al. 2016). The physical health dimension is effective functioning of the body where each organ works in perfect harmony (Sharp et al. 2019). In case of obesity, the physical dimension of health is disrupted as excess body fat accumulation creates imbalance between the endothelium-derived vasoactive factors. The hindered regulation of these factors because of endothelial cell dysfunction raises vascular resistance of the body adversely affecting the working efficiency of the heart to pump proper amount of body, in turn, raising the blood pressure as well as raise risk of cardiovascular diseases (Osanai et al. 2017). The emotional health dimension is proper balance between the body and psychological condition (Yufe et al. 2017). The people suffering from obesity are often stigmatised and bullied for their appearance in the society that adversely affects the emotional health of the individuals to develop depression and anxiety (Rankin et al. 2016).
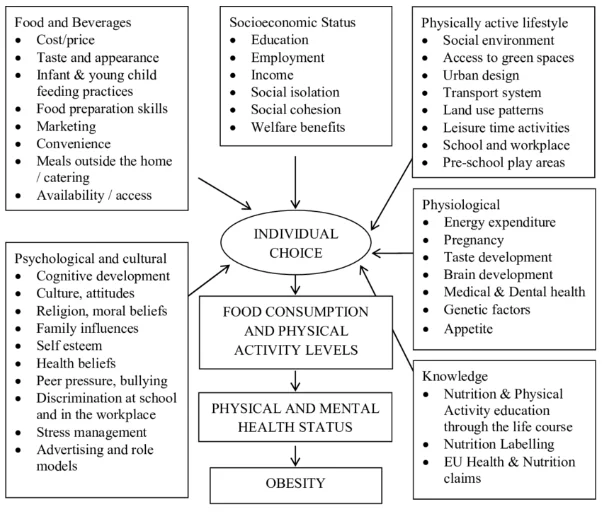
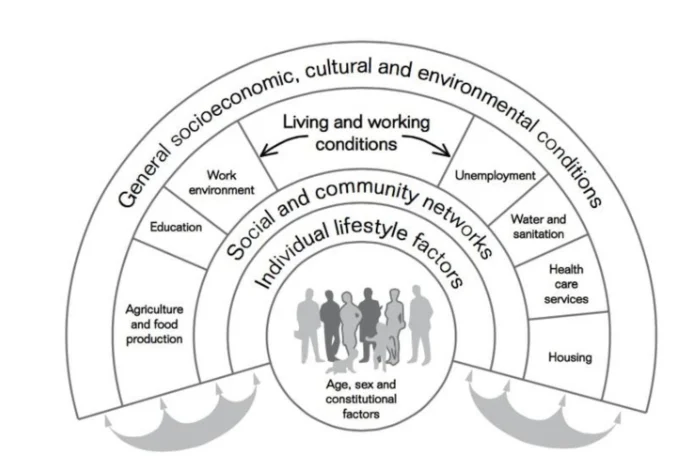
Determinants of health
The Dahlgren and Whitehead’s rainbow model is referred to the systematic framework which mentions individuals to be present at the centre and they are surrounded by various layers of health determinants (Rice and Sara, 2019). According to the model, health determinants like living condition, healthcare services, age, genetics, physical activity, food and others impact a broad range of health functioning and quality-of-life outcomes among individuals in an unequal way. This is because there are varied differences in the genetic arrangement, living condition, income ability and others among people that positively and negatively influence the way they live and ensure well-being in the society (Bonner, 2017).
Looking for further insights on The Growing Epidemic? Click here.
According to the model, one of the health determinants that influence the rise of obesity is level of education. This is because without health education the people suffering from obesity are unable to determine risk of the disease as well as the extent to which their current activities are creating progress in obesity (Ogden et al. 2017). As argued by Ward et al. (2017), lack of proper health education and awareness regarding the cause and impact of obesity leads the people remain insincere to make changes in their everyday lifestyle. This negatively influences their health and well-being. For instance, in the Scotland, there is 20% more prevalence of obesity found among the children in the most deprived areas compared to people in the least deprived areas. This is because the children and parents in least deprived areas can access proper health awareness programs and campaigns regarding obesity as well as are properly educated to understand the causes and risk of obesity. This is in comparison to people in most deprived areas where there is low level of education and healthcare services to develop proper activities by parents to help their children avoid being obese (scotpho.org.uk, 2017b).
The variation in genetic framework among the individuals influences their health raising changes of inequality (Loos and Janssens, 2017). In the study by Goodarzi (2018), it is mentioned that rarely inheritance of genetic pattern that is caused by alteration in single gene leads to obesity that is known as monogenetic obesity. This is mainly caused by continuous mutation in a single gene in the body that is related to control food intake and management of appetite. Since these natures of genetic alteration are not common, therefore health inequality in relation to genetic expression of obesity is seen among people. The presence of employment is seen to create health inequality regarding obesity. This is because unemployed people are prone to live a sedentary lifestyle with less physical activity. It leads them unable to use fats from the food as energy which results the fats to get deposition and stored in the body raising overall weight causing obesity (Bramming et al. 2018). It is evident from the study of Monsivais et al. (2015), where 1.56kg/year weight again among unemployed people are informed compared to 0.60kg/years among employed people in Britain mentioning the unemployed people to be at increased risk of obesity.
Factors influencing healthcare
The external factors like economic condition influence healthcare delivery as without proper availability of finances effective health promotion and services regarding any disease cannot be provided to ensure good health condition (Kaur, 2016). In contrast, the lack of proper legal and political condition in the country leads to development of hindered rules and regulations in management of health condition and delivery of healthcare services. This causes health professionals unable to organise proper healthcare to take stringent action in controlling any health issue for the public (Bleich et al. 2018).
The internal factors such as social stigma regarding any form of health issue or healthcare impact individuals to avoid exposing their health issues or receive care as they feel exposure of the condition would lead them to discriminated as well as harmed and abused in the society. It leads to hinder reach of healthcare services to all individuals suffering from the disease as they are unable to be identified to be offered care (Pont et al. 2017). In certain marginalised and ethnic groups, it is found that they have hindered perception regarding health that is supported by their custom and beliefs. In this condition, proper healthcare is unable to reach them out of their stringent action to avoid following actions out of the custom which is equal to disrespecting their beliefs (Yetti et al. 2018).
The presence of legal policies on unhealthy foods can reduce risk of obesity to some extent. For example, increased intake of sugary drinks leads to add increased amount of calorie in the body as it gets stored in the form of fat which eventually raises the weight of the body to make the person develop gradual obesity (Shearrer et al. 2018). Thus, the UK government is seen to have imposed sugar tax where 24p is charged for 8g of sugar/100 ml and 18p for 5-8 g sugar/100ml (heraldscotland.com, 2018). This is done with the intention to make food companies lower among of sugar in their manufactured products which would in turn impact to take action in lowering the risk of obesity among the UK population.
In relation to economic factors, it is found that nearly 8.4% of the healthcare costs in OCED countries are used for obesity management (weforum.org, 2019). The NHS, Scotland has spent nearly £3.6-6.1 billion for controlling obesity and overweight issues in 2016 (obesityactionscotland.org, 2016). This indicates that huge economic expenditure is being made for obesity management around the world as well as in Scotland indicating it to be a costly health issue to be managed by the government. The stigma regarding obesity and weight-based discrimination has increased risk of psychological distress among obese individuals. This has led physical as well as mental healthcare support to be arranged for obese individuals to ensure their good health (Bombak et al. 2016).
Partnership working, person-centred care and user carer inclusion
In health and social care, NMC Code of Practice informs that partnership working to manage healthcare are to be formed with inclusion of colleagues, patients and their families, health professionals and others to collaboratively take actions in controlling any health issues (NMC, 2018). This is effectively used for obesity management in the Scotland as partnership with patients, health professionals and others lead to gather resources, arrange expert knowledge and skills along with sharing power to deliver proper healthcare services in managing obesity (NHS, 2018). As argued by Bagnall et al. (2019), lack of partnership working lead lack of involvement of diverse ideas and create hindrance in taking proper decision through discussion for effectively resolving any health issue. This indicates that partnership working helps to resolve health issues in effective manner.
In the Scotland, partnership between local communities, primary healthcare providers, local community organisations and local business are developed under the National Institute for Health Excellence (NICE) guidance for obesity management to control prevalence of obesity (NICE, 2014). This is because partnership has led to share the responsibilities of creating awareness and delivery of healthcare regarding obesity control among the population. Moreover, it has led to control nature of foods to be sold in the local areas to ensure healthy eating is promoted among the population to avoid obesity raise from intake of unhealthy and fatty foods. In the NHS, Scotland, it is seen that multidisciplinary team that includes dietician, health professional, nurses and others are set to control and management obesity (healthscotland.scot, 2018c). This is because dieticians inform regarding diet charts to be followed whereas health professionals inform medication and intervention to be availed by people suffering from obesity to ensure each individual with obesity can access holistic care.
The carer user involvement is required for management obesity as it helps the carer understand which intervention are preferred by the users to help them overcome and manage obesity with satisfactory care (Hammersley et al. 2016). This is important as shared decision making in obesity management leads to greater compliance in care by users helping the carer to act smoothly in controlling the disease. The NMC Code of Practice mentions that person-centred care is to be offered to individuals by considering their specific needs and demands to ensure greater health improvement (NMC, 2018). This is because based on health condition regarding obesity there are varied needs present among individuals which are not always similar. Thus, offering person-centred care would help nurses to take specific course of action that is most effective for obese individuals in managing their condition with better efficiency.
Health improvement
Health promotion is referred to public policy taken to address different health determinants to allow people develop improved control over managing their health issues and well-being (WHO, 2018). The World Health Organisation (WHO) informs that for obesity management effective promotion of performing physical exercise among people of all ages is to be made. This is because physical exercise helps the body to burn extra fat and use increased calories taken in with food as energy avoiding them to be stored as fat and contribute to weight gain that results in obesity (WHO, 2018). The WHO mentions under Obesity Management promotion informs that healthy eating is to be promoted among people through proper delivery of health education (). This is because unhealthy food intake along with overeating is found to key cause of increased addition of fat in the body that leads towards obesity in the individuals (WHO, 2018).
In 2018, NHS Scotland to tackle obesity have develop the Diet and Healthy Weight Delivery Plan under which the key goals to be attained are promoting healthy eating among children, arranging food environment that offers healthier choices, allow people easy access to weight management, promote healthy weight and reduce diet-related health inequality (healthscotland.scot, 2018). There is still no existing evaluation made to judge the success of the plan. At the local level, the NHS Greater Glasgow and Clyde (NHS GGC) have developed obesity prevention strategy to promote the health of the individuals regarding the disease. The strategies include establishment of nutritional meal standards for school, running projects to improve physical activity and healthy eating in the area, offer NHS services to adult and elderly obese people and encourage food industries for labelling nutrition content on their products (NHSGGC, 2018). These are effective strategies and healthy eating and physical activity would avoid addition of unhealthy weight along with proper healthcare services for obese patients would make them control their health regarding obesity.

Conclusion
The above discussion informs that obesity is highly prevalent among all age groups in the Scotland as well as globally and it is going to increase in the comming years. Thus, active steps for its control are required to be taken to lower its prevalence. In this respect, the determinant and dimensions of health are to be considered to understand the influence of the disease. The assistance of the NHS Scotland along with NHS GGC and WHO are to be taken for effective promotion of obesity management in the UK.
Continue your exploration of Tackling Air Pollution with our related content.
References
Bagnall, A.M., Radley, D., Jones, R., Gately, P., Nobles, J., Van Dijk, M., Blackshaw, J., Montel, S. and Sahota, P., 2019. Whole systems approaches to obesity and other complex public health challenges: a systematic review. BMC Public Health, 19(1), p.8.
Bleich, S.N., Jones-Smith, J.C., Walters, H.J. and Rutkow, L., (2018). The Voices for Healthy Kids and state legislation to prevent childhood obesity: an update. American journal of preventive medicine, 54(6), pp.821-824.
Bombak, A.E., McPhail, D. and Ward, P., (2016). Reproducing stigma: Interpreting “overweight” and “obese” women's experiences of weight-based discrimination in reproductive healthcare. Social Science & Medicine, 166, pp.94-101.
Bonner, A. ed., (2017). Social determinants of health: An interdisciplinary approach to social inequality and wellbeing. Policy Press.
Bramming, M., Jørgensen, M.B., Christensen, A.I., Tolstrup, J.S. and Lau, C.J., (2018). Obesity and labor market participation: a prospective cohort study of transitions between work, unemployment and sickness absence. Revue d'Épidémiologie et de Santé Publique, 66, p.S265.
Goodarzi, M.O., (2018). Genetics of obesity: what genetic association studies have taught us about the biology of obesity and its complications. The Lancet Diabetes & Endocrinology, 6(3), pp.223-236.
Hammersley, M.L., Jones, R.A. and Okely, A.D., (2016). Parent-focused childhood and adolescent overweight and obesity eHealth interventions: a systematic review and meta-analysis. Journal of medical Internet research, 18(7), p.e203.
Kaur, A., (2016). Impact of Economic Condition on Obesity. American Journal of Health Research, 4(6-2), pp.1-4.
Kyle, R.G., Wills, J., Mahoney, C., Hoyle, L., Kelly, M. and Atherton, I.M., (2017). Obesity prevalence among healthcare professionals in England: a cross-sectional study using the Health Survey for England. BMJ open, 7(12), p.e018498.
Linton, M.J., Dieppe, P. and Medina-Lara, A., (2016) Review of 99 self-report measures for assessing well-being in adults: exploring dimensions of well-being and developments over time. BMJ open, 6(7), p.e010641.
Loos, R.J. and Janssens, A.C.J., (2017). Predicting polygenic obesity using genetic information. Cell metabolism, 25(3), pp.535-543.
Monsivais, P., Martin, A., Suhrcke, M., Forouhi, N.G. and Wareham, N.J., (2015). Job-loss and weight gain in British adults: Evidence from two longitudinal studies. Social science & medicine, 143, pp.223-231.
Ogden, C.L., Fakhouri, T.H., Carroll, M.D., Hales, C.M., Fryar, C.D., Li, X. and Freedman, D.S., (2017). Prevalence of obesity among adults, by household income and education—United States, 2011–2014. MMWR. Morbidity and mortality weekly report, 66(50), p.1369.
Osanai, T., Mikami, K., Kitajima, M., Urushizaka, M., Kawasaki, K., Tomisawa, T., Itaki, C., Noto, Y., Magota, K. and Tomita, H., (2017). Nutritional regulation of coupling factor 6, a novel vasoactive and proatherogenic peptide. Nutrition, 37, pp.74-78.
Pont, S.J., Puhl, R., Cook, S.R. and Slusser, W., (2017). Stigma experienced by children and adolescents with obesity. Pediatrics, 140(6), p.e20173034.
Rankin, J., Matthews, L., Cobley, S., Han, A., Sanders, R., Wiltshire, H.D. and Baker, J.S., (2016). Psychological consequences of childhood obesity: psychiatric comorbidity and prevention. Adolescent health, medicine and therapeutics, 7, p.125.
Rice, L. and Sara, R., (2019). Updating the determinants of health model in the Information Age. Health promotion international, 34(6), pp.1241-1249.
Sharp, M.L., Busuttil, W. and Murphy, D., (2019). Examining physical health conditions and associations of pain, obesity, and function of UK Veterans diagnosed with PTSD and other mental health conditions. Journal of Military, Veteran and Family Health, 5(2), pp.75-87.
Shearrer, G.E., Stice, E. and Burger, K.S., (2018). Adolescents at high risk of obesity show greater striatal response to increased sugar content in milkshakes. The American journal of clinical nutrition, 107(6), pp.859-866.
Shiloh, S. and Nudelman, G., (2020). Exploring dimensions of health behaviors’ representations. Psychology & Health, pp.1-16.
Ward, D.S., Welker, E., Choate, A., Henderson, K.E., Lott, M., Tovar, A., Wilson, A. and Sallis, J.F., (2017). Strength of obesity prevention interventions in early care and education settings: a systematic review. Preventive Medicine, 95, pp. S37-S52.
Yetti, R.E., Safar, M., Zulkifli, A., Indriasari, R., Tombeg, Z., Manggabarani, S. and Hadi, A.J., (2018). The association between eat culture and obesity among adolescents in tana toraja. Indian Journal of Public Health Research & Development, 9(11), pp.502-507.
Yufe, S.J., Taube-Schiff, M., Fergus, K.D. and Sockalingam, S., (2017). Weight-based bullying and compromised peer relationships in young adult bariatric patients. Journal of health psychology, 22(8), pp.1046-1055.
Bibliography
Hruby, A., Manson, J.E., Qi, L., Malik, V.S., Rimm, E.B., Sun, Q., Willett, W.C. and Hu, F.B., 2016. Determinants and consequences of obesity. American journal of public health, 106(9), pp.1656-1662.
Kilov, D. and Kilov, G., 2018. Philosophical determinants of obesity as a disease. Obesity Reviews, 19(1), pp.41-48.
Rice, L. and Sara, R., 2019. Updating the determinants of health model in the Information Age. Health promotion international, 34(6), pp.1241-1249.
Walls, H., Baker, P. and Parkhurst, J., 2018. Addressing trade policy as a macro-structural determinant of health: The role of institutions and ideas. Global social policy, 18(1), pp.94-101.
Torkamani, A. and Topol, E., 2019. Polygenic risk scores expand to obesity. Cell, 177(3), pp.518-520.
Appendix
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



