Vaccination Policy Briefing
Executive Summary
Due to widespread immunization, the UK has managed to control certain diseases with devastating health effects such as measles, pertussis, smallpox and polio. Consequently, public health experts have commended vaccines as one of the most significant public health achievements in the history of mankind. Nonetheless, despite the witnessed success of vaccines and a plethora of scientific evidence revealing their effectiveness in disease control, sceptics have spread misconceptions about vaccines, derailing the potential success of immunization as a public health initiative. To promote public confidence and improve uptake of vaccines and save lives, public health authorities and practitioners should evaluate the efficacy and safety of vaccines in relation to commonly held misconceptions. For a comprehensive approach, integrating insights from healthcare dissertation help can be valuable. More importantly, the authorities should promote transparency, while maintaining clear and participatory communication with the general public.

Introduction
The role of vaccines in the maintenance of health and well-being of people can never be overemphasized. Ehreth (2003) estimates that yearly, vaccines help prevent the death of at least 6 million people globally. They train the body’s immune system to detect more quickly, disease causing germs, thus preventing people from diseases. Iwasaki & Omer (2020) explained that vaccines work by imitating infections, but such infections do not cause illness unlike that acquired from an actual infection. Rather, the vaccine introduces a substance in the body that triggers the immune system to produce disease-fighting antibodies and blood cells that protects the body from the vaccinated disease for years.
While not all diseases that can be prevented through a vaccine seem serious, preventable infections such as the COVID-19 have serious health implications and have led to many deaths globally (Corrondo & Moita, 2020). On the other hand, common diseases such as influenza may be perceived as seasonal illnesses that are ‘mundane’ in nature, but it might be lethal to populations with weaker immune system such as children and older adults.
While some COVID-19 vaccines (e.g. Pfizer-BioNTech and Moderna) have been developed and approved for emergency use in countries such as the UK and the USA, some pharmaceutical companies and research institutes around the world are still working on safer and more effective COVID-19 vaccines (Lurie et al, 2020). Peiris & leung (2020) estimated that by mid-2021, more vaccines will be out for public use, while others (e.g. Carrondo & Moita, 2020) speculating that the entire process might take several years. That said, the availability of COVID-19 will have several policy implications beyond just changing the currently imposed public health policies such as restrictive curfews. The main aim of this policy brief paper is to:
- Highlight the benefits of widespread vaccination
- Identify some of the myths and misconceptions held by sceptics against vaccines
- Identify ethical principles upon which the vaccine rollout should be based
- To make policy recommendations on the most effective ways to roll out mass immunization programs for new vaccines. In the process, the report will refer to the newly developed COVID-19 vaccines.
Vaccine as a source of Herd immunity
Apart from protecting vaccinated individuals from preventable diseases, vaccines will protect communities from the disease through herd immunity. According to Fontanet & Cauchemez (2020), herd immunity is achieved through a mass immunization of most of the community, protecting the unvaccinated minority from the disease. It occurs because the disease is unable to advance when only a few individuals are vulnerable (Britton et al, 2020). Against this backdrop, the required rate of vaccination needed to achieve heard immunity can only be determined by the transmissibility of the disease. While most diseases require a vaccination rate of 80-90% to facilitate herd immunity, other highly contagious diseases (e.g. COVID-19) require 90-95% of vaccination coverage (Lipsitch et al, 2020).
Herd immunity also helps to protect individuals who cannot be fully vaccinated by merely receiving a vaccine. According to Britton et al (2020), this group might include the new-borns, pregnant women, the immunocompromised and the elderly. Ideally, such people can only be protected when there is a high immunization rate within the communities, they live in. They, therefore, form part of a vulnerable population, and may include those with immune supressing infections (e.g. organ transplant patients), or those with suppressed immunity as a result of therapy (Lipsitch et al, 2020).
Vaccine as a cost-effective health intervention
Preventable disease such as COVID-19 have caused serious economic burden not only in the UK but also in the world over. For example, according to Cantore et al (2020), COVID-19 has caused a global economic crisis by disrupting important economic activities manufacturing and production. UNIDO’s global statistics on average percentage loss of industrial production as a result of the COVID-19 pandemic indicate an average 18% loss of industrial production in the top 30 high income countries in the world, while upper-middle income countries are estimated to have lost 24% of their industrial production. Similar statistics also indicate that lower-middle income countries have lost 22% of their industrial production (Cantore et al, 2020).
The health burden of such diseases, from a cost perspective, has also gone high both in the UK and world over. For instance, in 2019 after the COVID-19 outbreak, UK’s cumulatively available bed capacity in acute care hospitals, mental health facilities and maternity hospitals recorded a new low of 127,225 since 1988 (National Health Service, 2020). Furthermore, over the period between 1988 and 2019, the UK’s health system recorded the highest number of hospital admissions by NHS, indicating the significant resource pressures experience by NHS hospitals as a result of COVID-19. Ideally, since the start of the pandemic, there has been a 34% reduction in bed availability including the beds available for long-term adult care (National Health Service, 2020).
In response to the decreasing rate of hospital bed availability (triggered by COVID-19), the UK government has since incurred more costs in building the so-called Nightingale hospitals – which are temporary hospitals meant to meet the hospital bed demands created by the pandemic (Ewbank et al, 2020). Latest data show that as a result of the construction of Nightingale hospitals, the critical bed capacity in the UK has increased by at least 3600 beds (Flynn et al, 2020). These response mechanisms have done nothing less that increasing the resources spent by the UK’s health system in response to the pandemic.
Through immunization, UK’s health system stands to spend way less that they currently spend on managing the pandemic. According to Flynn et al (2020), the COVID-19 vaccine, for example, will prevent further infections, leading to a reduced number of people in need of hospitalization. Consequently, the health system will not spend much on makeshift hospitals or other rapid response strategies that they currently must finance. This highlights the importance of mass vaccination of the UK public against preventable diseases such as COVID-19.
Vaccines have proven tremendous success with other preventable diseases such as measles, pertussis, polio, hepatitis B, hepatitis A and smallpox. For instance, according to 2014-2016 statistics by the UK government (GOV.UK, 2019), there was a 100% decrease in measles prevalence in England. Other data by GOV.UK (2019) indicate that as at 2018, only 136 cases of pertussis was reported in England, compared to 508 cases reported in 2012, an improvement attributed to vaccination (Public Health England, 2020). On the other hand, the NHS statistics indicates a 100% absence of polio in England, a phenomenon that is largely attributable to the polio vaccine (National Health Service, 2018). These dramatic decreases in preventable diseases as a result of mass vaccination justify the need for widespread vaccination and its potential role in solving socio-economic problems and reducing the burden on the UK’s health system.
Demystifying Vaccine Myths
Despite the plethora of research indicating the safety and efficiency of most vaccines (Diamond & Pierson, 2020), not all UK population recognize the importance of vaccination. Statistics on previously rolled out vaccines indicate that poor knowledge and misinformation about vaccines create a significant barrier against vaccination rates in the UK (Le et al, 2020). In this regard, Ghaebi et al (2020) confirm that much of the misinformation is perpetuated by vaccine sceptics who spread rumours about the recommended vaccine schedules. Ideally, the sceptics raise concern over three major issues namely: the safety and side effects of vaccines, the effects of vaccine schedule over people’s immune system, and the purported link between vaccine and other long-term illnesses such as autism (Bennet et al, 2020). However, there are scientific evidences that have addressed these issues.
Safety Monitoring
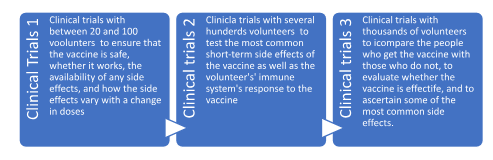
Regarding vaccine safety and side effects, vaccines undergo various safety monitoring and tests long before they are even tested on humans (Bennet et al, 2020). Beforehand, the safety precautions begin by an application for new safety certificate from relevant drug authorities (e.g. the UK’s Medicines and Healthcare products Regulatory Agency, MHRA; or the US’s Food and Drug Administration, FDA). In the process of applying for approval, the applicants must illustrate the testing and manufacturing procedures of the drug, as well as the proposed evidence-based studies and tests to evaluate the vaccine’s safety (Edwards et al, 2016). Each of the submissions undergo a series of rigorous reviews before undergoing clinical trials as described below:
Moreover, the certifying authority might permit the concomitant use of existing studies on the new vaccine to ensure they do not affect the safety and effectiveness of the existing vaccine (Le et al, 2020). Meanwhile, upon passing a new vaccine through the three phases, they must be further scrutinised before they are approved for use among the public. The clinical trial data is then reviewed by a team of medical experts before developing an effective immunization schedule. According to Sunita et al (2020), this process involves an examination of the severity of the disease being prevented, as well as the optimal age for which the vaccine is suitable. The recommendations from these reviews are then submitted for final approval before being officially admitted to the country’s official immunization schedule (Angelidou et al, 2020).
However, the rigorous monitoring does not end upon approval and admission of the vaccine into the country’s immunization schedule. Rather, other regulatory bodies such as the Joint Committee on Vaccination and Immunisation continuously monitor the safety and efficacy of the vaccine. Some of the issues they are on the lookout for during the continuous monitoring include any reports of adverse events after the vaccination – which anyone including the recipients, their parents or healthcare professionals can report; the maintenance of an exclusive database on the recorded vaccines side effects – facilitating an evaluation of whether the vaccine is associated with any of such side effects, and finally the development and execution of quality clinical studies that help with consultations among clinicians about the safety of the vaccine (Diamond & Pierson, 2020).
Apart from safety and side effects issues, sceptics also raise issues regarding the safety of vaccine ingredients. However, according to Ghaebi et al (2020), these ingredients are rigorously reviewed by pharmaceuticals manufacturing agencies and manufacturers to ensure that the preservatives and adjuvants used in the vaccine are safe (Edwards et al, 2016). Whereas some ingredients such as aluminium and formaldehyde can seem unnecessary and dangerous when reviewed out of context, according to Centers for Disease Control (2015a), most ingredients used in vaccines are rigorously reviewed for safety before used in the public domain. Moreover, these ingredients are only included when they significantly contribute to the vaccine’s efficacy. For instance, adjuvants are only added to vaccines because of their chemical components that help the body’s immune response to increase the robustness of the body’s immune system (Le et al, 2020). Nonetheless, vaccine sceptics have continued to single out certain ingredients of vaccines as unnecessary and dangerous:
Mercury
Today, only the multi-dose vaccines for flu contain thimerosal, which is a mercury derivative used in preventing bacterial growth (Centers for Disease Control, 2015b). Noteworthy, thimerosal is not included in any vaccine meant for children. That said, thimerosal contains ethyl-mercury, which the body rapidly eliminates (Bennet et al, 2020). According to Ghaebi et al (2020), ethyl-mercury differs from methylmercury, which is also found in fish, is toxic, and stays in the body for several years. However, it is important to note that major studies (e.g. Centers for Disease Control, 2015b) have associated thimerosal with autism.
Aluminium
The other controversial ingredient of vaccines is aluminium. According to Diamond & Pierson (2020), many vaccines contain small amounts of aluminium, which have been found to improve the body’s immune system through better efficacy of the agent vaccine. Aluminium is also found in drinking water (but in small quantities), infant formula, breast milk and foods (Le et al, 2020). That said, drug authorities responsible for vaccine authorization must monitor the aluminium content of new vaccines to ensure they fall below toxicity levels.
Antibiotics
Antibiotics content of vaccines have also been criticized by some sceptics. According to Diamond & Pierson (2020), most vaccines contain antibiotics because they help prevent contamination of the vaccine agents. Food and Drug Administration (2014) observed that some antibiotics such as sulfa drugs, cephalosporins and penicillin are most likely to cause severe allergic reactions in children and are therefore never used in vaccines. Moreover, most of the antibiotics in the vaccines are significantly reduced during the drug purification process. Consequently, they become undetectable.
Formaldehyde
Finally, the other controversial vaccine ingredient is formaldehyde, which is an organic chemical created during the body’s energy production and protein synthesis process (Bennet et al, 2020). Formaldehyde is also found in building materials as well as some household products. According to Ghaebi et al (2020), vaccines contain a negligible amount of formaldehyde compared to the amounts naturally produced in the body. They are essentially used in vaccines to inactivate viruses.
Cumulatively, these issues create an ethical dilemma around the production and distribution of vaccines, especially currently when the global healthcare community is struggling to fight COVID-19. To facilitate a better roll out of COVID-related vaccines, it is important to identify the ethical principles and priorities as well as their normative costs in the context of the pandemic. By identifying the ethical principles, it would be easier to identify the priorities for the vaccine distribution as the world transits into a mass vaccination era.
A Reflection on the Ethical Principles
In the field of public health ethics, stakeholders discuss six major normative principles that good public health actions (e.g. immunization) should be based on, namely: the population health maximization principle, the justice principle, the Harm principle, the principle of public trust, the principle of reciprocity and solidarity, and the autonomy principle (Stephenson et al, 2020). Ideally, according to Bandyopadhyay et al (2020), these principles provide a foundational basis for the distribution of scarce resources, especially within the context of the pandemic ethics (Württemberg, 2020). Before delving into each principle, it is also important to note that the interpretation of each principle is based on the context of COVID-19 vaccination that is most likely to occur under scarce resources.
The principle of population health maximization
Ideally, according to Filia et al (2020), the COVID-19 mortality and morbidity should be kept as low as possible. Developing effective epidemiological guidance on how to maintain low mortality and morbidity through the vaccine prioritization policy will help in effective decision-making.
The principle of justice
One of the most effective approaches to reducing health inequality is through fairness and justice in the distribution of health resources. By prioritizing the principle of justice in the vaccination policy, it will be easier to have everyone get the vaccine at their due dates and based on their health needs. This will also ensure that no group or individual is discriminated based on their personal characteristics such as age, gender, or economic status.
The principle of autonomy
The principle of autonomy gives recognizes every individual’s right to make their own informed choices regarding voluntary vaccination, and that such individuals are free to make decisions based on their beliefs, norms and wishes (Pickering et al, 2020). Prioritizing the principle of autonomy in the policy means that mandatory vaccination will be avoided at all cost.
The harm principle
Whereas the principle of autonomy grants individuals the right to self-determination, the harm principle dictates that people should not harm others while exercising their right to self-determination (James, 2020). Therefore, considering the potential impact of one’s vaccination status on others, prioritizing the harm principle in the immunization policy can have a positive health impact on the larger population.

The principle of public trust
This principle stipulates that public institutions have the responsibility to sensitize on, regulate and practice vaccine distribution in a trustworthy manner (Azzari, et al 2020). Furthermore, it requires that the institutions should act according to transparently available democratic and moral values. Incorporating this principle in policy will help build public trust towards the vaccines and the government’s initiative to distribute it.
The principle of reciprocity and Solidarity
According to Pickering et al (2020), this principle stipulates that policy on vaccine distribution should consider the socio-economic interdependence among the general public at different levels – also known as solidarity. On the other hand, the principle requires that the vaccine distribution should also consider reciprocity, whereby priority is given to individuals who face heavier burden in protecting the public good e.g. frontline nurses and doctors.
Recommendations
Based on the above principles, the following policy recommendations seem to be appropriate as far as the roll out of mass COVID-19 mass vaccination in the UK:
- There needs to be a clear, transparent, and participatory communication with the UK’s public to gain and maintain public trust and acceptance of the adopted immunization strategy. This should include engagement and sensitization about the current state of knowledge about the vaccine as well as the political decision-making processes together with the underlying ethical considerations. Such level of transparency will help address the concerns of various anti-vaxx movements in the UK. Furthermore, through transparency and sensitization, it will be easier for the authorities to fight conspiracy theories about the vaccination policy. That said, public health authorities such as the NHS are responsible for sensitizing the public about various aspects of the vaccine such as its safety and effectiveness – including information about the vaccine’s side effects and any potential limits on its effectiveness. Other pieces of information that should be communicated with transparency include: the immunization program’s prioritization strategy, any challenges and opportunities to revise the strategy; and the various types of stakeholders involved in the vaccine development and distribution.
- All the decisions regarding vaccination should be based on equality and morality of human beings, based on the best available scientific evidence to promote population health by preventing COVID-19, and based on democratic legitimacy.
- Priority should be given to health workers and other essential personnel such as the fire brigades, public transport practitioners, the police, supermarket personnel and public administration staff. These populations should be given priority because they are at a higher risk of being infected; because they are at a higher risk of infecting others, and to ensure a continuity of the functioning of the society.
- Upon immunizing essential workers, the distribution of remaining doses should be done fairly – in a way that secures equality for everyone. This could possibly be done through a lottery process, whereby fairness is secured rather than leaving the fairness of the distribution at the mercy of market forces.
In conclusion, this policy briefing has several policy issues concerning the development and administration of vaccines, including the COVID-19 vaccine that is expected to reach every corner of the world soon. The brief has also reflected on the science of vaccines as well as why it is important to prioritize immunization. It informs health policy formulation, public health practitioners and other public health practitioners at different levels of the UK government.
Dig deeper into Vaccination Of Children In The Uk with our selection of articles.
References
Angelidou, A., Diray-Arce, J., Conti, M. G., Smolen, K. K., Van Haren, S. D., Dowling, D. J., ... & Levy, O. (2020). BCG as a Case Study for Precision Vaccine Development: Lessons From Vaccine Heterogeneity, Trained Immunity, and Immune Ontogeny. Frontiers in Microbiology, 11, 332.
Azzari, C., Moriondo, M., Nieddu, F., Guarnieri, V., Lodi, L., Canessa, C., ... & Baldovin, T. (2020). Effectiveness and impact of the 4CMenB vaccine against group B meningococcal disease in two Italian regions using different vaccination schedules: a five-year retrospective observational study (2014–2018). Vaccines, 8(3), 469.
Baden Württemberg (2020) Influenzapandemieplan Baden-Württemberg. 2. März 2020. https://sozi-alministerium.baden-wuerttemberg.de/fileadmin/redaktion/m-sm/intern/downloads/Down-loads_Gesundheitsschutz/Influenzapandemieplan-BW.pdf
Bandyopadhyay, A. S., Gast, C., Rivera, L., Sáez-Llorens, X., Oberste, M. S., Weldon, W. C., ... & Rüttimann, R. (2020). Safety and immunogenicity of inactivated poliovirus vaccine schedules for the post-eradication era: a randomised open-label, multicentre, phase 3, non-inferiority trial. The Lancet Infectious Diseases.
Bennet, B. M., Wolf, J., Laureano, R., & Sellers, R. S. (2020). Review of current vaccine development strategies to prevent coronavirus disease 2019 (COVID-19). Toxicologic pathology, 48(7), 800-809.
Britton, T., Ball, F., & Trapman, P. (2020). A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science, 369(6505), 846-849.
Cantore N., Hartwich F., and Lavoipa A. (2020) Coronavirus: the economic impact. UNIDO. Available from: https://www.unido.org/stories/coronavirus-economic-impact-10-july-2020 [Accessed on 2/1/2020]
Carrondo, M. C., & Moita, J. J. (2020). Potentially preventable urinary tract infection in patients with type 2 diabetes–A hospital-based study. Obesity Medicine, 17, 100190.
Centers for Disease Control (2015a) Common Vaccine Safety Concerns.”, Available from: https://www.cdc.gov/vaccinesafety/concerns/index.html [Accessed on 2/1/2020]
Centers for Disease Control (2015b) Thimerosal in Vaccines. Available from: https://www.cdc.gov/vaccinesafety/concerns/thimerosal/index.html. [Accessed on 2/1/2020]
Centers for Disease Control (2016) Vaccine Adjuvants. Available from: https://www.cdc.gov/vaccinesafety/concerns/adjuvants.html. [Accessed on 2/1/2020]
Chua, B. Y., Sekiya, T., & Jackson, D. C. (2018). Opinion: making inactivated and subunit-based vaccines work. Viral Immunology, 31(2), 150-158.
Diamond, M. S., & Pierson, T. C. (2020). The challenges of vaccine development against a new virus during a pandemic. Cell Host & Microbe, 27(5), 699-703.
Dooling, K. L., Guo, A., Patel, M., Lee, G. M., Moore, K., Belongia, E. A., & Harpaz, R. (2018). Recommendations of the Advisory Committee on Immunization Practices for use of herpes zoster vaccines. Morbidity and Mortality Weekly Report, 67(3), 103.
Edwards, K. M., Hackell, J. M., Committee on Infectious Diseases, & Committee on Practice and Ambulatory Medicine. (2016). Countering vaccine hesitancy. Pediatrics, 138(3).
Ehreth, J. (2003). The value of vaccination: a global perspective. Vaccine, 21(27-30), 4105-4117.
Ewbank L., Thompson J., McKenna H., Anandaciva S. (2020) NHS Hospital bed numbers: past, present, future[Internet]. The King's Fund: United Kingdom. [update 26 March 2020; cited 29 April 2020]. Available fromhttps://www.kingsfund.org.uk/publications/nhs-hospital-bed-numbers.
Ewbank L., Thompson J., McKenna H., Anandaciva S. NHS Hospital bed numbers: past, present, future[Internet]. The King's Fund: United Kingdom. Available fromhttps://www.kingsfund.org.uk/publications/nhs-hospital-bed-numbers.
Filia, A., Rota, M. C., Grossi, A., Martinelli, D., De Graaf, T., Dominguez, A., ... & Rezza, G. (2020). Are vaccine shortages a relevant public health issue in Europe?. European Journal of Public Health, 30(Supplement_5), ckaa165-670.
Flynn, D., Moloney, E., Bhattarai, N., Scott, J., Breckons, M., Avery, L., & Moy, N. (2020). COVID-19 pandemic in the United Kingdom. Health policy and technology, 9(4), 673–691. https://doi.org/10.1016/j.hlpt.2020.08.003 [Accessed on 2/1/2020]
Fontanet, A., & Cauchemez, S. (2020). COVID-19 herd immunity: where are we?. Nature Reviews Immunology, 20(10), 583-584.
Food and Drug Administration (2014) Common Ingredients in the U.S. Licensed Vaccines. US Food and Drug Administration. Available from: https://www.fda.gov/biologicsbloodvaccines/safetyavailability/vaccinesafety/ [Accessed on 2/1/2020]
Ghaebi, M., Osali, A., Valizadeh, H., Roshangar, L., & Ahmadi, M. (2020). Vaccine development and therapeutic design for 2019‐nCoV/SARS‐CoV‐2: Challenges and chances. Journal of cellular physiology, 235(12), 9098-9109.
Iwasaki, A., & Omer, S. B. (2020). Why and how vaccines work. Cell, 183(2), 290-295.
James III, T. L. (2020). Ethically Addressing Vaccine Hesitancy in Pediatric Populations.
Le, T. T., Cramer, J. P., Chen, R., & Mayhew, S. (2020). Evolution of the COVID-19 vaccine development landscape. Nat Rev Drug Discov, 19(10), 667-8.
Lipsitch, M., Grad, Y. H., Sette, A., & Crotty, S. (2020). Cross-reactive memory T cells and herd immunity to SARS-CoV-2. Nature Reviews Immunology, 20(11), 709-713.
Lurie, N., Saville, M., Hatchett, R., & Halton, J. (2020). Developing Covid-19 vaccines at pandemic speed. New England Journal of Medicine, 382(21), 1969-1973.
National Health Service (2018) Polio. Internet. Available from: https://www.nhs.uk/conditions/polio/ [Accessed on 2/1/2020]
National Health Service England (2020) NHS steps up coronavirus fight with two more Nightingale Hospitals. [Internet]. England, 10 April 2020. Available formhttps://www.england.nhs.uk/2020/04/nhs-steps-up-coronavirus-fight-with-two-more-nightingale-hospitals/.
National Health Service. Bed availability and occupancy data- overnight. England, 2020. https://www.england.nhs.uk/statistics/statistical-work-areas/bed-availability-and-occupancy/bed-data-overnight/.
Peiris, M., & Leung, G. M. (2020). What can we expect from first-generation COVID-19 vaccines?. The Lancet, 396(10261), 1467-1469.
Pickering, L. K., Meissner, H. C., Orenstein, W. A., & Cohn, A. C. (2020, March). Principles of Vaccine Licensure, Approval, and Recommendations for Use. In Mayo Clinic Proceedings (Vol. 95, No. 3, pp. 600-608). Elsevier.
Stephenson, K. E., Wegmann, F., Tomaka, F., Walsh, S. R., Tan, C. S., Lavreys, L., ... & Peter, L. (2020). Comparison of shortened mosaic HIV-1 vaccine schedules: a randomised, double-blind, placebo-controlled phase 1 trial (IPCAVD010/HPX1002) and a preclinical study in rhesus monkeys (NHP 17–22). The Lancet HIV.
Sunita, Sajid, A., Singh, Y., & Shukla, P. (2020). Computational tools for modern vaccine development. Human Vaccines & Immunotherapeutics, 16(3), 723-735.
UK.GOV (2019) Measles in England [internet]. United Kingdom. Available from https://publichealthmatters.blog.gov.uk/2019/08/19/measles-in-england/ [Accessed on 2/1/2020]
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



