Cost effective analysis of combined pharmacotherapy and psychological therapy compared with pharmacotherapy in the treatment of post-traumatic stress disorder (PTSD)
- 16 Pages
- Published On: 03-10-2023
Introduction
Post-traumatic stress disorder (PTSD) is a hampering anxiety disorder caused by the exposure to traumatic events, for example, war, disaster, an interpersonal event like physical or sexual assault, accident, etc. There are three main symptoms of PTSD, one those related to re-experiencing the event, two: avoidance and arousal and three: distress and impairments caused by the first two symptoms (Hetrick et al. 2010). For students seeking to understand this complex topic, psychology dissertation help can provide valuable insights and guidance.
The person affected with PTSD has to face issues of economic instability, which not only affects the person mentally but also hampers the quality of life. As a person affected with PTSD is observed to be depressed most of the time, absence from the workplace is also seen to increase. This again affects the employment of the PTSD person as unemployment is common due to high rate of absence from work. In addition, for treating patients of PTSD, it requires medicines and other long-term treatments, which are very expensive. This negatively influences the patients’ lifestyle with reduced economic stability. Patients have to spend large amount of money on treatments, which makes their life miserable as other expenses are also high. This is supported by Endicott et al. (1976), in terms of a PTSD patient having lesser income cannot contribute much in leading a healthy lifestyle. This reflects on the degradation in the quality of life of the patient due to economic downfall from different angles.

Antidepressant is the most commonly used pharmacological intervention for the treatment of PTSD (Davidson 1999). However, guidelines from national institute for clinical excellence (NICE) suggest that people recover from PTSD effectively when a combination of both pharmacotherapy and psychological therapy is used. Kessler et al. (1995) stated that men are 8.1% more likely to develop PTSD after a traumatic event than 20.4% in women. Other than these interventions, there exist some legal and organisational policies, which are implemented towards better care of patients with PTSD. The legal and organisational policies are not only effective for providing enhanced care to patients; it also contributes in improving the quality of life of the patient. In addition, as patients have their right to obtain respect from the service providers of healthcare organisations, these legal policies are helpful in maintaining the rights of the patient.
Care Act 2014-This Act sheds light on the right of every individual including patients of PTSD to get proper treatments from the healthcare organisation. This also reflects on the service providers’ duty to maintain well-being of the patients by providing utmost care services depending on the nature of the disease. Care Act 2014 stresses on the fact of respecting patients when providing care services along with noting their choices and decisions. As PTSD patients are in mentally depressed state, therefore, there emotional wellbeing along with their physical wellbeing needs to be maintained as per their right. On the other hand, PTSD patients with the healthcare organisations often have to face discrimination and abuse from others or service providers. Hence, the Act also emphasises on protecting patients from abuse, discrimination and negligence. Along with this, it is duty of the local authorities to provide support to the PTSD patients in terms of financial support so that quality of life can be improved (Legislation.gov.uk, 2016).
Safeguarding Vulnerable Adults 2015- In context of patients of PTSD facing challenges in their life due to the post-traumatic disorder, they also faces issues of abuse, negligence and harm. Being vulnerable makes them weak towards society, and they are susceptible to be neglected by the society as well as in receiving proper treatments. According to Simon et al. (2008), Safeguarding Vulnerable Adults 2015 imposes rights of these patients to remain free from harassments within the society. Not only this is reflected, but service providers with the healthcare organisations have the responsibility of protecting these patients from abusers as well as counselling the victim. It also reflects on the fact of giving enhance attention to PTSD patients so that they face lesser issues of negligence with the healthcare organisation.
Maintaining Dignity- Every individual has achieved certain degree of respect and dignity before facing health issues or diseases such as PTSD. After their health deteriorates immensely, people neglect them and they get lesser respect from the society. Hence, maintaining dignity of patients within the healthcare and getting equal respect from the society helps patients of PTSD to recover from their severe condition. PTSD patients are in the depressed state and giving them respect and treating them with dignity makes them feel valuable in the society, which has positive effects of improving their state of mind.
Confidentiality of information- Within healthcare organisations, where PTSD patients are treated with appropriate care services and medications, service providers are required to keep patients’ information confidential. Organisational policies such as confidentiality of information in association with Data Protection Act 1998 reflect on the issue of protecting information of patients from disclosing to others (Legislation.gov.uk, 2016). As argued by Kessler et al. (1995), often service providers face dilemma of unable to disclose patient’s history and details even to the required health professionals other than doctors. Therefore, to overcome this issue, Data Protection Act 1998 expressed taking contents of the patient as well as from the doctors before disclosing facts about patient to other professionals. This is beneficial for PTSD patients in terms of not getting identified in the society as a vulnerable person, which affects their dignity and respect.
Methodology
Study Design:
Cost-effectiveness of two open labels randomised controlled trials (RCT) with the same number of patients allocated into the two groups in the ratio of 1:1. Eligible patients will be recruited from existing sexual health clinics, a referral from GP and charities that look after abused women.
For more information refer to appendix 1Setting / Location / Sample Size:
The study will take place in selected existing two trauma sexual health outpatient clinics. The trial will aim to recruit 430 participants with PTSD. Informed consent will be sought prior to the trial by a trained research assistant to help reduce social desirability that takes place between doctor and patient. The programme will run for a period of one year with assessments taken at baseline and six months, ten and twelve months.
Ethical Consideration:
Ethical approval will be obtained from the Ethical Research Committee. There will be confidentiality of data. Allocation list will be produced and patients assign to either group; this will be performed by a statistician that is not part of the study and the list will then be given to the study data manager.
Sample Size Calculation:
The outcome measures will be continuous changes in GAF (Endicott et al., 1976) and World Health Organisation Disability Assessment Schedules II-36 WHO-DAS (Pocock, 1983). The study sample size will be effectively powered by calculating sample size satisfactorily to identify variance in the group thereby producing valid results (Anderson, 1980, Anderson et al., 1986).
For more information refer to appendix 2
Identification Measurement and Valuation of Outcomes:
The primary outcome measures will look at the change in PTSD severity from baseline to endpoint using valid and reliable clinician- administered PTSD scale (CAPs Blake, 1990).
Secondary Outcomes:
NICE reported that in many situations co-morbid problems secondary to the PTSD, such as depression, general anxiety or alcohol or substance misuse, get better with trauma-focused psychological treatment. Treatment findings of PTSD show that with effective treatment of PTSD, co-morbid signs of depression and anxiety are reduced.
QALYs will measure improvements in Social Functioning, Global functioning scores and this will be based on EuroQol EQ-5D questionnaire, GAF (a structured scoring system with a minimum score of 0 and a maximum of 100) and Work and Social Adjustment Scale (Mundt, 2002). The study will also measure client satisfaction with the service using the Client Satisfaction Questionnaire.
Unit Costing and Costs / Identification of Resources:
The costs include costs of healthcare within and outside of the programme. Indirect costs include the cost of the police investigation; refurbishment of clinic facilitates to accommodate changes in the programme. The final cost will be calculated as the summation of products of the volumes of resources to be used alongside their individual unit cost. Resources can be identified by conducting search for relevant information on databases such as Pubmed, EBSCO, Medline, and so on. Information will be obtained by searching from these databases with relevant topics and based on the inclusion criterion appropriate journals and information will be selected.
In healthcare organisations, for treating patients of PTSD, unit cost per hour of contact with clients is £15 and for 12 sessions it is £183. Capital costs are estimated to be £7435 per year, which includes sharing basis for treatment process. Local authority expenses are £34 for attending each client. In addition, cost of healthcare services per residents is £75 per resident per week and for obtaining social services is £107 per resident per week.
Measurement / Valuation of Resources:
The trial will use clinical report forms of both physician and patient centred and the European version of PTSD severity indexes to collect data from following –up visits to the healthcare resources, travel expenses. Wellbeing related quality of life will be accessed using the disease-specific tool and psychiatric morbidity with a validated questionnaire.
This can be alligned with the Care Act 2014 policy, which stresses on providing better care services along with im proving quality of life of PTSD patients.
Method of Economic Evaluation:
The study will use the cost-effective method of economic evaluation to assess the intervention at the end of the trial, alternative treatment which in this case is “treatment as usual” will be assessed on costs and significant health-related gains. Economic evaluation can also be linked with the Care Act 2014, which emphasises on the responsibility of local authorities support patients in financial aspects. The willingness to pay threshold (WTP) will be ascertained to ensure that it is in line with NICE guideline of £30, 000 and if the ICER < WTP the study will be considered as being cost-effectiveness.
Statistical/Sensitivity Analysis:
Statistical Package for Social Science (SPSS IBM, 2006) is to be used for the quantitative analysis.
Intention to treat analysis will be performed on all participants that were recruited into the trial. Mantel-Haenszel X2 test adjusted for the stratification variable will be used to compare between the groups the proportions of patients that responded. The difference between the 2-arm summarised by average and standard deviations with a 95% confidence interval in both groups after adjusting for bias and using accelerated non-parametric bootstrapping drawing up 15 000 samples. Multi-way sensitivity analysis will be performed to examine the robustness of cost suitability of intervention (WTP to pay up to £30,000) to variations in unit cost and UK time trade-off based health utility algorithm. This evaluation can be linked with the confidentiality of information and Care Act 2014. This is because, these policies highlights the importance of respecting patients’ identity and protecting personal information.
Presentation of Results:
The findings of the study will be reported in line with revised CONSORT guidelines; the study does not plan to carry out interim analyses however the data will be cleaned prior to analysis. The findings will show the interaction between the many parts of the intervention and how they yield proposed outcomes. It will also show to patients, families or caregivers any specific component of the intervention acceptable to them. All costs will be calculated for both arms of treatment and cost-effectiveness of the intervention will be compared to treatment.

Placing Results in Context:
Monitoring and safety of the study will be regulated by an independent committee that will include mental health professionals, user group representation and caregiver groups. They will review the protocol before the trial begins and data will be sent to the committee quarterly including data of dropouts and participants who did not consent to the study.
Continue your journey with our comprehensive guide to Case Study on Pharmacological, Ethical and Legal Implications.
Implementation of combined therapy does not require major organizational change as most of the clinicians and mental health nurses are already trained in their respective areas, rather it will give staff the opportunity to know that with adequate support the changes made to adequately look after patients with PTSD can be feasible.
References
- "Care Act 2014", Legislation.gov.uk., 2016. 1 Mar. 2016.
- "Data Protection Act 1998", Legislation.gov.uk., 2016. 2 Mar. 2016.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd Edition. Washington, DC: American Psychiatric Association, 1980.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington, DC: American Psychiatric Association, 1994.
- Anderson C, Reiss D, Horgarty G. Schizophrenia and the family: Schizophrenia and the family: A practitioner’s guide to psycho-education and management. New York: Guildford Press. 1986
- Anderson CM. A psycho-educational program for families of patients with schizophrenia. In W.R McFarlane (Ed) Family therapy in schizophrenia pp, 99-116, New York: Guildford Press 1980
- Australian Centre for Posttraumatic Mental Health. Australian Guidelines for the Treatment of Adults with Acute Stress Disorder and Posttraumatic Stress Disorder. Melbourne: ACPMH, 2007
- Baigent C: The need for large-scale randomized evidence. British Journal of Clinical Pharmacology 1997; 43:349–353
- Ballenger JC, Davidson JRT, Lecrubier Y, Nutt DJ, Foa EB, Kessler RC, McFarlane AC, Shalev AY. Consensus Statement on Posttraumatic Stress Disorder from the International Consensus Group on Depression and Anxiety. Journal of Clinical Psychiatry 2000; 61:60–6
- Ballenger JC, Davidson JRT, Lecrubier Y, Nutt DJ,Marshall RD, Nemeroff CB, Shalev AY, Yehuda R. Consensus Statement update on posttraumatic stress disorder from the International Consensus Group on Depression and Anxiety. Journal of Clinical Psychiatry 2004; 65:55–62
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961; 4:561–71
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS, Keane T M. A clinician rating scale for assessing current and lifetime PTSD: the CAPS-1. Behaviour Therapist 1990;13:187-188
- Cohen JA, Mannarino AP, Perel JM, Staron V. A pilot randomized controlled trial of combined trauma-focused CBT and sertraline for childhood PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry 2007; 46:811–9
- Connor M, Rothbaum B, Foa EB, Davidson JRT, Cahill S, Clary C. A controlled trial of combined sertraline and prolonged exposure therapy in posttraumatic stress disorder. European Neuropsychopharmacology 2002; 12:s335
- Creamer M, Burgess P, Pattison P. Reaction to trauma: a cognitive processing model. Journal of Abnormal Psychology 1992; 101 (3):452–9
- Davidson J. Drug therapy for post-traumatic stress disorder. British Journal of Psychiatry 1992; 160:309–314
- Davidson JR. Recognition and treatment of posttraumatic stress disorder. Journal of the American Medical Association 2001; 286:584-588
- Davidson JRT, Connor KM. Management of posttraumatic stress disorder: Diagnostic and therapeutic issues. Journal of Clinical Psychiatry 1999; 60:33–38
- Davidson JRT, Payne VM, Connor KM, Foa EB, Rothbaum BO, Hertzberg MA, Weisler RH. Trauma, resilience and saliostasis: effects of treatment in post-traumatic stress disorder. International Clinical Psychopharmacology 2005; 20:43–48
- Davidson JRT. Pharmacotherapy of posttraumatic stress disorder: Treatment options, long-term follow-up, and predictors of outcome. Journal of Clinical Psychiatry 2000; 61:52–56.
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment of Functioning scale (GAF). A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976; 33:766–71
- Fisayo Momodu 2014: Assessing the effectiveness of an integrated early intervention service vs treatment as usual in first-episode schizophrenia in Nigeria: protocol for a randomised controlled trial
- Flannery BA, Volpicelli JR Pettinati HM. Psychometric properties of the Penn Alcohol Craving Scale. Alcoholism:Clinical and Experimental Research 1999;23(8):1289–1295.
- Foa EB, Steketee G, Rothbaum BO. Behavioural-cognitve conceptualizations of post-traumatic stress disorder. Behavior Therapy 1989; 20: 155–76
- Hetrick SE, Purcell R, Garner B, Parslow R. Combined pharmacotherapy and psychological therapies for post-traumatic stress disorder (PTSD) (Review). The Cochrane Library2010, Issue 7
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry 1995; 52 (12):1048–60.
- Larsen DL, Attkinson C C, Hargreaves WA,Nguyen T.D. Assessment of client/patient satisfaction : Development of a general scale. Evaluation and program planning, 1979, 197-207
- Marshall RD, Cloitre M. Maximizing treatment outcome in post-traumatic stress disorder by combining psychotherapy with pharmacotherapy. Current Psychiatry Reports 2000; 2: 335–40.
- Mundt JC, Shear KM, Greist JM. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. British Journal of Psychiatry 2002; 180: 461–464.
- OttoMW,Hinton D, Korbly NB, Chea A, Ba P, Gershuny BS, Pollack MH. Treatment of pharmacotherapy-refractory post-traumatic stress disorder among Cambodian refugees: a pilot study of combination treatment with cognitive behaviour therapy vs sertraline alone. Behaviour Research and Therapy 2003; 41:1271–1276.
- Pocock S J. Clinical Trials: A practical approach. Wiley 1983
- Rothbaum BO, Cahill SP, Foa EB, Davidson JRT, Compton J, Connor KM, Astin MC, Hahn C. Augmentation of sertraline with prolonged exposure in the treatment of post-traumatic stress disorder. Journal of Traumatic Stress 2006; 19 (5):625–638.
- Rothbaum BO, Foa EB, Davidson JRT, Cahill SP, Connor KM. Augmentation of sertraline with cognitive-behavioural therapy in the treatment of PTSD. 157th Annual Meeting of the American Psychological Association. New York, 2004; Vol. May 1–6. [: NR513]
- Simon NM, Connor KM, Lang AJ, Rauch S, Krulewicz S, LeBeau RT, Davidson JR, Stein MB, Otto MW, Foa EB, PollackMH. Paroxetine CR augmentation for posttraumatic stress disorder refractory to prolonged exposure therapy. Journal of Clinical Psychiatry 2008; 69 (3):400–5.
- Spielberger CD, Gorsuch RL, Lushene RE, Press CP. State-Trait Anxiety Inventory (Self-Evaluation Questionnaire). Palo Alto, CA: Consulting Psychologists Press, 1970.
- Statistical Package for Social Sciences (SPSS), Illinois, Chicago: IBM; 2006.IBM.
- Stein DJ, Seedat S, van der Linden GJ, Zungu-Dirwayi N. Selective serotonin reuptake inhibitors in the treatment of post-traumatic stress disorder: a meta-analysis of randomized controlled trials. International Clinical Psychopharmacology 2000; 15 (2):S31–9.
- The GAF is a scale from 0 to 100 where higher scores indicate greater levels of functioning. Optimal mental health and coping capabilities are represented by scores in the 91 – 100 range. Persons with mild psychological problems fall in the 71 – 90 range.
- The WHODAS-2 is a disability assessment instrument based on the conceptual framework of the International Classification of Functioning, Disability, and Health (ICF). It provides a global measure of disability and 7 domain-specific scores. 19 May 2010
- World Health Organisation. The Tenth Revision of the International Classification of Diseases and Related Health Problems (ICD-10). http://www.who.int/classifications/ apps/icd/icd10online/: World Health Organisation, 1992.
- www.ncbi.nlm.nih.gov
- www.nice.org.uk/guidance/cg26/evidence/cg26-posttraumatic-stress-disorder-ptsd
- www.who.int/icidh/whodas/
- Yehuda R. Biological factors associated with susceptibility to posttraumatic stress disorder to posttraumatic stress disorder. Canadian Journal of Psychiatry 1999;44 (1):34–9.
Appendix 1
Cont. Study Design:
Inclusion criteria will be women diagnosed with PTSD assessed using a structured clinical interview based on the DSM-IV (Cohen, 2007) and are re-experiencing distressing events, avoidance or arousal in at least four weeks (Ballenger, 2004). Patients already diagnosed with a psychotic disorder are excluded.
The control group will receive treatment as usual which will be selective serotonin reuptake inhibitors (SSRIs); an antidepressant which may work in adjusting disparities in neurotransmitters believed to play a role in initiating and /or preserving PTSD symptoms (Stein, 2000). Participants in the intervention will receive both the SSRIs and trauma-focused psychological interventions. The subjects will receive ten sessions two times a week. Both arms of the trial will be delivered at the sexual health clinic.
Appendix 2
Formula used to calculate the sample size
n = f (α/2, β) × [p1 × (100 − p1) + p2 × (100 − p2)] / (p2 − p1)2
- Where n = sample size
- Alpha = is set at 0.05 significance level with a 95% confidence interval (this is to ensure that type 1 error is avoided)
- Power =1 beta at 90% (to avoid type 11 error)
- P1= % success expected in the intervention group = 0.500 (5% chance of erroneously reporting a significant effect is accepted).
- P2= % success expected in the control group = 0.300
- Calculated size per group = 190
- Total sample size per trial = 380
- 20% attrition rate = 215 participants per group
- Approximate total number of participants = 430
Appendix 3
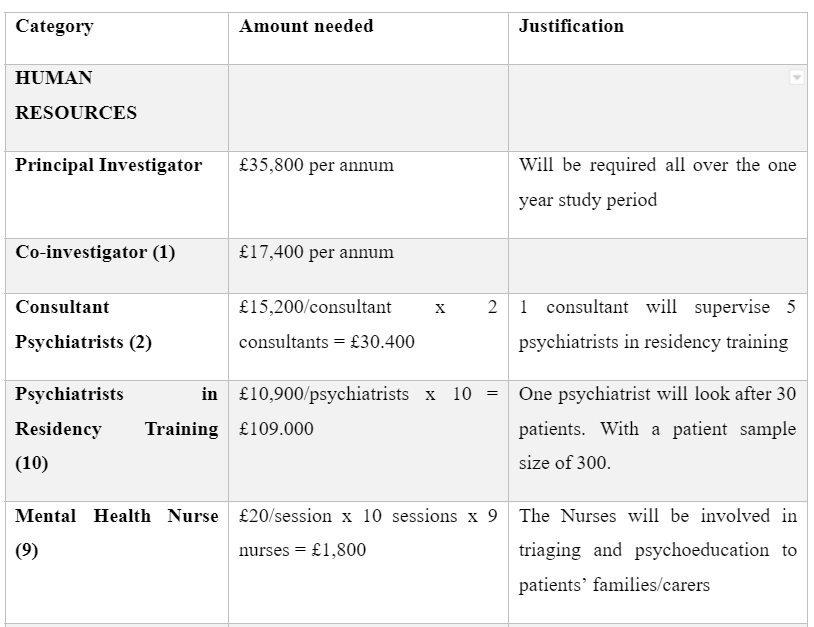
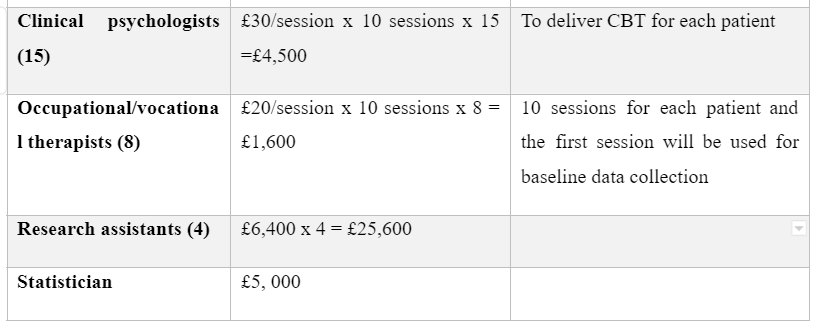
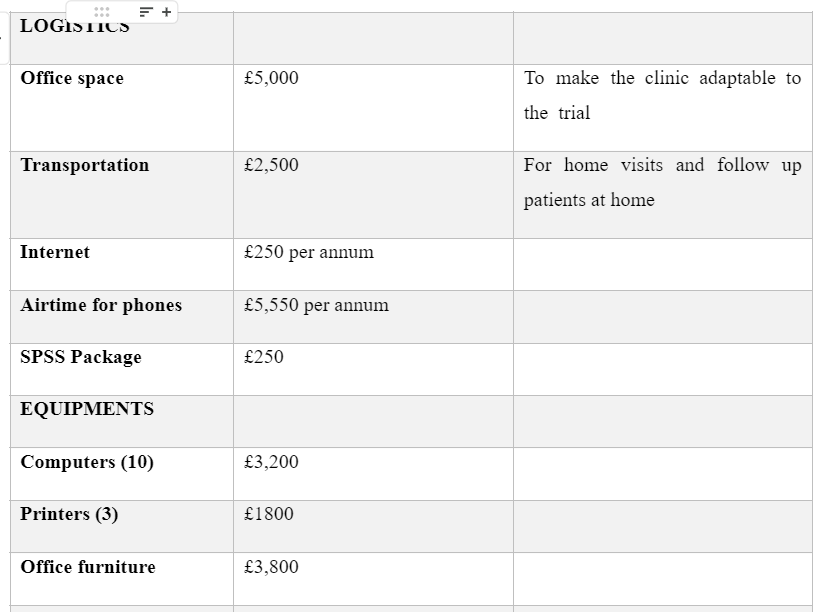
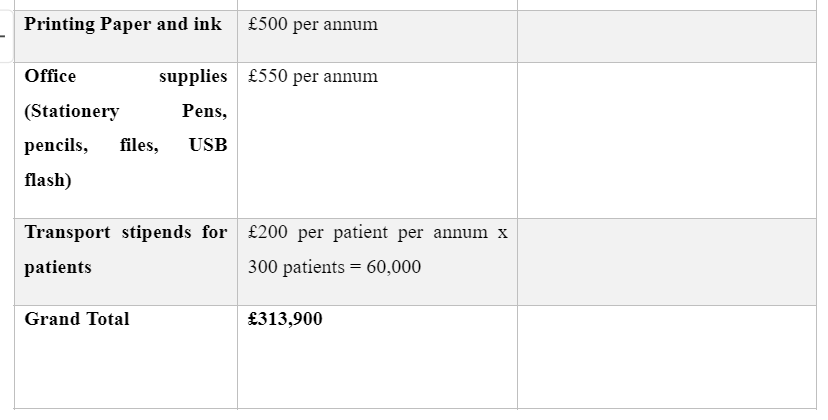
BUDGET
Costs and predicted expenses for the trial
Dig deeper into Cost effective analysis of combined pharmacotherapy and psychological therapy with our selection of articles.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



