Cemented vs Uncemented Stems in Total Hip Arthroplasty
INTRODUCTION
The great achievement of Total Hip Arthroplasty (THA) and the rate that its occurred are pre-dominantly due to development of cemented stems (charnley, 1960) the survival rate of it is 80% at 25 years (Berry et al. 2002, Callaghan et al. 2004). There has also been a huge increase in use of uncemented stems in recent times in place such as the U.S. due to the fact it allows bone ingrowth (Zicat et al. 1995, Kim et al. 1999, Della Valle et al. 2004, Sinha et al. 2004,) in spite of it costing more. In 2003 it is recorded that approximately 2/3 of all THA were done using uncemented stems, on the other hand some countries such as Sweden avoid using these techniques and use it more carefully (Malchau et al. 2002, Kurtz et al. 2005). Cemented and uncemented stems are diverse with many factors that can affect survivorship such as surface finishes, bearing, geometry etc.
There has always been a discussion occurring on whether uncemented stem or cemented stem is more better over many years since it was first introduced to currents time, taking into account factors such as survivorship, stability, durability etc. Cemented stem uses polymethylmethacrylate (PMMA) to function as a grout, producing an interlocking fit between cancellous bone and prosthesis. Uncemented stem depend on biological fixation of bone to a surface coating on the stem (Wilson,2017). The ideal fixation option should be directed by the results of the patient, specifically the stem survivorship as calculated by revision for aseptic loosening, this was a huge reason for uncemented to be introduced. Outstanding survivorship rates of cemented and uncemented stems however these studies have been disputed due to the fact that the sample size was small and the actual nature of the research, therefore the results can’t be justified on a regional or national level.
Cemented Stem
The durability and survivorship of a cemented stem depends on the quality of the cement technique and the design of the implant, bone-cement interface and cement-implant interface are the 2 interfaces that fixation occurs when it comes to the cemented technique. When cemented technique was first pioneered it consisted of introducing cement into an open medullary canal through finger packing and this pre-dominantly concluded in failure, cemented stem can be classed into two general groups :
Taper slip (force closed) : This type are collarless and have a very well-polished surface (Ra less than 1 micrometer) , they achieve longevity and stability by preventing the bone growing onto the surface of the stem thereby by decreasing the chances of fibrous membrane forming which results in loosening of the implant and this is done through micromotion. The critical Tolerance of the micro-movements which can be accepted are unknown as it depends on the user and certain factors of the actual implant (Viceconti et al. 2006) , through previous research it has been observed that micro-motion of an estimate of 40 μm can result to bone ingrowth and motions higher than 150 μm completely prevent bone ingrowth (Pilliar et al. 1986, Jasty et al. 1997). The taper slip stems achieve longevity and stability through micromotion on the stem surface interface leading to a slight distillation of the stem inside the cement mantle, generating radial stresses and eventually leading to solidity and firmness in the stem cement and bone cement interface (Davies N, Jackson W, Price A, Rees J, Lavy C.2006), exeter stem is an example of Taper slip stem
Composite beam (shape-closed) : This type achieves stability by making a firm connection between stem, cement and bone sustaining the position of the stem inside the mantle . The composite beam is designed with features including rough surface finish (Ra greater than 2 micrometer), the use of collar are utilised to enhance the survivorship at the stem-cement interface (Davies N, Jackson W, Price A, Rees J, Lavy. 2012).
Uncemented stem
There is a wide range of design when it comes to uncemented stems such as modular,tapered, S-rom, cylindrical etc and many other components to make the stem more stable such as proximal fins & ribs as well as splines which lessens the modulus of elasticity (Khanuja HS, Vakil JJ, Goddard MS. 2011). Uncemented stems were mainly introduced to combat the issue of stress shielding. When it comes to uncemented stem designs they all have similar goals and that is to increase stability and to maintain the stem in place while the surrounding bone adhere into or onto it. The reason why uncemented focuses on maximising stability is that the scale od micromotion has an affect on the tissue that builds at the bone stem interface. Uncemented stems are made in two ways:

On-Growth: This technique aims to create a textured surface and this is done via grit blasting or plasma spraying hydroxyapatite onto the stem and numerous marks are made on it for the bone to grow onto it (Mirza SB, Dunlop DG, Panesar SS, Naqvi SG, Gangoo S, Salih S. 2010) In-Growth: This technique aims to make microscopic pores thereby in which the bone can grow and this is engineered using sintered beads, fiber mesh and porous metals and this is what creates these pores, the ideal pore size for this technique is 50–400 μm. By using hydroxyapatite and tricalcium phosphate which are bioactive materials to coat the stem has drawn a lot of attention and interest. This is because these compounds actively stimulate osteoblasts, rather than just providing a scaffold for adherence (Thanner J. 1999). Research has shown progress in regards to weight transfer and radiographic appearance (Abrahams TG, Crothers OD. 1992), however there have been no conclusive result to show that there is improvement in terms of survivorship.

What has been done and why this is important
The Swedish hip registry (SHR) details a steady movement when it comes to the use of uncemented stems as there has been a heightened use for them, nevertheless it reported that 64% of patients in 2011 used cemented stems. When it came to younger patient and those who had good bone condition the use of uncemented stem was more popular and common, whereas when it came to older patients that are older than 70 years the use of cemented stem was more encouraged for them. In addition the SHR when it came to the use of cemented stems research showed that it had a 90% 16 year survivorship In comparison to the use of uncemented stem which was more likely to be revised during the first 8 years and through research it was observed this was probably due acetabular problems, however after 8 years the survivorship of the uncemented stem inclined to that of the cemented stem (Karrholm, Et al. 2016). When it came to those younger then that age of 70 the uncemented stem had fewer revisions ascribed to loosening. In the Norwegian hip registry they reported that in general cemented stems had a 20 year survival rate of 85% in comparison to uncemented which had a 50%, uncemented stems were preferred in patients > 60 years of age and cemented stem was preferred in patients < 60 years of age. According to the National Joint Registry of England and Wales (2016), the Kaplan-Meier estimates of cumulative percentage probability of revision after 13 years for cemented implants was 4.34% while for the uncemented implants was 8.66%. The cumulative percentage of revision (with 95%CI) at 9 years was 2.71% (2.57-2.87) for cemented, 6.71% (6.40-7.05) for uncemented (Michael Wyatt, Gary Hooper. 2014. As per these two reports, the cemented implants have a higher rate of survivorship than the uncemented ones. According to the New Zealand world registry (NZR) it had similar research outcome to that of other data mentioned previously, this can be seen in table 1 and figure 2. In addition the NZR has shown revision rate of 0.89/100 component years (cy) for uncemented THRs in patients under 55 years compared to 1.73/100 cy for cemented THR and 0.90/100 cy compared to 0.98/100 cy for those between 55-65 years (P < 0.001). Over a 65 years period this was overturned with cemented stem having a higher survival rate than uncemented stem(P < 0.001), the revision rate was lower in those patients < 65 years of age (0.65-0.45/100 cy) in contrast to patients > 65 years of age. Early revision occurred more in uncemented stems (0.899%) compared to that of cemented stems (0.353%) which represented all age groups however was more substantial in patients < 65 years of age (P < 0.001), when analysed why they needed early revision the research showed it could be due femoral fracture , dislocation etc. These results contradict that of the SHR which showed that during the first 5 years uncemented stems are revised two times the rate of cemented stems and the cemented stems where ten times less projected to require revision for periprosthetic fracture.


The NARA which is made up of the Scandinavian countries (Denmark, Norway, Finland and Sweden) which was established in 2007 and Finland later joined 3 years later in 2010. They published a report which included 347,899 THA’s patient aged 55 years of age from 1995-2011 (Mäkelä KT, Matilainen M, Pulkkinen P, et al.), 66.9% used cemented stem and 20.5% used uncemented stem. After modifying for factors such as age, sex etc and using Kaplen-Meier survival analysis , the results revealed the survivorship rate was lower in uncemented stem when compared to the cemented stem and this was in patients 65 years age. In addition Pederson et al carried out a study using NARA research data found out that the patients who were younger who used uncemented stems had less revisions and this was because of aseptic loosening than the ones who used cemented stems.
Search strategy
A systematic search was done on the main search engines namely Google, Bing and Yahoo, reporting the outcomes on survivorship rates of the fixation of both cemented and uncemented stems. In addition, published journals and books were used as referrals for the obtained data. Particular sites considered for reliable medical journals include EMBASE (which has over 29 million records), MEDLINE (which has more than 22 million biomedical pieces), PsycINFO (with over 3.5 million medical journals), Cochrane Database of Systematic Reviews (CDSR), Medline Plus, PubMed, Ovid, Web of Science, Science Direct, Scopus, and Google Scholar. All these are rich online archives of health related journals filled with credible health and medical information. Only those articles that were peer reviewed were included. Also, it was required that the articles included be accessible in full text publication. No papers with purchase costs attached were considered. Non-English papers were also left out as the researcher is not conversant with other languages. Additionally, only researches with human patients were considered, bearing in mind that other studies include animal patients.
The main keywords used for the electronic search included: Cemented hip, Hip Arthroplasty, Cemented stem, and Uncemented stem, Total Hip Arthroplasty, Total Hip Replacement, THA survivorship, THR survivorship, THA survival rates, cemented stem durability, and uncemented stem durability. Each search result was then adequately scrutinized to ensure the title and contents matched the inclusion and exclusion criteria. (Do you use these key words separately or combined, if it is combined, you should indicate whether you use ‘and’ or ‘or’)
Data collection method
The research involved the combination of a good number of secondary data sets. This is because of the nature of the research, which involves an exploration of survival rates for patients who undergo total hip replacement with cemented stem in comparison to those who undergo total hip replacement with uncemented stem. The other reason for this is the location of the patients. It would not be sufficient for the current research to focus on one locality. Obtaining data from different countries and nationalities gives a more wholesome picture.
Study Design
Randomised controlled trials (RCT) have been incorporated as this provides randomisation and will remove any biases. RCTs can also be easily analysed with common statistical tools. RCTs are believed to be ‘gold standard’ in assessing the usefulness of intervention. When comparing cemented and uncemented stems a number of single / multi RCTs have been reported. A number of joint registries were used from Sweden, Norway, England, Wales, Northern Ireland and New Zealand as it provided data that was done on a large scale and compliments to the RCTs.
Inclusion Criteria
The patients ranged from 18 to 100 years of age had undertaken primary total hip replacement due to osteoarthritis, either use cemented or uncemented fixation will be included in this study. The research will also focus on those patients who are admitted to hospital in pain due to cracks in their femoral neck and are in great need of hip replacement. Also included were those patients who expressed their willingness to participate in the various studies for six months and above. It was also a requirement that the patients come from independent dwelling situations. Lastly, the patients included should not be suffering from dementia.
Exclusion Criteria
Patients that had other bone pathologies such as rheumatoid arthritis, trauma and development dislocation of the hip (DDH) etc, or had revision total hip replacement, or with underline diseases such as cardiovascular disorder which could affect their daily activities, or the age beyond the range will be excluded to this study. Also, patients who exhibited difficulties in understanding the objectives of the study were excluded. Patients suffering dementia were not considered for this research. Patients with a serious case of obesity, i.e. with a body mass index of more than 30, were not included in the research.
Evaluation of risk of bias and quality assessment of included studies
To avoid bias, the triangulation method was used , which involves analysis of multiple sources of data to support the interpretations done. This way, it makes the findings more legitimate. For quality purposes, a total of 80 journals were first shortlisted. This list was further thinned down to the top 7 significant studies that will meet the objectives of the current research.
Data extraction and management
Each study eligible for the research was identified using the surname of the first author, the first three words of the title and the year in which it was published. This was solely handled by the researcher.
Results
The previous chapter discussed in detail the methods used for data collection and the reason why the methods settled on were the best for the research. This chapter presents the findings of the research in accordance to the previously-mentioned methods.
Identified studies
Aa total of 100 eligible researches were shortlisted, ensuring there was no duplicate. The doi served as a reliable check for the uniqueness of each study, without necessarily going into the details of the authors and titles. These papers were further scrutinized individually to ensure they conformed to the current study’s inclusion and exclusion criteria. 30 papers were shortlisted from the first elimination round. These were further checked for quality and relevance to the study, and the best 10 were picked for use in the research. The flowchart below illustrates the process by which the entire 100 studies were identified and trimmed down to the 10 most relevant.


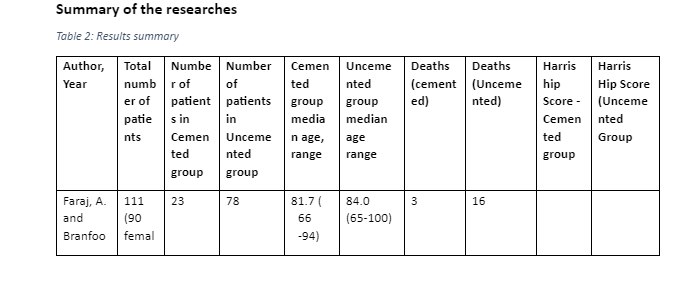
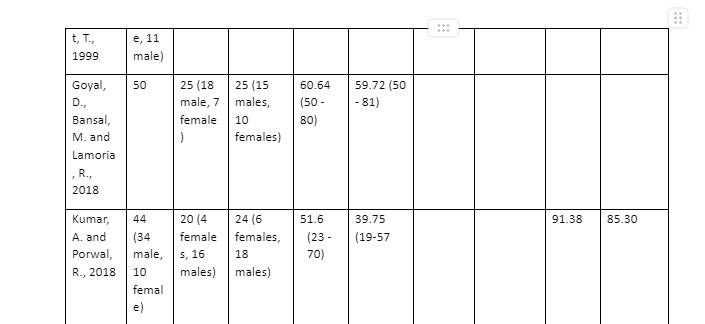

One of the studies focused on only those patients younger than 55 years (Morshed et. al., 2007). One study concentrated on the New Zealand Joint Registry (Wyatt et.al, 2014). The study that covered the largest number of regions was the one by Zhang, Yan, and Zhang (2017), given it includes patients from Sweden, Australia, Norway, New Zealand, and England-Wales,
Excluded studies
A total of 70 potential studies were excluded because they failed to fully satisfy the inclusion criteria for the research. Ten of the shortlisted papers included patients over 100 years old. 5 included dementia patients as part of the sample. 15 required monetary donations in exchange for the full text. 3 were currently underway during the time of the research, and therefore could not be included. A further 10 were excluded because the data was not of adequate quality in the researcher’s judgement.
Discussion
The fundamental aim of this research study was to investigate secondary data and find out the better stem fixation method between cemented and uncemented in patients above the age of 18 years who have undergone total hip replacement. Through the research, the discussion whether uncemented stem is better than cemented will be placed into perspective considering factors such as the number of patients undergoing either cemented or uncemented implants, survivorship of the hip after the surgery, cost-effectiveness, mortality rate, chances of revision of primary surgery, functionality, and the preferred age for the different fixations. The various reasons why Total Hip Replacement is done include to relieve pain, and restore functionality of the damaged, diseased, or fractured hip. This chapter will discuss the major findings from the secondary data used to compare uncemented stem and cemented stem and determine which one is better for total hip arthroplasty. Even though there are many factors to consider in selecting the best type of stem fixation method, this study will focus on the survivorship of the stems in terms of mortality and survival rate after surgery. Survival of the stems
Survival of the stems
Survival rate in this study refers to the time period the implanted stem can survive in the body of an individual without complications after the primary THR has been done. From the sources used for this study, survivability rate of the stem depends on the type of stem fixation used as some survive for longer than others. Goyal et al., (2018), Morshed et al. (2009), Wyatt et al. (2014), Zhang et al. (2017) investigations on the superior technique between cemented and uncemented prothesis found out that their survivorship depended on the age the process was performed on. The survival rate for cemented stems was estimated to last for more than 8 years without any revisions. For the cemented prothesis to survive longer, it had to be done on older patients usually above 65 years as it worked well with their poor bone density. The level of survivorship of cemented stems on younger patients below the age of 65 years was very low and presented various complications earlier. Wyatt et al. (2014) and other studies used explained that uncemented stems were created to counter or address the complications caused by cemented implants on younger patients. For that reason, Loppini and Grappiolo (2018) analysed various secondary sources and came up with a list of short uncemented stems which were Collum femoris preserving, Metaphyseal total hip arthroplasty, Mayo, Proxima, Nanos, Tri-lock bone preservation system, Global Tissue Sparing, Fitmore, Radiostereometric analysis, Einzel-Bild-Röntgen-Analyse femoral component analysis, and Dual energy x-ray absorptiometry analysis. Using the mean Harris hip score, the level of thigh pain experienced, as well as the stem revision at the end of the survival period of the stem, the study concluded that the survivorship rate of all the uncemented stems was ranging between 96-100% when used with appropriate surgery. Most of the aforementioned uncemented hemiarthroplasty survived between 4 to 8 years and were revised to cemented during the second prothesis.
Factors that promote the survivorship of the prothesis stems
Age of the patient
In most of the studies used in this study, the most common factor in selecting either cemented or uncemented to deal with fractured diseased or damaged hips has been age. In the first study the mean age was 83 years, 60 for the second, 45years for the third study, 70 for the sixth, while others used secondary data that concentrated of people above the age of 50 years. From the different studies, it is evident that most patients above the age of 65 years use the cemented hemiarthroplasty to fix their hip problems while the uncemented has been used more on patients under the age of 65 years. Other studies like for Wyatt et al (2014) showed that cemented works better for patients over the age of 70 years. Studies such as Faraj and Branfoot (1999), Wyatt et al (2014), Morshed et al. (2009), Goyal et al. (2018), and Yang et al. (2019) reported that uncemented stem fixation works better for the young patients mostly below 65 years because of the condition of their bone quality. Wyatt et al. (2014) investigation on the European registry and the New Zealand’s Joint registry confirm that cemented hemiarthroplasty is good for patients older than 70 years because of their poor bone density. From the discussion, it is clear that for the hemiarthroplasty stems to survive their intended survival period to revision, determining the age of the patient is essential. The cemented stems will last for longer or survive their intended period in patients that are older. Studies differ in the minimum age to give the cemented stem but the most considered and investigated age appropriate for the survival of the cemented stems is above 65 years. Given the fact, that most studies mentioned that cemented stems had serious negative implications on the younger patients thus the formation of the uncemented, it is clear that the uncemented stems will survive their intended period of between 4 to 8 years before revision in younger patients below the age of 65 years because of their good bone quality and need form more motion activities.
Aspects that hinder survivorship of the prothesis stems
When the stems are revised before their intended survival time, they are considered to have failed. According to study 5 which was an investigation carried out by Morshed et al. (2009), failure is revision of either the cup or stem using uncemented or cemented THA done before the survival time of the stem is due to complications or post-surgery problems. Wyatt et al. (2014) study also defines failure of uncemented or cemented fixation as the revision for primary prothesis. From the two studies, higher rates of failure are observed in younger patients when cemented stems are used while lower rates of revisions are recorded in patients under the age of 55 years when the uncemented stems are used. Zhang et al. (2017) agrees with Wyatt et al. (2014); and Morshed et al. (2009) by noting that most research studies on cemented and uncemented stems investigate revision-related risks before appropriating which method is better than the other. The study concludes that the revision rate for cemented stems was much less than that of the uncemented stems and the rate has been reducing further since 2005. It was well noted that repeated operations or revising of implants cannot be done where there is evidence of superficial or deep infection, on symptomatic or radiographically loose stems. Therefore, when either the cemented or uncemented stem does not reach its intended time after surgery, it is considered to have failed due to the following reasons that hinder stem survival:
Complications Associated with either Cemented or Uncemented THA
Failure or revision of primary Total Hip Arthroplasty that used either prothesis techniques is due to complications that are noted after the surgery or hip replacement procedure. Most studies used in this research work cited different types of problems observed during or after hemiarthroplasty procedures or total hip replacement which are obstacles to the survival of either stems.
Study one by Faraj and Branfoot (1999) discovered that after hemi-arthroplasty some patients can experience different forms of complications including prothesis dislocation and pain which were associated with the level of femoral cut in the fixation procedure. From the research, patients that had uncemented prothesis could experience dislocated prothesis as early as 3 months and had persistent thigh and hip pain. Though their replaced hip function, the pain could still be felt with uncemented stems. For the cemented stems, they healed faster and had greater comfort implying less pain after the surgery. Faraj and Branfoot (1999) concluded that uncemented prothesis has high rate of complications. The second research study used which is by Goyal et al. (2018) divided the complications they observed into during and after surgery. After surgery patients the major complications noticeable on patients with uncemented and cemented stems were aseptic loosening and late appearance of periprosthetic osteolysis. During the surgery, patients that were given cemented implants lost more blood than the ones with uncemented fixations. Goyal et al. (2018) settled that uncemented stems have higher rate of complications are revisions while cemented fixations healed faster and the hip-thigh pain subsided earlier but the foot could drop during surgery. Another comparative study of Kumar and Porwal (2018) noted that uncemented stems had complications such as shortening of the hip, pain, redness of upper lateral thigh, and swelling. Loppini and Grappiolo (2018) also cited hitches relative to uncemented stems to include stem malalignment, incorrect stem sizing, and intra-operative fracture. Morshed et al. (2009) that defined failure of the uncemented or cemented prothesis as revisions or repeated surgery, highlighted the complications that led to the revisions to include aseptic loosening or mechanical failure of the stem which was higher in uncemented fixations. Another study that investigated complications as one of the factors to determine when choosing the best prothesis between uncemented and cemented was by Prashanth and Niranjan (2017). From their study, some of the patients with cemented prothesis had either superficial or deep infections after surgery, shortened stem, and external rotation deformity. Some of the patients with uncemented stems also experienced similar post-operative problems. Furthermore, Thiagarajan (2020) also noted the rate of post-operative problems that patients with uncemented or cemented implants showed. The number of uncemented patients with avascular necrosis, fracture neck, fracture dislocation, periprothesis fracture, infected bipolar, arthritis, and displaced DHS were higher than those with cemented stems considering the equal participants of each group. Study 8 that was done by Wyatt et al. (2014) added acetabular problems and femoral fracture as the reasons for early revision. Last but not least, is the pain mentioned by Zhang et al. (2017). With this analysis in mind, it is evident that cement less stems have higher risks of complications compared to the cemented fixations thus the higher revision risks with uncemented THAs. All the mentioned complications result to the failure of the stems and most cases the surgeries are repeated thus hindrances to the survival of the stems to their intended time. The studies show that the rate of complications is higher in uncemented stems than in the cemented stems hence prove that most cemented prothesis achieve their survival period before revisions unlike the uncemented.
Survivorship of the patients during or after surgery or Mortality Rate
Surgeries are considered risks to life that a patient can either survive or die. Survivorship of the patients that underwent hemiarthroplasty or THR was also investigated in the selected studies. Out of the ten studies explained, only two mentioned death of patients. From the first study by Faraj and Branfoot (1999) 16 patients that underwent uncemented prothesis died and 3 that had cemented THR. Prashanth and Niranjan (2017) is the other study that cited the number of patients that died after one year of primary stem implantation which could have been prothesis related as two died of myocardial infarction, another due to bronchopneumonia, and the other from a road accident. Stroke, heart attack, and pneumonia are considered long-term side effects of the type of anesthesia used during the surgical procedure. It is evident that the mortality rate of uncemented and cemented prothesis is low and risks such as deep infection and high loss of blood during the cemented surgery can lead to death of patients thus the need for higher caution by the surgeons during the procedure. Loppini and Grappiolo (2018) pointed out the need for appropriate surgical procedure in reducing complications and increasing the chances of survival for both the patient and the uncemented or cemented stems. The orthopedic surgeon must understand the potential risks and benefits of the two prothesis as they are the ones to give the patients the best advice on which one will work better on them to prevent complications that can result to death of the patient and early revision of the used stems.

References
- Faraj, A. and Branfoot, T., 1999. Cemented versus uncemented Thompson's prostheses: a functional outcome study. Injury, 30(10), pp.671-675.
- Goyal, D., Bansal, M.and Lamoria, R., 2018. Comparative study of functional outcome of cemented and uncement ed total hip replacement. Journal of Orthopedics, Traumatology and Rehabilitation, 10(1), p.23.
- Kumar, A. and Porwal, R., 2018. Evidence of Efficacy of Cemented Versus Uncemented Fixation with Respect to Functional Outcome; A Comparative Study. Annals of International medical and Dental Research, 4(2).
- Loppini, M. and Grappiolo, G., 2018. Uncemented short stems in primary total hip arthroplasty. EFORT Open Reviews, 3(5), pp.149-159.
- Morshed S, Bozic KJ, Ries MD, Malchau H, Colford JM., Jr Comparison of cemented and uncemented fixation in total hip replacement: a meta-analysis. Acta Orthop 2007;78:315-326.
- Prashanth, Y., 2017. Comparative Study of Surgical Management of Fracture Neck of Femur with Cemented Versus Uncemented Bipolar Hemiarthroplasty. JOURNAL OF CLINICAL AND DIAGNOSTIC RESEARCH,.
- Thiagarajan, P., 2020. Assessment of Functional Outcome between Cemented and Uncemented Total Hip Replacement: A Comparative Study. International Journal of Contemporary Medical Research [IJCMR], 7(1).
- Wyatt, M., Hooper, G., Frampton, C. and Rothwell, A., 2014. Survival outcomes of cemented compared to uncemented stems in primary total hip replacement. World Journal of Orthopedics, 5(5), p.591.
- Yang, C., Han, X., Wang, J., Yuan, Z., Wang, T., Zhao, M. and Han, G., 2019. Cemented versus uncemented femoral component total hip arthroplasty in elderly patients with primary osteoporosis: retrospective analysis with 5-year follow-up. Journal of International Medical Research, 47(4), pp.1610-1619.
- Zhang, C., Yan, C. and Zhang, W., 2017. Cemented or cementless fixation for primary hip arthroplasty—evidence from The International Joint Replacement Registries. Annals of Joint, 2(10), pp.57-57.
Continue your exploration of Black Minority Ethnic Women Experiencing Domestic Violence in Uk with our related content.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



