Managing Acute Exacerbation of Stage 4 COPD
Care Plan
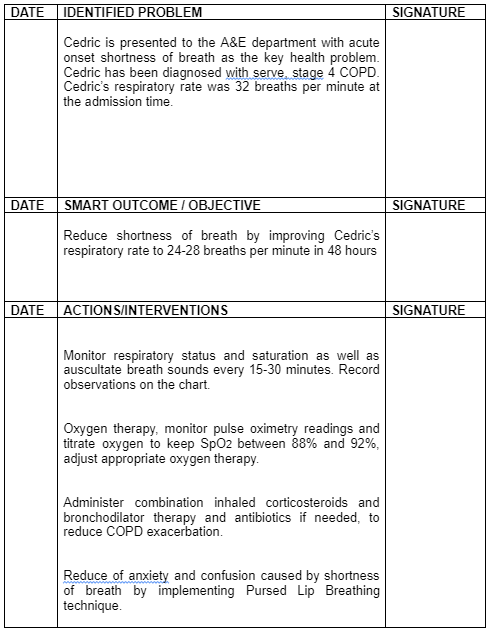
Cedric is 75-years-old male individual admitted to the A&E department with acute onset shortness of breath problem. He has been diagnosed with serve stage 4 COPD. Chronic obstructive pulmonary disease is a lung disease described as a chronic limitation of lung airflow that affects breathing and is not fully reversible (World Health Organisation 2013). British Lung Foundation (2020) data estimated 1.2 million people are living with diagnosed COPD and it is the 2nd most common lung disease in the UK after asthma as nearly 115,000 are diagnosed with COPD each year. For healthcare dissertation help, this case study is going to provide the most valuable insights into COPD management and the major challenges faced by patients such as Cedric.

Cedric is an ex-smoker who quit smoking a year ago. Smoking is the main trigger of COPD in countries with high and middle income (WHO 2013). Cedric acute exacerbation of COPD with onset shortness of breath is very dangerous to his life that means medical intervention along with hospitalisation is required. Reduction in shortness of breath will be achieved by reducing the respiratory rate to 24-28 breath per minute in 48 hours. To achieve the SMART goal four main interventions will be taken, monitoring of patient condition regularly and record into a chart. Oxygen therapy would be implemented. Administer combination inhaled corticosteroids, bronchodilator therapy and antibiotics if needed. Reduce of anxiety and confusion caused by shortness of breaths by implementing Pursed Lip Breathing technique.
The SMART goal aims to reduce Cedric exacerbation of COPD, by improving his breathing pattern in 48 hours. Following NICE (2018) pathway Cedric would be admitted to the hospital ward, so changes in his health condition would be easily measurable in hospital settings. Observation of his respiratory status, breathing sounds, and saturation would clarify Cedric's response for interventions taken. Furthermore, Pulse oximetry and atrial blood gas assessment is to be used as intervention in monitoring health of Cedric regarding SOB (NICE 2018). Following interventions mentioned in the introduction, the goal should be achieved in 48 hours during hospital admission.
Patient's assessment must be performed as the first action to follow The Nursing Process, the assessment will support a nursing diagnosis and will be crucial to understand Cedric condition and set the SMART goal. Furthermore, observation and monitoring the patient's condition is a part of evaluation care helps to record patient's health changes, choose interventions needed as well as assess the accuracy of interventions taken (Hill 2018). Future observation and recording on the chart of respiratory status and saturation every 15-30 min, as well as auscultate breath sounds every 15-30 min, would be continued until the SMART goal's achieved, as significant changes to the patient condition can be observed, such as respiratory rate changes (NICE, 2018).
Cedric's respiratory rate was 32 breaths per minute at the admission time whereas normal respiratory rate should oscillate between 12-20 breath per minute. Although we know the normal respiratory rate, that cannot be applied to Cedric with his chronic respiratory condition, as he would not be able to achieve it. Evidence suggests that reduce the respiratory rate to < 25 breath per minute significantly decreasing the risk of hyperventilation and breathless for a patient (Resuscitation Council UK, 2015). However, for people with stage 4 COPD, like Cedric, we are looking to reduce the respiratory rate to 24-28 breath per minute. (Swearingen and Wright 2019). Also, Potter et al. (2019) identify that observation helps the nurse to compare the effect of interventions with goals and outcomes. Therefore, the observation of Cedric's breathing efficiency is to be used as a measure for determining effectiveness of provided treatment and to what extent the SMART goals are achieved.
The mechanism of forced Oxygen Therapy in COPD patients includes creating a forced flow of oxygen into the lungs to resolve a shortage of oxygen in the bloodstream. In this process, oxygen at 24% is provided at 2-3L/min or oxygen at 28% is provided at 1-2 L/min via a venturi mask to the patient (Pilcher, 2019). The forced technique is applied to COPD patient because shortness of breath (SOB) in them makes the patient unable to naturally breathe in increased amount of required oxygen from the air. The forced oxygen therapy leads to create increased oxygen content in the body of the COPD patients and helps to meet lack of oxygen created in the muscles and body as a result of SOB. This action of reducing raised oxygen demand to normal leads the COPD patient to breathe nearly at normal rate and overcome SOB (Vogelsinger et al., 2017).
The Pulse oximetry is to be used for monitoring the blood oxygen level of Cedric after administration of oxygen therapy. Moreover, to receive information regarding PaCO2, PaO2 or blood PH, the atrial blood gas assessment is to be made as the pulse oximeter do not provide the reading regarding the aspects. The normal parameter of PaCO2 is 35-45 mmHg, 75-100 mmHg for PaO2 and pH of 7.35-7.45 (Martin et al., 2016). The factors to be considered in COPD patient while providing them artificial oxygen is the oxygen saturation level in their blood and to ensure it remains more than 90% which is normal value (Pavlov et al., 2018). These parameters are to be achieved through oxygen therapy provided to Cedric within 48 hours. It is able to be achieved as an increased flow of oxygen in the therapy would gradually raise the blood oxygen level which in turn reduces the carbon dioxide content in the bloodstream, making the blood become more alkaline out of lower presence of CO2 which is acidic in nature (Branson, 2018). The time taken by the body for initiating the impact of oxygen therapy is immediate and gradual. Therefore, it can ensure that by within 24-48 hours with continuous impact of oxygen therapy to increased blood oxygen level would help Cedric overcome shortness of breath while supported with other therapies or medication.
The bronchodilators are considered as the backbone for the treatment of respiratory exacerbations in COPD patients (Roberts et al., 2020). This is because shortness in breath is experienced by the COPD patients due to blocked airways by the presence of increased sputum that resist free airflow into the lungs. However, the bronchodilators act to dilate the reduced airways in turn lowering airflow resistance which leads the patients to overcome shortness of breath and gradually develop normal breathing (Roberts et al., 2020). According to NICE (2018), short-acting bronchodilator such as salbutamol 5mg short-acting β₂ agonist (SABA) should be delivered via a nebulizer in the hospital setting. This is to be provided to Cedric for resolving his shortness of breath within 48 hours because the bronchodilators initiate to act immediately as its described mechanism by dilating airways and continue its effect for 2-4 hours in the body (Almadhoun and Sharma, 2020). Thus, it repeated use within the 48 hours would help to gradually normalise the shortness of breath whenever exacerbation occurs.
Pulmonary rehabilitation is beneficial for patients in any stage of COPD because the technique leads to remove the trapped air in the lungs by slowing the breathing rate and enhancing the patient to overcome shortness of breath. The technique causes the airways to be opened for longer and allows increased oxygen to be flow in and carbon dioxide to the breathed out from the lungs (Sundh et al.2017). The Pursed Lip Breathing technique is to be introduced as a part of pulmonary rehabilitation for Cedric. This is because SOB in COPD patient may also be caused by too much of air present in the lungs, in turn, decreasing the amount of place left for extra air to enter lungs and support breathing (Yang et al., 2020). In this condition, pursed lip breathing technique is implemented in which the increased trapped air is released. It leads to create room in the lungs for breathing, in turn, resolving SOB in COD patients (Yang et al., 2020).
Cedric’s daughter Tracy should also be involved in those sessions as she is his carer. This is because it would help her to understand the way to be cared for Cedric after release from the hospital so that further exacerbation of SOB is not experienced by him. The nurse will teach Cedric Pursed Lip Breathing technique, which involves lightly pursing the lips together during controlled exhalation, its aimed at patients with COPD and Asthma by teaching them on how to compile with episodes of dyspnoea. It is able to be achieved by the end of 48 hours when he has developed enhanced breathing as it is rehabilitation technique for Cedric. Those sessions will help Cedric to improve ventilation and releases trapped air also will keep airways open longer and slowing the respiratory rate by prolonging exhalation. Working in partnership with pulmonary rehabilitation team in Cedric care would be an example of integrated care which aim to benefit a person in care by receiving care from different care provides those sessions could be continued in the future to prevent exacerbations of COPD ( Monitor 2015, The Code 2015).

The above discussion mentions that Cedric is a stage-4 COPD patient who ha been admitted to the A&E department of the hospital with the help health raised to be shortness of breath (SOB). In order to understand the impact of intervention for SOB management in Cedric for next 48 hours, the breathing rate and oxygen saturation level in the blood is to be monitored through pulse oximeter and arterial blood gas measurement. In the initial stage, Cedric is to be provided forced oxygen therapy so that the oxygen lag created due to SOB in the body is resolved. Moreover, with lowering of the demand of oxygen in the blood followed by escape of air through the forced action from the lungs would create space for more air to enter the lungs and help him breathe in turn resolving his SOB. The bronchodilators are to be administers to allow more oxygen to enter the lungs and resolve SOB in COPD. In rehabilitation care for Cedrick, he is to be educated regarding the way o performed pursed lip breathing in resolving SOB rise in future.
References:
- Almadhoun, K. and Sharma, S., (2020). Bronchodilators. StatPearls. pp.20-34. Available at: https://www.ncbi.nlm.nih.gov/books/NBK519028 [Accessed on 7 September 2020]
- Branson, R.D., (2018). Oxygen therapy in copd. Respiratory care, 63(6), pp.734-748. https://rc.rcjournal.com/content/respcare/63/6/734.full.pdf [Accessed on 7 September 2020]
- British Lung Foundation (2020); Chronic obstructive pulmonary disease (COPD) statistics available at:
- Hill, R. (2018) Assessment, Planning, Implementation and Evaluation (APIE): The Process of Nursing IN Delves-Yates, Essentials of Nursing Practice, 2nd edn. London: SAGE
- https://statistics.blf.org.uk/copd?_ga=2.15302006.1317978988.1594487389-1028033020.1594487389 Swearingen, P., Wright, J. (2019); All in One, Nursing Care Planning Resource 5th edition. Elsevier, Missouri.
- Hurst, J.R (2011) "Exacerbation Phenotyping in Chronic Obstructive Pulmonary Disease." American Journal of Respiratory and Critical Care Medicine, 184(6), pp. 625–626. Available at: https://doi.org/10.1164/rccm.201106-1136ED Published: 15 September 2011
- Martin, Ş.A., Tomescu, V. and Voidăzan, S., (2016). Secondary elements of blood pH variation can influence the effort effectiveness based on adaptive changes within a group of elite athletes. Clujul Medical, 89(4), p.506. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5111491/ [Accessed on 7 September 2020]
- Monitor (2015) Delivering better integrated care. Available at: https://www.gov.uk/guidance/enabling-integrated-care-in-the-nhs
- NICE (2018); Chronic obstructive pulmonary disease in over 16s: diagnosis and management, NICE guideline [NG115] Published date: 05 December 2018 Last updated: 26 July 2019, available at: https://www.nice.org.uk/guidance/ng115
- NICE (2020); Oxygen, Available at: https://bnf.nice.org.uk/treatment-summary/oxygen.html
- Nursing & Midwifery Council (2015) The Code professional standards of practice and behaviour for nurses, midwives and nursing associate. Professional standards of practice and behaviour for nurses, midwives and nursing associates Available at: https://www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf Accessed 29 January 2015.
- O'Driscoll, B. Howard, L. Earis, J. Mak,V. (2017); BTS guideline for oxygen use in adults in healthcare and emergency settings; Thorax 2017;72:ii1-ii90
- Pavlov, N., Haynes, A.G., Stucki, A., Jüni, P. and Ott, S.R., 2018. Long-term oxygen therapy in COPD patients: population-based cohort study on mortality. International journal of chronic obstructive pulmonary disease, 13, p.979. Available at: https://www.dovepress.com/long-term-oxygen-therapy-in-copd-patients-population-based-cohort-stud-peer-reviewed-article-COPD Accessed on 27 November 2020]
- Pilcher, J., 2019. High concentration oxygen and hypercapnia in respiratory disease. Victoria University of Wellington. 2019. pp.20-34. Available at: https://researcharchive.vuw.ac.nz/xmlui/bitstream/handle/10063/8057/thesis_access.pdf?sequence=1 Accessed on 27 November 2020]
- Pisani, L., Fasano, L., Corcione, N., Comellini, V., Musti, M.A., Brandao, M., Bottone, D., Calderini, E., Navalesi, P. and Nava, S., (2017). Change in pulmonary mechanics and the effect on breathing pattern of high flow oxygen therapy in stable hypercapnic COPD. Thorax, 72(4), pp.373-375. Available at: https://thorax.bmj.com/content/thoraxjnl/72/4/373.full.pdf [Accessed on 7 September 2020]
- Potter, P., Perry, A., Stockert, P. & Hall, A. (2019) Essentials for Nursing Practice. 9th edn. Elsevier.
- Resuscitation Council UK (2015); available at: https://www.resus.org.uk/library/2015-resuscitation-guidelines/abcde-approach
- Roberts, M.H., Mapel, D.W. and Petersen, H., (2020). Comparative Causal Analysis of the Effects of Long-Acting Muscarinic Antagonist Versus No Long-Acting Bronchodilator Use on Readmission or Mortality After Hospitalization for Chronic Obstructive Pulmonary Disease. Drugs-real world outcomes, 7(1), pp.1-17. Available at: https://link.springer.com/article/10.1007/s40801-019-00171-w [Accessed on 7 September 2020]
- Sundh, J. Lindgren, H Hasselgren, M Montgomery, H Janson, C Stallberg, B (2017) Pulmonary rehabilitation in COPD--available resources and utilization in Swedish primary and secondary care. International Journal of Chronic Obstructive Pulmonary Disease, vol. 12, 2017, p. 1695+.Available at: https://go-galecom.ezproxy.bcu.ac.uk/ps/i.do?p=AONE&u=uce&id=GALE|A531988296&v=2.1&it=r&sid=summon. Accessed 23 Aug. 2020
- Tobias Welte, Marc Miravitlles; European Respiratory Journal 2014 44: 11-13; DOI: 10.1183/09031936.00041914; available at: https://erj.ersjournals.com/content/44/1/11 ;Published online June 30, 2014
- Vogelsinger, H., Halank, M., Braun, S., Wilkens, H., Geiser, T., Ott, S., Stucki, A. and Kaehler, C.M., 2017. Efficacy and safety of nasal high-flow oxygen in COPD patients. BMC pulmonary medicine, 17(1), p.143. Available at: https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-017-0486-3 Accessed on 27 November 2020]
- Waugh, A. Grant, A. (2018) Ross & Wilson Anatomy and Physiology in Health and Illness, 13th Edition, Elsevier Ltd.
- Wedzicha, J.A., Miravitlles, M., Hurst, J.R., Calverley, P.M., Albert, R.K., Anzueto, A., Criner, G.J., Papi, A., Rabe, K.F., Rigau, D. and Sliwinski, P., (2017). Management of COPD exacerbations: a European respiratory society/American thoracic society guideline. European Respiratory Journal, 49(3). pp.34-67. Available at: https://erj.ersjournals.com/content/erj/49/3/1600791.full.pdf [Accessed on 7 September 2020]
- Westphalen, D., (2019), What to know about inhaled steroids, Available at: https://www.medicalnewstoday.com/articles/325666 [Accessed on 7 September 2020]
- World Health Organization (2013); What is chronic obstructive pulmonary disease (COPD)? available at: https://www.who.int/news-room/q-a-detail/what-is-chronic-obstructive-pulmonary-disease-(copd); Published 8 October 2013
Looking for further insights on Lifecourse Approaches in Health Social Care and Ageing? Click here.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



