What are The Vascular Complication in Diabetes
Abstract
Background: Diabetes mellitus (T1DM) is a condition that occurs when the pancreatic cells that produce insulin are destroyed; hence the body is unable to make insulin. Due to a lack of insulin in the body, glucose remains unprocessed. On the other hand, vascular complications are pathological conditions that arise from diabetic conditions. They are classified into macro and micro complications. Biomedical science dissertation help is said to be crucial for students regarding researching topics such as the emergence of vascular complications in the context of diabetes. Objectives: The primary purpose of this review is to different vascular complications that arise from diabetes. Another objective is to identify the prevalence and factors predictive of vascular complications in young adults with diabetes. Methodology: These 12 reviews that deal with the emergence of vascular complications of diabetes were selected using the PRISMA reporting system. Their analysis was done using the critical appraisal tool. Findings: The results of this study determined that there indeed are vascular complications that are associated with diabetes. These complications were divided into two types, microvascular and macrovascular complications. Microvascular complications are long term complications inclusive of retinopathy, nephropathy and neuropathy. Macrovascular complications include coronary heart diseases, peripheral artery diseases and cerebrovascular diseases. Different clinical studies have proved a connection between diabetes and vascular diseases; however, there are other risk factors present in diabetic patients, such as hypertension and obesity. Conclusions: Diabetes mellitus results in various vascular complications through different pathogenesis pathways, such as insulin resistance. The connection between Diabetes and vascular complications is apparent; however, more clinical studies are required to identify the pure effect of DM.

CASP Critical Appraisal Skills Programme
T1DM Diabetes Mellitus>
NICE National Institute for Health and Care Excellence
WHO World Health Organization
ADA Adenosine Deaminase
UK United Kingdom
PRISMA Preferred Reporting Items For Systematic Reviews And Meta-Data Analysis.
T2DM Type 2 Diabetes Mellitus
GDM Gestational Diabetes Mellitus
ACE Angiotensin-converting enzyme
UKPDS United Kingdom Prospective Diabetes Studies
ACCORD Action to Control Cardiovascular Risk in Diabetes
ACEI angiotensin-converting enzyme inhibitor
ADVANCE Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation
DCCT Diabetes Control and Complications Trial
DIAD Detection of Ischemia in Asymptomatic Diabetics
FIELD Fenofibrate Intervention and Event Lowering in Diabetes
FREEDOM Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease
MI myocardial infarction
PAD peripheral artery disease
PCI percutaneous coronary intervention
PLATO Platelet Inhibition and Patient Outcomes
PRoFESS Prevention Regimen for Effectively Avoiding Second Strokes
SPRINT Systolic Blood Pressure Intervention Trial
SYNTAX Synergy Between PCI With Taxus and Cardiac Surgery
UKPDS United Kingdom Prospective Diabetes Study
VTE venous thromboembolism
Introduction
Diabetes is a metabolic disorder that presents with hyperglycemia due to defects in the secretion of insulin from the pancreas. Insulin is a hormone in the human body that works by helping the body cells in using the available sugar (Piardi et al, 2016). Absence of this hormone makes the body unable to use this glucose hence leaving too much glucose circulating in the blood stream (Zaharieva et al., 2017). Microangiopathy is the major cause of death in patients with diabetes. This condition is referred to as diabetic microangiopathy and its pathogenesis is far from clear and the mechanisms that cause it are unknown and in most cases it has been linked to genetics (Chiang et al., 2014). This condition occurs by thickening of the capillary basement membranes. Diabetes has a range of micro vascular complications which include retinopathy, nephropathy and neuropathy. Inadequate insulin in adolescents children as the first signs and symptoms manifest during this time (Chiang et al., 2014). The pathologic hallmark of the condition is associated with vasculature that contributes to microvascular and microvascular complications (Donaghue et al., 2018). Besides, there has been an association between the chronicity of hyperglycemia and the long term damage as well as the failure of various organ systems such as the kidneys, heart, eyes as well as the nerves (Chiang et al., 2014). Kidney diabetes occurs when blood vessels in the kidney are injured hence failure of this organ to clean blood properly. This results in ankle swelling and weight gain as the body retains a lot of salt and water than the normal range (Diabetes UK, 2016). Damaging of nerves in the body causes difficulty in emptying of the bladder. Infections arise as a result of this failure as urine remains in the bladder for a long time. Research has shown that about 30% of patients with diabetes eventually suffer from kidney failure. In people with juvenile the nephrons slowly thicken and become scarred with time (Chiang et al., 2014). Hence leading to a condition known as diabetic nephropathy, which is a type of kidney disease (Rossing and Frimdot, 2019). A blur has been reported as much as the line of demarcation between the pathophysiology of microvascular and macrovascular complications of diabetes as well as the therapeutic interventions for the same are concerned (Bjornstad, Donaghue, and Maahs, 2018). Diabetes has been reported to encourage changes in the microvasculature resulting in the protein synthesis of the extracellular matrix. Besides, it leads to the thickening of the basement membrane. These are the pathogenic features of diabetic microangiopathy (Gan et al., 2012). The need to explore and better understand the microvasculature and microvasculature associated with Diabetes is thus inevitable.
Background
Dig deeper into Aspiring for a BSc in Accounting and Finance with our selection of articles.
Based on the seventh edition of the diabetes atlas, diabetes is a major prevalent condition that has been approximated to be around 8.8 of the world population. Besides, there is an expected rise in the number to 13.6% in the next 25 years (Chiang et al., 2014). Globally, reports have indicated that around 193 million undiagnosed diabetes are in existence. They are thus predisposed to develop chronic complications such as chronic hyperglycemia (Songini et al., 2017). The increased prevalence of diabetes globally highlights it as a serious challenge to the health systems. Considering the prevalence of the condition in a global aspect, there has been an estimation of around 490,100 children presumably living with the disease. This has also been estimated to increase by 2.8% in children below 15 years (Chiang et al., 2014). This is a significant issue of concern owing to the mortality and morbidity rates of diabetes across the population. Those diagnosed with diabetes below thirty years tend to have a 4.7 fold excess risk of exposure to mortality (Tonnies et al., 2018). Vascular complications are usually the main cause of early mortality (Piardi et al., 2016). However, there is little research on the prevalence or predictive aspects of diabetes development among children. Hence, identifying the disease complication prevalence or any possible predictive characteristic would be a milestone for benchmarking these risks, assisting healthcare providers in targeting information towards averting the onset of such complications. In a study by Suneja et al., the researchers observed that the prevalence of vascular complications in diabetes had been perceived to result from the consequences of the disordered actions of lipid metabolism enzymes that affect the endothelial function, leading to coagulation, inflammation, platelet activation, and fibrinolysis (2018). With cardiovascular and athero-thrombosis risk factors, a state of progressive and persistent damaging of the vascular walls is created, referred to as macro-angiopathy (Schmidt et al., 2013). In the end, the patient gets the micro-angiopathic disease that is facilitated by hyperglycemia as a primary pathogenic factor. These vascular co-morbid complications include nephropathy due to renal failure and may require kidney dialysis or transplantation, and retinopathy, which causes blindness and reduced vision (Strain and Paldanius, 2018). The latter is in addition to hypertension associated with peripheral, cardio, and cerebrovascular ailment, leading to amputation, stroke, cardiac failure, and sudden death. Unfortunately, young adults might be highly vulnerable to such complications. They demand unique health needs related to their physical, psychological, and socio-cultural life-stage issues (Sivaprasad et al., 2012). Currently, there is a lack of coherence among scholars on the methods of diabetes prevention. However, the diabetes audit done in the UK demonstrated that most of the deaths associated with diabetes could have possibly been prevented through health checks, regular medication, and proper diet (Diabetes-UK 2016). Arguably, from the audit’s result, most diabetic patients are ignorant of the potential dangers and implications that could arise from poor treatment of diabetes, and the majority have taken the issue of adjusting their lifestyle lightly (Sivaprasad et al., 2012). The latter is also supported by most of the studies that have been vocal on proper education for diabetes as one of the key treatment approaches and preventive measures of diabetes generally. Studies have also noted that the incidence as well as the progression of microvascular complications is lowered by intensive glycemic control (Piardi et al., 2016). However, the morbidity that is associated with such conditions has been seeing an increase over the years. Studies like those carried out by the United Kingdom Prospective Diabetes Study (UKPDS) have reported that strict glycemic control has the potential of limiting microvascular disease (Donaghue et al., 2018). However, attempts to improve macrovascular outcomes have yet remained shrouded with controversy as much as the use of glucose-lowering strategies is concerned. In the ten years of follow-up of UKPDS, the organization has noted a relative risk reduction in myocardial infarction associated with diabetes (Sivaprasad et al., 2012). Also, the organization has reported that the risk of cardiovascular mortality, stroke as well as nonfatal myocardial infarction is reduced through pioglitazone in a trial of prospective pioglitazone clinical trial in cases involving macrovascular conditions (Cavender et al., 2015; Schmidt et al., 2013). Much attention has been directed towards the management of macrovascular conditions like stroke and acute coronary syndromes (Tonnies et al., 2018). Besides, vascular complications presents with evidence of pathology in other vascular territories around affected tissues (Gan et al., 2012). There has been an establishment of a linear relationship between microvascular complications and the period the disease lasts. Also, researchers have reported the presence of microvasculopathy in distinct age groups. In other studies, researchers have noted that both microvascular and macrovascular complications develop at the same time in diabetes (Donaghue et al., 2018). This issue is a global health concern thus the study aims to identify the prevalence as well as the predictive factors of vascular complications in young adults living with diabetes. They study also aims to investigate the presence of microvascular complications in patients that are newly diagnosed with diabetes mellitus.
Aims and Objectives
To investigate the pathological instigators of vascular complications in type I diabetes patients To explore the possible interventions for reducing dangers of vascular complications associated with diabetes To explore the relationship between microvascular and macrovascular complications in diabetesRationale
The rationale for conducting this study is based on the seriousness of these vascular complications and the cost that they impact on healthcare systems (Hex et al., 2012). Vascular complications associated with type diabetes have been an issue of great concern thus the need to apt address the issue. The study is thus undertaken to identify the vascular complications of diabetes in United Kingdom. This research papers used in this study clearly informs the topic of research and have been able to deduce that diabetes vascular complications that are long term and greatly affect small blood vessels in the human body most especially the kidney (Piardi et al., 2016). This study is expected to provide new insights into the problem for better management in the quest to ensure patient safety and health outcomes as much as vascular complications in diabetes are concerned.
CHAPTER 2: METHODOLOGY
Research design
This section of the study presents the technique that was used in the identification and gathering of data that was relevant to the topic of study. This is a secondary study that involved review of literature to meet the aims and objectives of the study. This study thus adopted a qualitative research approach. The reason for the choice is based on the advantage in that it enabled reflections on what has already been known or learned during decision making in the research process. Vividly, qualitative approach enable researcher to have a deeper insight and interpret of the phenomena that diabetic patients undergoes, thus could be suitable to understanding some of the risk factors that patients with T1DM faces that exposes them to high prevalence of vascular complications. The qualitative study involved synthesis of literature from various databases, their analysis and presentation of the evidence. The databases that are used are inclusive of PubMed, Medline, Medscape, Research gate, and Ebsco. Keywords are used in searching for relevant studies from the chosen databases. The chosen studies also undergo an inclusion and exclusion criteria before being used in the study. A critical appraisal tool has also been used to critically appraise the chosen studies to assess their quality and eligibility.
Key words
Diabetes Diabetes Emergence Vascular complications Microvascular Macrovascular Complications PatientsInclusion and Exclusion Criteria
The studies that have been used in this systematic review were those that evaluated microvascular and microvascular complications in type 1 diabetic patients and they passed the following criteria:Inclusion criteria
- Studies published in English and within the last ten years
- Studies that reported human data
- Studies that clearly defined diabetes and vascular complications
- Primary studies
Exclusion criteria
- Studies published in languages other than English
- Studies dated more than ten years
Search Strategy
The literature review that was undertaken involved the summary besides the synthesis and critique of studies from the literature search. The databases that were selected were used since they contained many references that were significantly relevant to the topic of study. They were systematically screened by use of MeSH terms as follows: Diabetes (MeSH Terms) OR Diabetes AND vascular complications OR microvascular OR macrovascular AND complications (All Areas) OR diabetes OR patients OR diabetes patients AND vascular complications OR emergence of AND vascular complications AND diabetes AND patients. In addition to the screening, the researchers also undertook a manual search in the quest to look for the mentioned terms in identifying extra studies that could not be retrieved via the initial screening. The reference lists of the identified studies also underwent careful assessment in the quest of ensuring only relevant papers were sourced from the literature search.
Refining and Narrowing of Literature Search
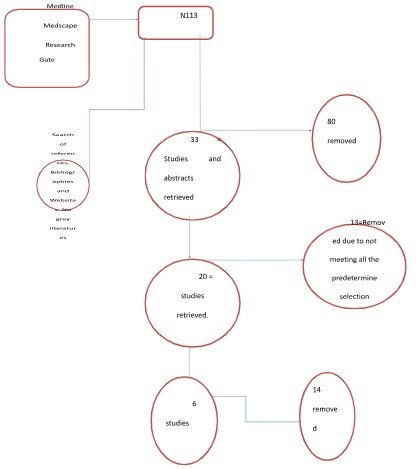
The study collected data in 113 articles in total. However, a systematic evaluation of these articles was done, giving more attention to where the authors addressed the vascular complications and risk factors attributed to diabetes, as well as their stages of development. With this, 80 articles removed since they were duplicates. Of the 33 articles that remained, 13 of them were removed since they did not meet the inclusion criteria. 20 articles them removed and their titles and abstracts as well as the references were reviewed from which 14 articles were removed. 6 articles thus remained and they were critically appraised to ensure their reliability, validity and quality before being used in the research study.
Data Analysis
The data that was identified were thematically analyzed various themes were identified.CHAPTER 3: RESULTS
The themes that came up from the data analysis form the subheadings in the discussion and recommendations chapter
The following studies were identified from the literature search:Bressler, S.B., Qin, H., Melia, M., Bressler, N.M., Beck, R.W., Chan, C.K., Grover, S., Miller, D.G. and Diabetic Retinopathy Clinical Research Network, 2013. Exploratory analysis of the effect of intravitreal ranibizumab or triamcinolone on worsening of diabetic retinopathy in a randomized clinical trial. JAMA ophthalmology, 131(8), pp.1033-1040.
Cavender, M.A., Scirica, B.M., Bonaca, M.P., Angiolillo, D.J., Dalby, A.J., Dellborg, M., Morais, J., Murphy, S.A., Ophuis, T.O., Tendera, M. and Braunwald, E., 2015. Vorapaxar in patients with diabetes mellitus and previous myocardial infarction: findings from the thrombin receptor antagonist in secondary prevention of atherothrombotic ischemic events-TIMI 50 trial. Circulation, 131(12), pp.1047-1053.
Donaghue KC, Marcovecchio ML, Wadwa RP, Chew EY, Wong TY, Calliari LE, et al. ISPAD Clinical Practice Consensus Guidelines 2018: Microvascular and macrovascular complications in children and adolescents. Pediatr Diabetes. (2018) 19 Suppl 27:262–74. doi: 10.1111/pedi.127422017. Diabetes Care. (2018) 41:233–40. doi: 10.2337/dci17-0031
Mi, D., Jia, Q., Zheng, H., Hoff, K., Zhao, X., Wang, C., Liu, G., Wang, Y., Liu, L., Wang, X. and Wang, Y., 2012. Metabolic syndrome and stroke recurrence in Chinese ischemic stroke patients–the ACROSS-China study. PloS one, 7(12), p.e51406.
Stratton, I. M., Adler, A. I., Neil, H. A. W., Matthews, D. R., Manley, S. E., Cull, C. A., ... & Holman, R. R. (2015). Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. Bmj, 321(7258), 405-412.
Tönnies, T., Stahl-Pehe, A., Baechle, C., Castillo, K., Kuss, O., Yossa, R., Lindner, L.M., Holl, R.W. and Rosenbauer, J., 2018. Risk of microvascular complications and macrovascular risk factors in early-onset type 1 diabetes after at least 10 years duration: an analysis of three population-based cross-sectional surveys in Germany between 2009 and 2016. International journal of endocrinology, 2018.
Caldwell’s Critical Appraisal Tool
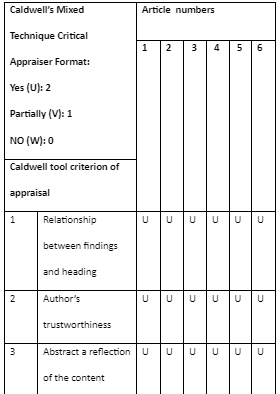
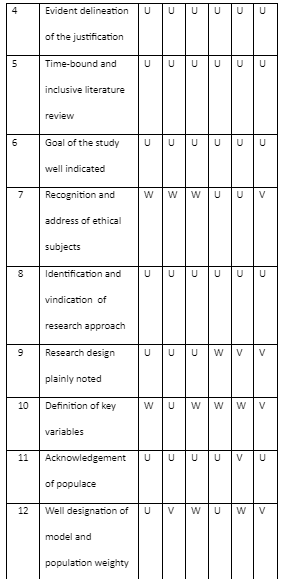
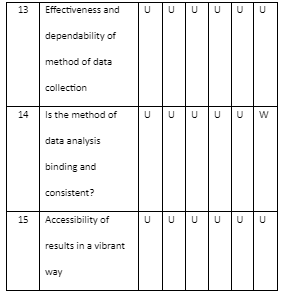
Critical appraisal comments
The quality of the articles was assessed using the Caldwell appraisal tool where a list of criteria was provided. The studies were given values of U, V, and W where U was for yes with a score of 2, V was for partially with a score of 1 while W was for a No with a score of 0. The pass mark was 25 and all the studies qualified for the study.
CHAPTER 4: DISCUSSION AND RECOMMENDATION
This study had identified three major manifestations of microvascular complications in diabetes patients.Retinopathy
According to the study by Stratton et al., the researchers noted that there is a strong association between microvascular disease and hyperglycemia (2015). The researchers’ note that chances of developing retinopathy is 11 times more relative to the increase in chances of developing of coronary artery disease. Diabetic patients are reported to develop evidence of retinopathy even seven years after developing type 2 diabetes thus insulin resistance has a contribution to the same (Stratton et al., 2015). Loss of pericytes has been reported as the earliest signs of retinopathy associated with diabetes mellitus. These are noted to wrap around the arteriolar besides the capillary endothelial cells. Thereafter, there are signs of membrane thickening followed by formation of microaneurysms after permeability of the endothelial cells (Kobyliak et al., 2018). Retinopathy are of two types, namely, the proliferative and the nonproliferative where the latter involves patients developing dot hemorrhages in the middle of the retina as well as signs of retinal edema (Bressler et al., 2013; Lee, Wong, and Sabanayagam, 2015). On the other hand, proliferative retinopathy is characterized by development of neovascularization on the retina with complication of vitreous hemorrhage which has the potential of contribution to vision loss. Retinopathy is quite prevalent. The study notes that 28.5% of diabetic population present with the complication while vision loss has been reported in 4.4% of the population (Kobyliak et al., 2018). In the United Kingdom, diabetic retinopathy has been reported amongst the leading causes of blindness. Fortunately, various treatments have been reported to significantly improve the outcomes. The study notes that systemic medical therapy has had a significant impact in microvascular disease and has been important in reducing the progression to vision loss (Bressler et al., 2013).
Nephropathy
The study also notes nephropathy as a common microvascular complication associated with diabetes (Donaghue et al., 2018). Just like retinopathy, this is also associated with the thickening of basement membrane associated with the formation of microaneurysm. Besides, nephropathy as a result of diabetes has been associated with glomerular hyperfiltration that contributes to expansion of the extracellular matrix and progressing sclerosis of the tubules and the glomeruli. The changes that are caused by nephropathy result in albuminuria (Rossing and Frimdot, 2019). 7% of diabetic patients have been noted to develop diabetic nephropathy. In the most developed states, diabetic nephropathy is the most common form of vascular complication experienced, which causes renal failure in diabetic patients. According to Rossing and Frimodt-Møller (2019), microalbuminuria is the earliest indicator of nephropathy onset. Nephropathy is a kidney damage condition caused by hyperglycemia that leads to renal failure or end-stage renal disease at its worst ends (Songini et al., 2017). On this accord, studies allude that early detection of microalbuminuria would be an excellent opportunity to approach nephropathy with controlled glycemic and blood pressure and could serve as a way to improve the lives of diabetic patients with such complications (Rossing and Frimdot, 2019).
Nephropathy
Unlike retinopathy and nephropathy, neuropathy is regarded as the disturbance of the functioning of the peripheral nerves and is simultaneously linked with the severe symptoms that decrease quality of life (Jaiswal et al., 2017). As mentioned, neuropathy exposes diabetic individuals to foot ulcers that potentially lead to amputation of lower limbs. According to Hicks (2019), some of the main neuropathy symptoms in T1D include loss of sensation, pain, foot ulcers, disorder balancing, and other foot injuries. The main symptoms of autonomic neuropathy include disordered vasomotor functioning, dysfunction of the genitourinary, abnormal perspiration, gastrointestinal motility disorders, and impaired hypoglycemia (Kelkar, 2020). Further, literature alludes that the manifestation of diabetic neuropathy is not very virulent among diabetic children or young youths clinically; however, there is a unanimous increased risk due to poor glycemic control (Jaiswal et al., 2017).
Medical therapy and microvascular Disease
Another study reported the possibility of preventing the profession of microvascular disease via aggressive treatment pf hyperglycemia as well as the treatment of cardiovascular risk factors (Strain and Paldanius, 2018). For instance, as the researchers’ reports, intensive treatment has been associated with 76% reduction in retinopathy development (Donaghue et al., 2018). On the hand, the same has contributed to 43% and 69% reduction in nephropathy and neuropathy respectively (Hicks and Selvin, 2019). Lowering glucose has been demonstrated to be beneficial according to the study by UKPDS. According to a study by Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE), aggressive glycemic control of glucose is important for microvascular infections (Zaharieva et al., 2017). Studies have also reported that controlling blood pressure has the potential of reducing the likelihood of microvascular disease. In a meta-analysis that involved examination of the impact of blood pressure, the researchers noted that it controlled diabetic retinopathy (Donaghue et al., 2018). For instance, better blood pressure contributes to 18% reduction in the occurrence of retinopathy in type 1 diabetes mellitus patients and 22% for those with type 2 diabetes. Studies have also reported that Angiotensin-converting enzyme inhibitors significantly lower the incidence of nephropathy (Rossing and Frimdot, 2019).
Cardiovascular disease
Coronary artery disease
For more than four decades, there has been a link between diabetes mellitus and an increased risk of myocardial infarction (Schmidt et al., 2013). The study also notes that diabetes mellitus is not the only risk equivalent of previous myocardial infarction for a similar case in the future (Cavender et al., 2015). Diabetes thus increases the risk of future myocardial infarction relative to any other risk factor (Cavender et al., 2015). In a case study in the INTERHEART global case, it was noted that diabetes mellitus surged the chances of myocardial infarction in women relative to any other risk factor. In another study that involved nondiabetic patients with coronary disease, an oral glucose test indicated that 18% of the participants had undiagnosed diabetes mellitus while 32% had impaired glucose tolerance (Cavender et al., 2015). Lastly, 5% had impaired fasting glucose. Of all the patients that took part in the study, half had evidence of dysmetabolic condition linked to type 2 diabetes mellitus (Zaharieva et al., 2017). Patients with diabetes mellitus have greater consequences of myocardial infarction relative to those without it (Bjornstad, Donaghue, and Maahs, 2018). Studies have reported that diabetic patients have a 2-fold greater risk of cardiovascular death alongside myocardial infarction or strike relative to individuals who are nondiabetic (Strain and Paldanius, 2018). In a platelet inhibition and patient outcomes (PLATO) trial, it involved a comparison of ticagrelor and clopidogrel in acute coronary patients with diabetes mellitus had a 66% higher risk of developing cardiovascular death alongside MI and stroke (Cavender et al., 2015; Thukkani et al., 2015). The outcomes of diabetic patients are worsened by percutaneous coronary revascularization. Diabetes patients who are asymptomatic have their outcomes not affected by screening for myocardial ischemia or anatomic proof of coronary heart disease though there is a worse cardiovascular prognosis relative to persons who are nondiabetic (Cavender et al., 2015). There is a higher rate of coronary heart disease occurrences in diabetic relative to nondiabetic patients. However, cardiovascular conditions have reduced precipitously over the last twenty years (Strain and Paldanius, 2018). The prevalence of acute MI in diabetes patients has been reported to have decreased by 68% that are associated with frequent use of effective medical as well as strategies for revascularization (Schmidt et al., 2013).
Stroke

There is complexity and difficulty in associating diabetes and the risk of suffering from stroke. In a study conducted by Nurses Health, there was an association between types 1 diabetes mellitus with increased risk of ischemic as well as hemorrhagic stroke (Tonnies et al., 2018). On the other hand, type 2 diabetes mellitus has been associated with a heightened risk of ischemic stroke relative to hemorrhagic stroke (Tonnies et al., 2018). In a survey that involved Asian patients, there was an association between type 2 diabetes and increased risk if ischemic stroke and not hemorrhagic stroke. Studies have also suggested that the risk of strike is more in diabetes mellitus patients that are hyperglycemic unlike those who are not hyperglycemic (Tonnies et al., 2018). There exists complex relationship of the metabolic syndrome and incidences of stroke in diabetic patients. For instance, researchers report that the metabolic syndrome doubles the risk of stroke though it has little or no effect in recurrent stroke incidences (Mi et al., 2012). The outcomes of stroke are worsened by diabetes just like diabetes worsens the outcomes of coronary artery diseases. For instance, studies have reported that diabetic mellitus significantly worsens the risk of mortality rates increasing in patients with stroke (Mi et al., 2012). Besides, the duration of the condition is important in determining the severity of stroke. Diabetic patients have also been reported to present with higher rates of neurological deterioration relative to patients who are nondiabetic even though strokes can be of the same size and severity. One of the most effective and beneficial treatment for ischemic stroke among diabetic patients has been reported to be thrombolysis (Tonnies et al., 2018).
Peripheral artery disease
This has been strongly associated with diabetes. For instance, various epidemiological surveys have noted that there is a 2-to-4 fold increase in the risk of diabetic patients developing peripheral artery disease (PAD) according to the ankle-brachial index not more than 0.90 (Tonnies et al., 2018). In a trial on the ankle brachial index, a study noted that a good percentage of patients with diabetes mellitus develop PAD relative to a lower percentage of those who are nondiabetic. In fact, the rate of increasing the risk has been noted to be even higher for the risk of suffering from stroke or from CAD (Tonnies et al., 2018). The rate of disease development is also increased in younger patients who are diabetic. Detecting PAD in diabetic patients has been an issue of great concern. There has been association between diabetic mellitus and medical calcinosis (Tonnies et al., 2018). This raises the ankle-brachial index artifactually due to the inability of large arteries to be compressed even though there can be considerable artery occlusive disease besides lowering of the perfusion pressure of the actual ankle. Also, the lower extremity has been note to be severely affected by diabetes mellitus (Hicks and Selvin, 2019). Researchers have noted that diabetic patients that also suffer from PAD are more likely to suffer from neuropathy as well as from the exertional leg symptoms and pain while they resting relative to patients who are nondiabetic (Hicks and Selvin, 2019). The likelihood of pain on exertion as well as the risk of atypical leg pain is increased by diabetes mellitus. Also, studies have also reported that diabetic patients are at a 4-fold risk of amputation at every level of their ankle perfusion pressure relative to patients that are nondiabetic. Being diabetic is further associated with certain conditions that enhance the occurrence of wounds in the foot as well as complications of vascular insufficiency (Tonnies et al., 2018).
Medical Therapy of Diabetes Mellitus and Atherosclerosis
Hypertension
In a study by the UKPDS, they have established that the control of blood pressure to reduces stroke by approximately 44%. Besides, it reduces deaths related to diabetes by 32%. Besides, the study made a comparison of the use of captopril and the use of atenolol as agents against such conditions. No differences in the two were reported from the study. There is need for hypertensive diabetic patients to have their blood pressures lowered as this lowers mortality rates by approximately 14%. Lowering blood pressure has thus remained as a major target for addressing the problems associated with diabetes mellitus and hypertension. The efficacy of RAS inhibitors have been examined for their potential in reducing the atherosclerotic vascular events in diabetic patients. For instance, Ramipril has been reported by researchers to reduce the rates of death, MI cases as well as stroke occurrences amongst diabetic patients. Also, the efficacy of ACEI has also been investigate and has been noted to have a significant cardiovascular risk reduction. In cases where losartan was administered, a substantial decrease in the composite of cardiovascular death alongside myocardial infarction and stroke was reported (Schmidt et al., 2013).
Dyslipidemia
Various studies reported the use of hdroxymethylglutaryl-CoA reductase inhibitors in the treatment of diabetes mellitus. Some trials have made use of simvastatin and a reduction in the rate of myocardial infarction as well as stroke and death were reported (Cavender et al., 2015). Statins have been reported to be effective in the secondary prevention of cardiovascular conditions amongst diabetic patients that also present with history of coronary artery disease. Recent reports also indicate that the administration of statin has been associated with increased incidences of diabetes mellitus. Besides, same studies have associated hypercholesterolemia with a reduction in the prevalence of diabetes mellitus. Reports by researchers have also indicated that the prevalence of type 2 diabetes is lowered in patients that carry apolipoprotein B mutations as well as in patients with low-density lipoprotein receptor mutations relative to those that do have the same effects. These studies thus suggest a link between lipids, lipid receptors, and glucose metabolism (Zaharieva et al., 2017). There is however a limitation on the efficacy of drugs that is lipid lowering on diabetic patients.
Hyperglycemia
The effect of glycemic control on cardiovascular risk reduction has been an area of great unclearity for medical practitioners. Metformin has been noted from the literature review as one of the available hypoglycemic agents and it has been noted to substantially lower the risk of myocardial infarction. Based on a study by the UKPDS, diabetic patients treated with metformin experience a significant reduction in the experiences of MI, 25% death reduction relative to other hypoglycemic agents. In type 1 diabetes patients, intensive glucose control has been noted to lead to reduction of cardiovascular events in a broad spectrum. Intensive treatment has also been noted to reduce the rates of non-serious myocardial infarction, stroke and sometimes death (Cavender et al., 2015). Other hypoglycemic agents have also been reported to have relatively less effect as much as the reduction of cardiovascular events is concerned. For instance, in an investigation of the use of empagliflozin that is a sodium glucose cotransporter inhibitor, an improvement of cardiovascular outcomes was reported (Zinman et al., 2015). Besides, after follow-up activities, reports still noted relative reduction of death from cardiovascular events as well as all-cause death. In stroke, there was no notable increase in outcomes of the patients (Zinman et al., 2015). The use of the medicine has been further linked to reductions in glycohemoglobin, blood pressure, amongst other parameters (Schmidt et al., 2013). Its efficacy indicates that lowering glucose has some level of significance.
Antiplatelet therapy
Experiments have indicated that there is platelet activation in diabetic patients. However, the significance of antiplatelet therapy has not been established where there is no atherosclerosis. Studies examined aspirin in diabetic patients but no benefit has been established. Besides, the importance of drugs that activate the adenosine diphosphate receptor in the quest to prevent of diabetes in patients with no atherosclerosis has not been established. A drug like clopidogrel has been noted to reduce rate of occurrences of vascular death as well as the cases of myocardial infarction and stroke among diabetic patients (Thukkani et al., 2015). The absolute reduction rate of the same has been reported to be 2.1% while the relative reduction date is 12.5% relative to the reduction of 0.9% and 6.1% for absolute and relative reductions respectively for patients suffering from diabetes mellitus (Thukkani et al., 2015). Better results are provided by more potent adenosine diphosphate inhibitors in the acute setting. An example that has been reported in literature includes prasugrel that is more effective than clopidogrel in reducing a composite end point of cardiovascular death alongside nonfatal MI and stroke (Thukkani et al., 2015). The benefit has also been noted to be greater in diabetic patients relative to patients that are nondiabetic. On comparing Ticagrelor and clopidogrel, it is superior (Thukkani et al., 2015).
Smoking cessation
Smoking of cigarette increases the risk of atherosclerotic vascular disease. These are inclusive of myocardial infarction, stroke, and PAD. Besides, studies have reported that ceasing to smoke is linked with reduced adverse effects of cardiovascular events. Ceasing to smoke cigarette also increases the risk of diabetes mellitus. Cigarette smoking has been linked to a synergistic effect as well as insulin resistance leading to atherosclerosis. Thus, it is crucial to aggressively pursue smoking cessation interventions.
Ethical Considerations
In conducting research ethics were considered in research formulation and plan evaluation. This research was conducted in line with all ethical considerations. The content used in this paper is informed, which is a major issue in conducting research. Patient’s rights to autonomy are protected by informed consent as it seeks to incorporate the rights of individuals through self-determination (State, 2010). Participants were made aware of this project, the main purpose and how the results of this study will be used. Informed consent allowed respondents to make informed decisions at whether to participate or not. There was voluntary participation and participants were allowed to freely withdraw anytime (Roberts et al, 2019). Another important ethical issue that was considered by this research was the anonymity and confidentiality. Richards and Schwartz studies on the term confidentiality displayed that in health care professionalism, the term means that no personal information is disclosed except in certain situations. This research did not disclose the names of the participants as well as the patients that were used in conducting research (Clark-Kazak 2017). This research minimized any possibility of intrusion into the autonomy of study participants. Children and other vulnerable individuals should have access to an advocate or an elderly person during data gathering sessions.
CONCLUSION
Type 1 diabetes mellitus causes various vascular complications through different pathological ways, including hyperglycemia and insulin resistance. These vascular complications are divided into two types which are microvascular complications and macrovascular complications. Microvascular complications have long-term complications and generally affect the small blood vessels and include neuropathy, nephropathy, and retinopathy. In contrast, macrovascular complications occur in the coronary arteries, peripheral arteries, and cerebrovasculature. Neuropathy is associated with nerve pathology and is classified according to the affected nerves. It is more prevalent in patients with diabetes with more than 25 years, while it accounts for about 7% in patients within one year. Diabetes mellitus results in various vascular complications through different pathogenesis pathways, such as insulin resistance. The connection between Diabetes and vascular complications is apparent; however, more clinical studies are required to identify the pure effect of DM
References
- Bjornstad, P., Donaghue, K.C. and Maahs, D.M., 2018. Macrovascular disease and risk factors in youth with type 1 diabetes: time to be more attentive to treatment? The Lancet Diabetes & Endocrinology, 6(10), pp.809-820.
- Bressler, S.B., Qin, H., Melia, M., Bressler, N.M., Beck, R.W., Chan, C.K., Grover, S., Miller, D.G. and Diabetic Retinopathy Clinical Research Network, 2013. Exploratory analysis of the effect of intravitreal ranibizumab or triamcinolone on worsening of diabetic retinopathy in a randomized clinical trial. JAMA ophthalmology, 131(8), pp.1033-1040.
- Cavender, M.A., Scirica, B.M., Bonaca, M.P., Angiolillo, D.J., Dalby, A.J., Dellborg, M., Morais, J., Murphy, S.A., Ophuis, T.O., Tendera, M. and Braunwald, E., 2015.
- Vorapaxar in patients with diabetes mellitus and previous myocardial infarction: findings from the thrombin receptor antagonist in secondary prevention of atherothrombotic ischemic events-TIMI 50 trial. Circulation, 131(12), pp.1047-1053.
- Chiang, J.L., Kirkman, M.S., Laffel, L.M. and Peters, A.L., 2014. Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes care, 37(7), pp.2034-2054.
- Clark-Kazak, C. (2017). Ethical considerations: Research with people in situations of forced migration. Refuge: Canada's Journal on Refugees/Refuge: revue canadienne sur les réfugiés, 33(2), 11-17.
- Dabelea D, Stafford JM, Mayer-Davis EJ, D'Agostino R Jr, Dolan L, et al. Association of type 1 diabetes vs. type 2 diabetes diagnosed during childhood and adolescence with complications during teenage years and young adulthood. JAMA. (2017) 317:825–35. doi: 10.1001/jama.2017.0686
- Dabelea D. Diabetes in youth-looking backwards to inform the future: Kelly West Award Lecture
- Diabetes-UK, 2016. List of countries by incidence of type 1 diabetes ages 0 to 14. DiMeglio, L.A., Evans-Molina, C. and Oram, R.A., 2018. Type 1 diabetes. The Lancet, 391(10138), pp.2449-2462.
- Donaghue KC, Marcovecchio ML, Wadwa RP, Chew EY, Wong TY, Calliari LE, et al.
- ISPAD Clinical Practice Consensus Guidelines 2018: Microvascular and macrovascular complications in children and adolescents. Pediatr Diabetes. (2018) 19 Suppl 27:262–74. doi: 10.1111/pedi.127422017. Diabetes Care. (2018) 41:233–40. doi: 10.2337/dci17-0031
- Gan, M.J., Albanese-O’Neill, A. and Haller, M.J., 2012. Type 1 diabetes: current concepts in epidemiology, pathophysiology, clinical care, and research. Current problems in pediatric and adolescent health care, 42(10), pp.269-291.
- Hamman RF, Bell RA, Dabelea D, D'Agostino RB Jr, Dolan L, et al. The SEARCH for diabetes in youth study: Rationale, findings, and future directions. Diabetes Care. (2014) 37:3336–44.d doi: 10.2337/dc14-0574
- Hex, N., Bartlett, C., Wright, D., Taylor, M. and Varley, D.J.D.M., 2012. Estimating the current and future costs of Type 1 and Type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabetic medicine, 29(7), pp.855-862.
- Hicks, C.W. and Selvin, E., 2019. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Current diabetes reports, 19(10), pp.1-8. https://www.diabetes.org.uk/About_us/News_Landing_Page/UK-has-worlds-5thhighest-rate-of-Type-1-diabetes-in-children/List-of-countries-by-incidence-of-Type-1-diabetes-ages-0-to-14/ [Accessed February 2, 2021]. International Diabetes Federation’s Diabetes Atlas. Available at:
- Jaiswal M, Divers J, Dabelea D, Isom S, Bell RA, Martin CL, et al. Prevalence of and risk factors for diabetic peripheral neuropathy in youth with type 1 and type 2 diabetes: SEARCH for diabetes in youth study. Diabetes Care. (2017) 40:1226–32. doi: 10.2337/dc17-0179
- Kelkar, S., 2020. Diabetic Neuropathy and Clinical Practice. Springer.
- Kobyliak, N., Falalyeyeva, T., Mykhalchyshyn, G., Kyriienko, D. and Komissarenko, I., 2018. Effect of alive probiotic on insulin resistance in type 2 diabetes patients: randomized clinical trial. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 12(5), pp.617-624.
- Lee R, Wong TY, and Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis (Lond). (2015) 2:17. doi: 10.1186/s40662-015-0026-2
- Li, J.Q., Welchowski, T., Schmid, M., Letow, J., Wolpers, C., Pascual-Camps, I., Holz, F.G. and Finger, R.P., 2020. Prevalence, incidence and future projection of diabetic eye disease in Europe: a systematic review and meta-analysis. European journal of epidemiology, 35(1), pp.11-23.
- Mi, D., Jia, Q., Zheng, H., Hoff, K., Zhao, X., Wang, C., Liu, G., Wang, Y., Liu, L., Wang, X. and Wang, Y., 2012. Metabolic syndrome and stroke recurrence in Chinese ischemic stroke patients–the ACROSS-China study. PloS one, 7(12), p.e51406.
- Okorie, C., 2018. The role of nurses as educators in preventing the complications of Type 1 Diabetes among young patients: A systematic literature review.
- Piardi, T., Lhuaire, M., Bruno, O., Memeo, R., Pessaux, P., Kianmanesh, R. and Sommacale, D., 2016. Vascular complications following liver transplantation: a literature review of advances in 2015. World journal of hepatology, 8(1), p.36.
- Roberts, L. W., Berk, M. S., & Lane-McKinley, K. (2019). Ethical considerations in research on suicide prediction: necessity as the mother of invention. JAMA psychiatry, 76(9), 883-884.
- Rossing, P. and Frimodt-Møller, M., 2019. Clinical features and natural course of diabetic nephropathy. In Diabetic Nephropathy (pp. 21-32). Springer, Cham.
- Schmidt, M., Johannesdottir, S. A., Lemeshow, S., Lash, T. L., Ulrichsen, S. P., Bøtker, H. E., and Sørensen, H. T. 2013. Obesity in young men, and individual and combined risks of type 2 diabetes, cardiovascular morbidity and death before 55 years of age: a Danish 33-year follow-up study. BMJ open, 3(4), e002698.
- Sivaprasad, S., Gupta, B., Gulliford, M.C., Dodhia, H., Mohamed, M., Nagi, D. and Evans, J.R., 2012. Ethnic variations in the prevalence of diabetic retinopathy in people with diabetes attending screening in the United Kingdom (DRIVE UK). PloS one, 7(3), p.e32182.
- Songini, M., Mannu, C., Targhetta, C. and Bruno, G., 2017. Type 1 diabetes in Sardinia: facts and hypotheses in the context of worldwide epidemiological data. Actadiabetologica, 54(1), pp.9-17.
- Strain, W.D. and Paldánius, P.M., 2018. Diabetes, cardiovascular disease and the microcirculation. Cardiovascular diabetology, 17(1), pp.1-10
- Stratton, I. M., Adler, A. I., Neil, H. A. W., Matthews, D. R., Manley, S. E., Cull, C. A., ... & Holman, R. R. (2015). Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. Bmj, 321(7258), 405-412.
- Suneja, S., Christian, Y. and Chandra, N.C., 2018. Milieu of Diabetes in the 2nd Decade of 21st Century. Journal of Diabetes & Metabolism, 9(09), pp.1-14.
- Thukkani, A.K., Agrawal, K., Prince, L., Smoot, K.J., Dufour, A.B., Cho, K., Gagnon, D.R., Sokolovskaya, G., Ly, S., Temiyasathit, S. and Faxon, D.P., 2015. Long-term outcomes in patients with diabetes mellitus related to prolonging clopidogrel more than 12 months after coronary stenting. Journal of the American College of Cardiology, 66(10), pp.1091-1101.
- Tönnies, T., Stahl-Pehe, A., Baechle, C., Castillo, K., Kuss, O., Yossa, R., Lindner, L.M., Holl, R.W. and Rosenbauer, J., 2018. Risk of microvascular complications and macrovascular risk factors in early-onset type 1 diabetes after at least 10 years duration: an analysis of three population-based cross-sectional surveys in Germany between 2009 and 2016. International journal of endocrinology, 2018.
- Wang, W. and Lo, A.C., 2018. Diabetic retinopathy: pathophysiology and treatments. International journal of molecular sciences, 19(6), p.1816.
- Zaccardi, F., Webb, D.R., Yates, T. and Davies, M.J., 2016. Pathophysiology of type 1 and type 2 diabetes mellitus: a 90-year perspective. Postgraduate medical journal, 92(1084), pp.63-69.
- Zaharieva, D., Yavelberg, L., Jamnik, V., Cinar, A., Turksoy, K. and Riddell, M.C., 2017. The effects of basal insulin suspension at the start of exercise on blood glucose levels during continuous versus circuit-based exercise in individuals with type 1 diabetes on continuous subcutaneous insulin infusion. Diabetes technology & therapeutics, 19(6), pp.370-378.
- Zinman, B., Wanner, C., Lachin, J.M., Fitchett, D., Bluhmki, E., Hantel, S., Mattheus, M., Devins, T., Johansen, O.E., Woerle, H.J. and Broedl, U.C., 2015. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. New England Journal of Medicine, 373(22), pp.2117-2128.
Continue your exploration of Unrecognized Statehood with our related content.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



